Review Article - (2022) Volume 10, Issue 11
Neurologic Manifestations of Post COVID Syndrome
Priya Malik*, V Wagh and Swaroopa Chakole
*Correspondence: Dr. Priya Malik, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India, Email:
Abstract
Respiratory condition COVID-19 pandemic spreads, it is turning out to be progressively apparent that COVID sickness 2019 (COVID-19) isn't restricted to the respiratory framework like difficulty in breathing but different organs can be impacted. Specifically, infection related neurological signs are being accounted for increasingly more oftentimes in like central nervous system autonomic nervous system. Cases of neurological manifestations in patients infected with deadly virus are on the rise, and presentations can be simple like a mild headache to more serious manifestations such as seizure, polyneuropathy, encephalopathy, myopathy and stroke. It can cause post COVID neurological syndrome. It comprises of neurological outcome after COVID-19. Loss of smell, taste, and headache are most frequent symptoms. It can pose serious outcome in persons who are affected with this virus. It has been found that persons who get cured of the virus remain dormant in CNS for a very long time and after sometime this virus is able to restart its CNS manifestations. There are also case of GUILLAIN-BARRE syndrome in person after recovering from COVID-19 it can be confused with post viral fatigue acute COVID-19 symptoms that last more than 6 weeks are tiredness, loss of memory, headache, chronic fatigue syndrome. It is now clear that COVID has an affinity for nervous system through its various manifestations. Post mortem studies of persons who succumbed to this deadly disease have shown virus particles in CSF which surround brain and spinal cord and also in cytoplasm of neocortex and hypothalamus. It also causes degeneration of neuron, cell death.
Keywords
COVID-19, Gullian-barre syndrome, Polyneuropathy, Encephalitis, Stroke, Headache, Fatigue
Introduction
Presently, post COVID syndrome can incorporate manifestations identified with remaining inflammation organ harm, sway on prior ailments or vague impacts because of hospitalization or person who may be requiring mechanical ventilation for long periods of time, that is, post intensive care syndrome. In this aspect it makes sense to focus assessing prognostic markers (blood biomarkers) like C reactive protein, neutrophil lymphocyte proportion, serum ferritin and D dimer. These markers can tell us about morbidity and mortality.
Reports of CNS complaints in COVID-19 patients are on the rise, with presentations varying from a mild headache to more severe manifestations such as seizure, polyneuropathy, encephalopathy, and stroke. Recently, cases of Guillain-Barre Syndrome (GBS) the organism that has lived up to its reputation and truly gone viral, has created a whirlwind in the field of medicine [1].
Dec 2019, in China Hubei first case of COVID-19 was identified and after that disease has spread rapidly, engulfing the entire world, with its high infectivity index. India as of today stands as one of the most affected nations.
The clinical manifestations of this novel infection are heterogeneous. The typical triad at the offset of the pandemic consisted of fever, dry cough, and breathlessness, but with the passage of time, symptoms involving almost all systems have been uncovered and added to the spectrum of COVID-19. The symptoms of COVID-19 can be mild which includes only upper respiratory tract and can be severe as it can cause acute respiratory distress syndrome, multi organ dysfunction, and death. Little is known at this juncture about the pathogenesis and long term sequelae of this mysterious pathogen.
Neurological sequelae can be disastrous which include intra cerebral haemorrhage, encephalitis, loss of smell and taste, strokes which are caused by thrombus occluding vessel. There are even some cases of young age group people with no risk factors developing stroke.
Peripheral neuropathy, myopathy, acute inflammatory demyelinating neuropathy are another example.
After the principal instances of the novel Coronavirus sickness (COVID-19) were accounted for in Wuhan, China, in December 2019, the spread of serious intense respiratory disorder COVID quickly turned into a pandemic, compelling medical services frameworks and state-run administrations across the world to go to outrageous lengths to contain the disease, and at the same time drawing in mainstream researchers in a test of skill and endurance to foster powerful therapies. Study has been done that proof this viral infection can be spread through air droplets, virus has also been identified in stool but mainly it spreads by respiratory route. Not only symptomatic but also persons without any symptoms but infected can spread the virus to other individuals [2,3].
