Research - (2021) Volume 9, Issue 5
One Year Follow-Up Study of Acute and Transient Psychosis with Specific Focus on Cultural Factors Influencing the Course and Outcome
C Prarthana Saraswathi and S Nambi*
*Correspondence: S Nambi, Department of Psychiatry, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Patients and family members supernatural and religious beliefs with diagnosis of acute and transient psychotic disorder were assessed through a course of one year. Almost all the patients and family members had sought magic religious treatments prior to psychiatric treatment and had high supernatural beliefs in the form of sorcery/ witchcraft/, evil spirits, ghosts, planetary influences, divine wraths and karma and low beliefs in stress and chemical imbalance as the cause of illness. An acute (within 2 weeks) onset in all the cases; presence of typical syndromes which are described as rapidly changing, variable, polymorphic states, and typical schizophrenic symptoms; evidence for associated acute stress in a substantial number of cases and complete recovery in most cases within 2 -3months.To assess the knowledge and attitude towards mental illness of the patients and the caregivers in Acute and Transient Psychotic Disorder. To assess the Magico Religious beliefs in relationto the abnormal behavior and the influence of karma in Acute and Transient Psychotic Disorder. To assess the stability of diagnosis of Acute and Transient Psychotic Disorder at the end of one year follow up. The belief in supernatural causation of the illness reins high even at the end of one year follow up. This calls for greater community and patient level education about the cause and treatability of psychiatric disorders.
Keywords
Supernatural and religious, Polymorphic states, Schizophrenic, Psychotic disorder
Introduction
Acute and transient psychosis includes a severe but a heterogeneous presentation of psychiatric disturbance which is associated with considerable distress not only to the patient, but also among the family members and the society in general [1-3]. Social and cultural factors have quite an influence on the management of psychiatric disorders. Culture not only influences the presentation of psychiatric disorders, but also how the disorder is conceptualized in the society, and what remedies are considered beneficial [4,5]. Early appropriate treatment of acute psychosis is associated with better outcomes. Conversely, delays due to social and cultural factors may lead to poorer prognosis among patients with acute psychosis. Belief systems in the Indian society are likely to influence the treatment of patients with acute psychosis. Traditional healers are often resorted to in cases of behavioral disturbances, purportedly to pacify the supernatural powers [6-8].
India is a diverse country with varying cultures and sub-cultures across different geographical regions. Hence, the methods of treatment for psychiatric disturbances may vary from one region to another. Previous literature has attempted to document the characteristics and experiences of traditional and temple healing in south India. However, no study has explicitly attempted to assess religious coping and its association with traditional religious healing in the south Indian population [9-15]. Hence, the present study aimed to understand the religious treatment for acute psychosis in the clinical population in south India, and to find its association with religious coping and supernatural belief systems. We also attempted to find out the religious coping and belief systems of family members of patients with acute psychosis, as they are often the driving force for religious healing for the observed behavioral disturbances.
Materials and Methods
The Outpatient and Inpatient of Department of Psychiatry, Sree Balaji Medical College and Hospital, Chromepet. Type of the study is Longitudinal, Questionnaire based.63 patients along with their family members. One year follow up study, Patients were enrolled in the study from Feb 2015 onwards and were followed up till the end of one year.
Refusing informed consent.
Agitated or clinically unstable patients.
Previous psychotic episodes.
Methodology of the study
The patients and the family members were recruited as dyads in the study after obtaining the Institutional Ethical Committee approval.
The patients who fulfilled the inclusion and the exclusion criteria and diagnosed of having Acute and Transient Psychotic disorder were included in the study after obtaining informed consent.
The participants were administered a preform a constructed to elicit the socio demographic and clinical details. Information was gathered about the age, gender, educational level and occupational status of the participants. The selfreported religion, type of family and residential background was recorded. Information was also gathered about the source of referral to the hospital and details of previous religious treatment. Socio economic status was assessed using the modified Kuppuswamy scale.
Brief Psychiatric Rating scale (BPRS) was used to assess for the severity of psychotic symptoms. Brief Religious Coping (RCOPE) questionnaire was used to assess for religious coping among patients and their family members. An adapted version of the Magico Religious beliefs questionnaire was used to assess for culturally based beliefs of the patients and the family members towards the psychiatric illness. In addition, Hamilton Depression Rating Scale (HAM-D), Young Mania Rating Scale (YMRS), Global Assessment of Functioning (GAF) scales were also administered.
Detailed interviews were done with the caregivers to understand the procedures of faith healing treatment during the onset of the illness, and it was recorded as per verbatim for ease of classification. Since many patients were recommended sacred thread/amulets, clinical photographs of these were also obtained after getting additional consent. The patients and the caregivers were followed up at 1 month, 3 months, 6 months, 9 months and at the end of one year of the illness.
All the scales which were administered during the first visit were re administered during the follow up visits. The data was analysed by using SPSS version 16(IBM Corp, TX) by descriptive analysis. The correlation between the socio demographic, clinical details with severity of psychotic symptoms, religious coping and magico religious beliefs were studied. A P value of less than 0.05 was considered as significant. Qualitative data relating to faith.
Results and Discussion
Socio demographic and clinical characteristics of the patients
About 63 patients who fulfilled the diagnosis of Acute and Transient Psychotic Disorder were included in the study. The mean age of the sample was 23.9years (±6.3). About 61.9% of the study participants were females and the remaining 38.1% weremales.17.5% of the Study participants were educated upto primary school, 31.7% had completed upto 11 th or 12thstd, 22.2% were graduated.31.7% of the study participants were employed and 68.3% of the patients were unemployed. Majority of the study population belonged to Hindu religion -76.2%, followed by Christian religion-14.3% and Muslim religion-9.5%.
57.1% of the study population were from a nuclear family, 42.9% belonged to joint family. 47.6% of the participants resided in a semi urban area, 28.3% from anurbanareaand23.8%werefr omruralarea.61.9% of the patients belonged to the lower middle socio-economic class, 14.3% from lower and middle socio economic class, 9.5% from upper middle socio economic class (Table 1 and Table 2).
| Variable | N % | |
|---|---|---|
| Age | 23.9 (±6.3) | |
| Gender | Male | 24 (38.1%) |
| Female | 39 (61.9%) | |
| Nil | 11 (17.5%) | |
| Education | First to10th Standard | 18 (28.6%) |
| 11th to 12th Standard | 20 (31.7%) | |
| / Diploma | ||
| Graduation and above | 14 (22.2%) | |
| Occupation | Employed | 20 (31.7%) |
| Not employed | 43 (68.3%) | |
| Religion | Hindu | 48 (76.2%) |
| Christian | 9 (14.3%) | |
| Muslim | 6 (9.5%) | |
| Family | joint | 27(42.9%) |
| Nuclear | 36 (57.1%) | |
| Residence | Rural | 15 (23.8%) |
| Semi urban | 30 (47.6%) | |
| Urban | 18 (28.6%) | |
| Socio-economic status | Lower | 9 (14.3%) |
| Lower middle | 39 (61.9%) | |
| Middle | 9 (14.3%) | |
| Upper middle | 6 (9.5%) | |
Table 1: Socio demographic characteristics of the patients.
| Variable | Temple | Dargah | Church | |
|---|---|---|---|---|
| (n %) | (n %) | (n %) | ||
| Age of patient | Mean | 24.3 | 24.1 | 25.2 |
| Range | 16 to 40 | 17 to 40 | 16 to 40 | |
| Patient’s gender | Male | 16 (33.3%) | 10 (30.3%) | 11 (35.50%) |
| Female | 32 (66.7%) | 23 (69.70%) | 20 (64.50%) | |
| Referred by | Relatives | 41 (85.4%) | 16 (48.50%) | 20 (64.50%) |
| Neighbours | 5 (10.4%) | 13 (39.40%) | 10 (32.30%) | |
| Friends | 2 (4.2%) | 4 (12.1%) | 1 (3.2%) | |
| Duration of treatment in days | Median | 3.5 | 1 | 2 |
| Range | 1 to 20 | 1 to 7 | 1 to 14 | |
| Stay in the setting | 36 (75.0%) | 17 (51.50%) | 23 (74.20%) | |
| Duration of stay in days | Median | 2 | 3 | 2 |
| Range | 1 to 14 | 1 to 5 | 1 to 14 | |
| Amount spent | Median | 10,000 | 2,000 | 2,000 |
| Range | 1,500 to 50,000 | 0 to 15,000 | 500 to 5,000 | |
| Adverse consequences | 14 (29.2%) | 12 (36.40%) | 9 (29.0%) | |
Table 2: Religious treatment in various setting.