Symptoms of COVID-19 are similar to other viral infections. The most well-known symptoms of COVID-19 are cough without any sputum, fever and rhinorrhoea, git manifestation are not much common [3].
Studies from China have shown that most patients had mild pneumonia (81%) while the rest 19% developed severe respiratory problems, multi organ failure and septic shock [4]. Neurological manifestations occurring one to one eighty days can be intracranial haemorrhage, cerebrovascular disease, Parkinson's disease and Parkinsonism, neuromuscular diseases, peripheral neuropathy, myoneural junction and muscle disease encephalitis, dementia, fatigue, gustatory and olfactory disturbances. Studies have shown that almost 1 in 3 individuals tend to develop neurological problems post COVID. Severely infected individuals mainly develop neurological complications and these manifestations are associated with poor outcome. These are more common in people with previous neurological disorders and person having comorbidities like diabetes mellitus and hypertension and persons who are immune compromised.
Literature Review
Objective
To write a review article on neurological manifestations of post COVID syndrome.
Meaning of post COVID-19 syndrome: Post viral disorders can happen after an infection and are an assortment of manifestations that happen as a reaction to the past viral disease. The most widely recognized manifestation is unexplained exhaustion that keeps on enduring after the infection is as of now not dynamic. What causes these manifestations after viral infection are yet being studied, they are accepted to be the consequence of anomalies in the anxious, resistant, and metabolic frameworks. Post COVID-19 Neurological Syndrome (PCNS) is mainly caused by body immune response and also cerebrum, it as a reality has been affirmed by different clinical experts [5].
Because of a provocative reaction to the COVID-19 infection, proteins like cytokines are produced by the body that affect cell correspondence. COVID-19 infection can cause break in blood brain barrier and eventually it lead to deposition of these cytokines in central nervous system. Sleep cycle, feeding centre that controls appetite, release of hormones, regulation of temperature are affected because of cytokines entering hypothalamus. They can likewise cause intellectual irregularities, as well as serious fatigue. This is the manner by which PCNS can cause long haul impacts even after the dynamic disease has passed. At times, these indications might prompt long haul unexpected problems, for example, heart attack, stroke, lung pathology, and persistent exhaustion or Myalgia Encephalomyelitis (ME) [6].
Relationship between COVID-19 and neurological complications has been noticed. COVID-19 can cause long term sequelae. Surveys at present reported an association between COVID-19 and neurological inadequacies, communicating that individual who was treated with COVID-19 were at higher risks of cognitive loss and intellectual impairment [7].
Viral encephalitis, systemic inflammation, cerebrovascular changes, and organ dysfunction leads to brain injury. And these are the reason for neurological complication during a COVID-19 disease, they can likewise prompt long haul neurological outcomes, for example, disturbing a current neurological condition or starting another one. Person who is less severely affected by COVID 19 also complains of prolonged symptoms like fatigue, dizziness, smell and taste issues, and myalgia.
Therefore, data collection and research are important for diagnostic and therapeutic intervention. And also, how to avoid this neurological manifestation and to know who are at greater risk of these manifestations.
PCNS include myopathy, an effect on mind set causing depression and anxiety, fatigue, brain fog, concentration problems, headache, cognitive decline. Studies have confirmed that vast majority of people that is ninety seven percent people have also shown features suggestive of Post-Traumatic Stress Disorder (PTSD) [8].
Studies show that PCNS can manifest in the form of prolonged muscle weakness and myopathy in some survivors [9]. Neurological symptoms can occur in central nervous system and the peripheral nervous system. In early months of COVID-19, doctors keep focusing only on respiratory system like here breathing problems but soon neurological symptoms start to come in the limelight. Some patients show delirium, confusion, agitation (Figure 1).
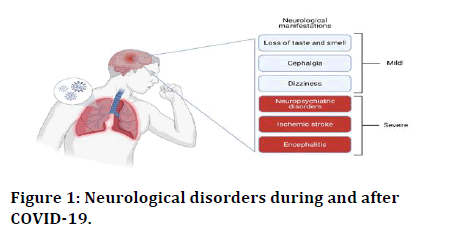
Figure 1: Neurological disorders during and after COVID-19.