The mean score for positive religious coping for the patients was 26.0 (standard deviation of 2.2) while the mean negative religious coping score was 24.5 (standard deviation of3.4). Likewise, the mean positive and negative religious coping scores for family members were 25.4 and 23.5 respectively (standard deviations of 2.6 and 3.9 respectively). The patients and their family members concurred in descending order in terms of wondering whether the church had abandoned him, asked forgiveness for sins, and questioned God’s love. Other items for which the patient and family members concurred were deciding the devil made this happen, sought help from God in letting go of my anger, wondered whether God had abandoned, wondered what he/she did for God to punish, focused on religion to stop worrying about problems, tried to put plans into action together with God, and felt punished by God for lack of devotion. The correlation of patient’s and family member’s positive coping (r=0.463, p<0.001) and negative coping (r= 0.649, p<0.001) was significant (Figures 1 to Figure 9).
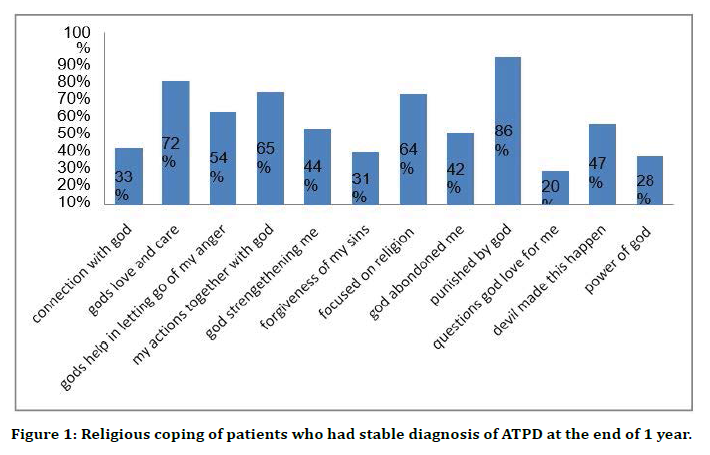
Figure 1. Religious coping of patients who had stable diagnosis of ATPD at the end of 1 year.
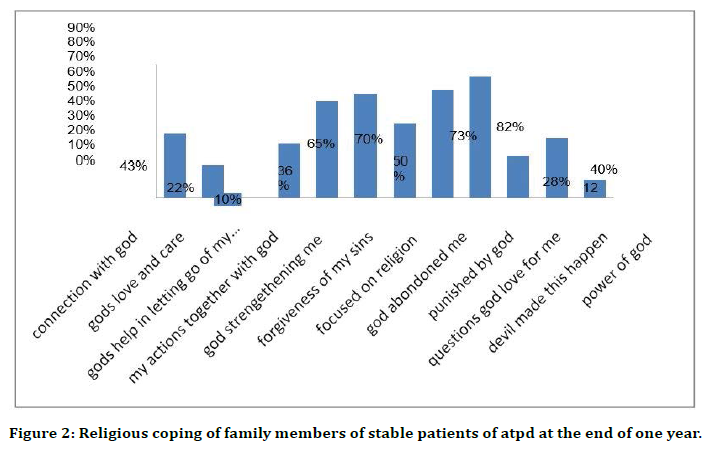
Figure 2. Religious coping of family members of stable patients of atpd at the end of one year.