Neurological disorders during and after COVID-19 are illustrated in the figure below.
How COVID 19 affects brain: Viruses can infect the brain but how novel Corona virus does it is not very clear. It can be either due to inflammation or over stimulation. Polymerase chain reaction despite its high sensitivity and specificity is not able to detect virus particles in CSF that is contained in the brain ventricles and the cranial and spinal subarachnoid spaces.
Cause for that can be ACE 2 is protein that virus particle use for entry is not much expressed in brain cells. ACE 2 receptors expressed on cells to regulate blood pressure. Virus uses it as route of entry. Studies have shown that various neurological manifestation of COVID-19 is due to body immune response rather than virus invading brain [10].
In cerebrospinal fluid surrounding brain and spinal cord, changes in immune function have also seen. This includes presence of antibodies which are formed against virus they react with nervous system. There is a cascade of events starting from inflammation, capillary endothelitis, as a result blood brain barrier is broken and further it causes pro-inflammatory cytokine cascade [11,12].
Also, there is a hyper coagulable state formed via mechanisms of thrombosis and inflammatory states [13,14]. ACE 2 is expressed on type two pneumocystis. It is also expressed on glial cells and astrocytes. Therefore, astrocytic marker of brain injury that is glial fibrillary acidic protein is increased in persons with neurologic manifestations, other neuronal injury marker is neuro filament light chain protein these both markers are increased in acute phase only and in patients who were critically ill requiring hospitalization, mechanical ventilation, oxygen therapy. On follow up biomarker values are usually within normal limits [15].
Discussion
Mechanism of neurological complication: Mechanism is diverse and multifactorial.
It includes:
• Neurologic injury from systemic dysfunction it caused post hypoxic encephalopathy and encephalopathy due to metabolic derangement.
• Renin angiotensin system dysfunction.
• Immune dysfunction, it includes pro inflammatory state which causes cytokine storm, coagulopathy, and capillary endothelitis. Para infectious and post infectious triggers that cause GBM and ADEM
• Direct viral invasion of nervous system by olfactory, vagal, neurotropism, transcytosis, endocytosis, Tran’s synaptic transmission [16].
Risk factors for more serious COVID-19 infections in patient with pre-existing neurological disorder
• Age more than 60 years
• Swallowing or breathing difficulties
• Person on immunosuppressant
• Pre-existing neurological disorder
• Comorbidities like diabetes mellitus hypertension
• Immuno compromised
• These all persons can in one study also get prolonged COVID
Various neurological manifestations
Smell and taste disorders: In prolonged COVID, patient can suffer from anosmia and dysgeusia even half a year after symptom onset. Though its mechanism is not fully understood. In some people even after a year they have not acquired an ability of smell and taste some research has led to conclusion that virus gains entry through olfactory bulb. This virus also causes congestion of nasal mucosa. Smell and taste disorder more common among female gender and among people who does not smoke.
Sometimes it can be an only and first presenting symptom of virus infection. One study was done thirty percent of impacted patients who had recuperated olfactory capacity mean manifestation of length was eight days [17,18].
Chronic fatigue syndrome/myalgia encephalitis: Fatigue is most common reported symptom. Extreme intense respiratory disorder COVID 19 (SARS-CoV-2) can cause constant and intense infection. Post-Acute Sequelae of SARS-CoV-2 (PASC) incorporate injury to the lungs, heart, kidneys, and mind that might create an assortment of side effects [19].
PASC likewise incorporates a post Covid sickness 2019 (COVID-19) disorder ('long COVID') with highlights that can follow other intense irresistible illnesses and myalgia encephalomyelitis/on-going weariness condition [20].
Encephalopathy: Persons suffering from COVID at any point of time either in acute stage or sub-acute stage has suffered from delirium and problem with consciousness. Its mechanism is same as other neurological manifestation that is interaction of virus and ACE 2 receptor it leads to neuronal damage and interleukin are high [21,22].
It is associated with poor outcome. And commonly found in critically ill patient. All have variable neurologic findings. Person can also exhibit delirium, agitation and decreased level of consciousness [21].
Often it is associated with poor outcome. Examples are acute demyelinating encephalomyelitis, necrotizing encephalitis. Neuroimaging demonstrate hyper intensity in median temporal lobe, multifocal white matter lesion in flair. Haemorrhage in white matter may be seen. More common in patients who are admitted.
Cerebrovascular disease: Risk of stroke varies according to the severity of illness. During this pandemic time patient coming with stroke like symptom should be checked for COVID test. Mostly stroke occurs 1-3 weeks after onset of COVID-19 symptoms but can be initial presentation also. Stroke can be ischaemic or haemorrhagic in type. Stroke commonly found in these patients is generally of ischemic type and mainly were present in elderly males [23].
The outcomes portrayed are mostly identified during the hospitalization for acute treatment. Patients who became critically ill eventually died. There have also been incidences of young people in their 20's and 30's who have no other stroke risk factors suffering from cerebrovascular disease during or post COVID infection.
Mortality is higher in people who contract COVID-19 along with stroke rather than only stroke. Patients suffering from stroke as a complication of COVID-19 disease can also develop kidney injury because of deranged coagulation profile. Use of intravenous thrombolytic agents should be done cautiously after proper coagulation profile check-up [24].
Facial nerve palsy: It can be a late CNS manifestation. The facial nerve palsy in which the face becomes crooked and the facial muscles get paralyzed, either on one side or both sides. Sometimes, the muscles which enable eye ball movement also get affected which causes double vision, difficulty to open and close eyelids and takes a while to recover with treatment. It can be a only presenting symptom and can occur after some time of infection [25,26].
Neuromuscular disease: GBS associated with COVID-19 infection has low incidence rates. Acute Inflammatory Demyelinating Polyneuropathy (AIDP) is more prevalent than other variants. COVID-19 GBS seems to be more severe than non COVID-19 GBS. Cerebrospinal fluid study and electro diagnostic studies are usually unremarkable [27].
Though it is rare, its long term sequelae are devastating and are associated with poor outcome. It can present as weakness in lower extremities to a more severe presentation of swallowing and difficulty problems. The reason for developing neuropathy is infection that led to strong immune reaction following which there is a cascade of pro inflammatory cytokine [27]. In early phase it is important to identify its signs and symptoms and accordingly referral should be made to a proper tertiary care institute [28].
Diagnosis of GBS requires electromyography and presence of anti-ganglioside antibodies. Other examples are peripheral nerve injuries that occur mainly after prone positioning mostly of lower trunk, myositis, fatigue, myalgia are also other common examples. There can be also hydroxyl chloroquine, dexamethasone, azathioprine induced neuropathy or myopathy.
Seizures: Prevalence of seizures in COVID PTS is around 4.1% patients infected with virus mainly develop acute cerebrovascular disease. Seizures occur due to the virus invading the central nervous system but it can also occur due to less oxygen supply to brain that is, hypoxia caused by severe respiratory involvement, for example as seen in pneumonia. The virus gains entry and trigger activation of many pro inflammatory cytokines that cause depolarization of neuron. This causes metabolic changes and induces status [29]. Persons having history of status epilepticus have more poorer outcome because in these patients, the frequency and intensity of seizures increase [30].
COVIDosomnia: It can include both excess sleep and less sleep. Not only those who recovered from deadly virus but also other people have been noticing significant changes in their sleep pattern. They fear about getting the infection, worry about friends and family, not having the option to go to work, not having social contact with others, and the worry of loss of loved one or financial issues because of not going to work haunts them. Some of them meet the criterion for constant sleep deprivation; not having the option to nod off for even 30 minutes multiple times each week for over a period of 3 months or more [31].
Critical illness polyneuropathy/myopathy: Seen in patient who have long hospital stay. COVID infection can infiltrate the brainstem via trans synaptic route. Being female and who require oxygen therapy, mechanical ventilation, developed sepsis, hyperglycaemia is at higher risk [32].