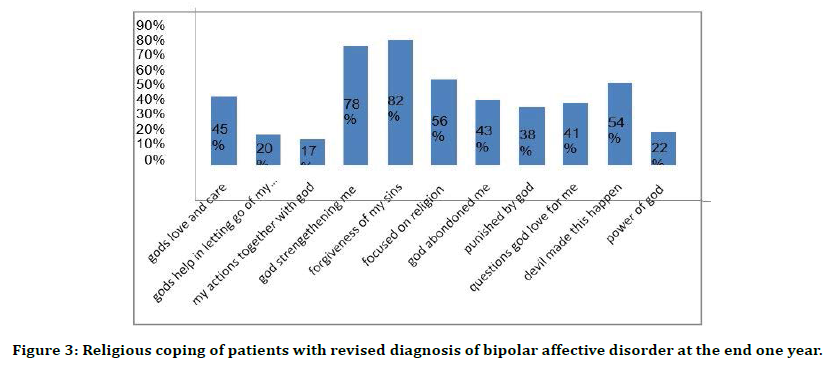
Figure 3. Religious coping of patients with revised diagnosis of bipolar affective disorder at the end one year.
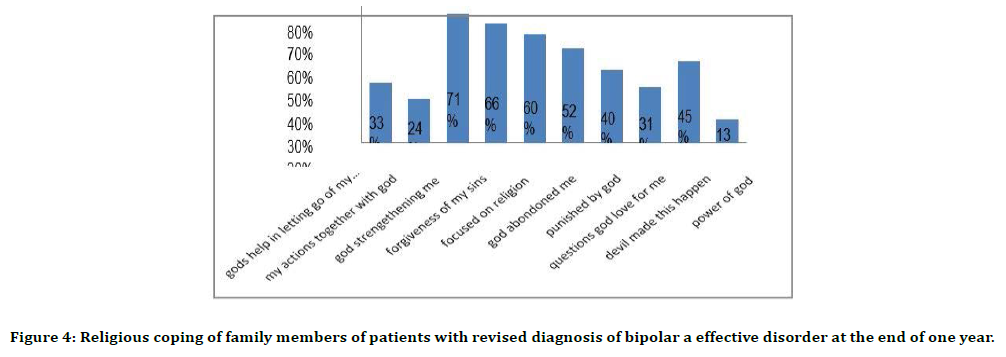
Figure 4. Religious coping of family members of patients with revised diagnosis of bipolar a effective disorder at the end of one year.
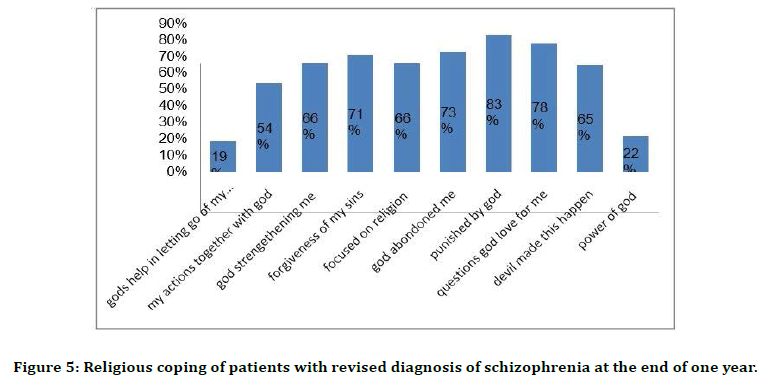
Figure 5. Religious coping of patients with revised diagnosis of schizophrenia at the end of one year.
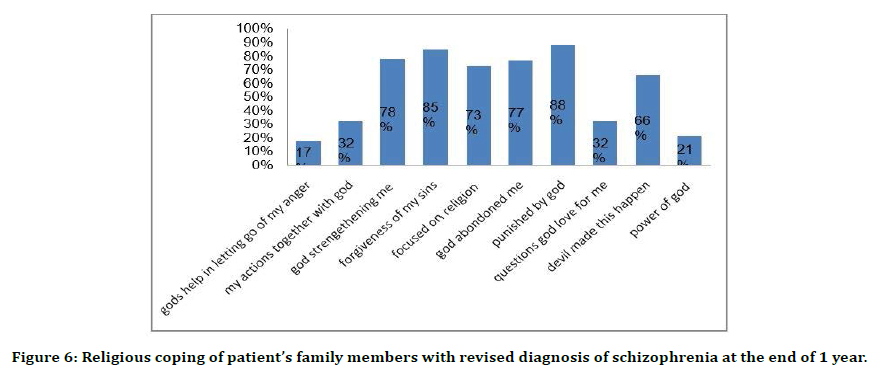
Figure 6. Religious coping of patient’s family members with revised diagnosis of schizophrenia at the end of 1 year.