Microcirculation of the central nervous system and peripheral nervous system is changed by free radicals, inflammatory markers, cytokines they mainly decrease nutrient and oxygen availability. Critically illness myopathy mainly develops in patients who are critically ill [33]. Mechanism of CIM is complex as it includes mitochondrial dysfunction, metabolic alteration and excitation contraction coupling is also not normal [34].
Brain fog: Many months after a person has recovered from COVID infection, there can be persisting cognitive complaints. These complaints are called ‘brain fog’. In one patient it was also seen in an acute setting with their cerebrospinal fluid biomarkers highly suggesting Alzheimer’s disease. Brain fog may persist beyond one year. It is an umbrella term for cognitive impairment which includes confusion, loss of memory, difficulty in concentration, dizziness. It is more common in patient who become critically ill and requires mechanical ventilation ICU admission and in female gender [35].
Headache: Some patients unluckily don’t completely recover from deadly Coronavirus infection. They continue to experience post COVID manifestations. One such example is headache occurring in acute phase of post COVID is almost similar to migraine and tension like headache especially in its chronicity. Headache should be differentiated from migraine as a person with preexisting migraine have increased frequency, long lasting COVID headache, delayed onset COVID headache and post COVID headache or even headache associated with many other symptoms (such as loss of sleep, loss of memory, dizziness, fatigue, etc.) to identify as “post COVID-19 syndrome” [36].
Conclusion
The current pandemic is still going on. It is difficult to explain the full clinical picture of post COVID neurological manifestations but neurological complications caused by COVID 19 are frequent and increase mortality by mechanisms are yet unclear. But the affinity of COVID-19 virus for nervous system can’t not be denied after seeing its various neurological manifestations. There should be strict control of metabolic alterations and cardiovascular danger factors, powerful and safe treatment are a current test all through the pandemic. The recovery in these patients is a task. This is because of impediments produced by multi organ harm.
Various neurological manifestations also appear to depend on the level of infection. Neurological manifestations are mild in people who are less severely affected by virus and severe symptoms of CNS are noted in people who become critically ill by virus.
There should be proper management and early identification of persons with neurological manifestations post COVID.
References
- Vitalakumar D, Ankita Sharma, Anoop Kumar, et al. Neurological manifestations in COVID-19 Patients: A meta-analysis. ACS Chem Neurosci 2021; 12:2776-2797.
- Zou L. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 329:1177–1179.
- Gomes C. Report of the WHO China joint mission on Coronavirus disease 2019 (COVID-19). Braz J Implantol Health Sci 2020; 2.
- Zhang H, Penninger JM, Li Y, et al. Angiotensin Converting Enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med 2020; 46:586–590.
- Wijeratne T, Crewther S. Post COVID 19 Neurological Syndrome (PCNS); A novel syndrome with challenges for the global neurology community. J Neurol Sci 2020; 419:117179.
- Kahouty. COVID-19 and the Brain: Post COVID-19 Neurological Syndrome (PCNS). 2020.
- Heneka MT, Golenbock D, Latz E, et al. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alz Res Therapy 2020; 12:69.
- Bo H-X, Li W, Yang Y, et al. Post-traumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med 2020; 1–2.
- Chan K, Zheng J, Mok Y, et al. SARS: prognosis, outcome and sequelae. Respirol 2003; 8:6–40.
- Micheal Marshall. How COVID-19 can damage the brain. Nature 2020; 585:342-343.
- Najjar S, Najjar A, Chong DJ, et al. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuro inflammation 2020; 17:231.
- South K, McCulloch L, McColl BW, et al. Preceding infection and risk of stroke: An old concept revived by the COVID-19 pandemic. Int J Stroke 2020; 15:722-732.
- Wang T, Chen R, Liu C, et al. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol 2020; 7:e362–e363.
- Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost 2020; 18:1747–1751.
- Virhammar J, Naas A, Fallmar D, et al. Biomarkers for central nervous system injury in cerebrospinal fluid are elevated in COVID-19 and associated with neurological symptoms and disease severity. Eur J Neurol 2021; 28:3324-3331.
- Newman N. Bradley and Daroff's neurology in clinical practice, 8th edition, Elsevier. 2021; 2.
- Petrocelli M, Cutrupi S, Salzano G, et al. Six month smell and taste recovery rates in coronavirus disease 2019 patients: A prospective psychophysical study. J Laryngol Otol 2021; 135:436-441.
- Lechien JR, Chiesa Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild to moderate forms of the Coronavirus disease (COVID-19): A multicentre European study. Eur Arch Otorhinolaryngol 2020; 277:2251.
- Pilotto A, Cristillo V, Cotti Piccinelli S, et al. Long term neurological manifestations of COVID-19: prevalence and predictive factors. Neurol Sci 2021; 42:4903-4907.
- Komaroff AL, Lipkin WI. Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of post-acute COVID-19 syndrome. Trends Mol Med 2021; 27:895-906.
- Panda PK, Sharawat IK, Panda P, et al. Neurological complications of SARS-CoV-2 infection in children: A systematic review and meta-analysis. J Trop Pediatr 2020.
- Nuwer MR. Alpha coma in COVID encephalopathy. Clin Neurophysiol 2021; 132:202-203.
- Fraiman P, Godeiro Junior C, Moro E, et al. COVID-19 and cerebrovascular diseases: A systematic review and perspectives for stroke c management. Front Neurol 2020; 11:574694.
- Trejo JM, Galan G. Stroke as a complication and prognostic factor of COVID-19. Neurologia 2020; 35:318–322.
- Zammit M, Markey A, Webb C. A rise in facial nerve palsies during the Coronavirus disease 2019 pandemic. J Laryngol Otol 2020; 134:905-908.
- Codeluppi L, Venturelli F, Rossi J, et al. Facial palsy during the COVID-19 pandemic. Brain Behav 2021; 11:01939.
- Hussain F, Eldeeb M, Blackmore D, et al. Guillian Barre syndrome and COVID-19: possible role of the cytokine storm. Autoimmun Rev 2020; 19:102681.
- Toscano G, Palmerini F, Ravaglia S, et al. Guillain–Barre syndrome associated with SARS-CoV-2. N Engl J Med 2020; 382:2574-2576.
- Asadi-Pooya AA. Seizures associated with Coronavirus infections. Seizure 2020; 79:49-52.
- Lahiri D, Ardila A. COVID-19 pandemic: A neurological perspective. Cureus 2020; 12:e7889.
- Jing Qi, Jing Xu, Bo-Zhi Li, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med 2020; 72:1–4.
- Yang T, Li Z, Jiang L, et al. Risk factors for intensive care unit acquired weakness: A systematic review and meta-analysis. Acta Neurol Scand 2018; 138:104–114.
- Vanhorebeek I, Latronico N, Van den Berghe G. ICU acquired weakness. Intensive Care Med 2020; 46:637–653.
- Zhou C, Wu L, Ni F, et al. Critical illness polyneuropathy and myopathy: A systematic review. Neural Regen Res 2014; 9:101–110.
- Hugon J, Msika EF, Queneau M, et al. Long COVID: cognitive complaints (brain fog) and dysfunction of the cingulate cortex. J Neurol 2021; 18:1-3.
- Caronna E, Alpuente A, Torres Ferrus M, et al. Toward a better understanding of persistent headache after mild COVID-19: Three migraine like yet distinct scenarios. Headache 2021; 61:1277–1280.
Author Info
Priya Malik*, V Wagh and Swaroopa Chakole
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, IndiaCitation: Priya Malik, V Wagh, Swaroopa Chakole, Neurologic Manifestations of Post COVID Syndrome, J Res Med Dent Sci, 2022, 10 (11): 098-103.
Received: 16-Sep-2022, Manuscript No. JRMDS-22-65466; , Pre QC No. JRMDS-22-65466(PQ); Editor assigned: 19-Sep-2022, Pre QC No. JRMDS-22-65466(PQ); Reviewed: 03-Oct-2022, QC No. JRMDS-22-65466; Revised: 17-Nov-2022, Manuscript No. JRMDS-22-65466(R); Published: 28-Nov-2022