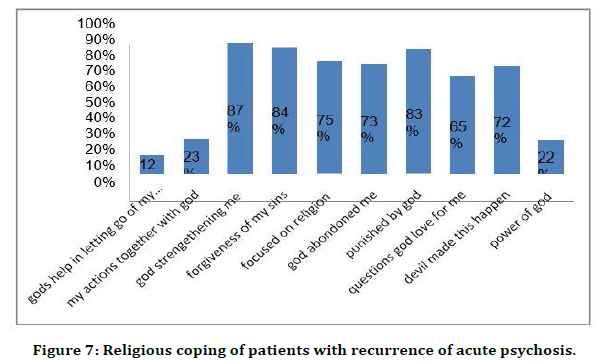
Figure 7. Religious coping of patients with recurrence of acute psychosis.
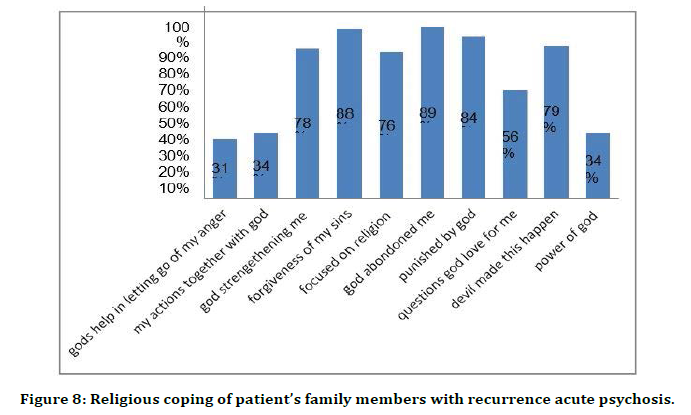
Figure 8. Religious coping of patient’s family members with recurrence acute psychosis.
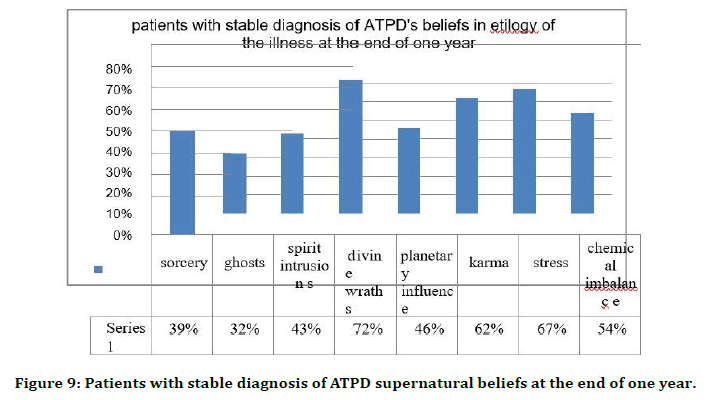
Figure 9. Patients with stable diagnosis of ATPD supernatural beliefs at the end of one year.
Patient’s supernatural beliefs prior the psychiatric treatment showed that 87.3% of the patients had beliefs in sorcery/witchcraft, 95.2% in ghosts, and spirit intrusions.87.3% of the patients believed insorcery and witchcraft as the etiology of the illness, 95.2% in ghosts as the etiology, 93.7% in spirit intrusions as the etiology, 74.6% in divine wraths, 63.5% in planetary influences, 71.4% in karma as the etiology of illness, 42.9% in stress as the cause of illness, 25.4% in stress as the aetiology of the illness. 93.7% of the patients believed that only prayers could lead to improvement in symptoms, 96.8% believed that only magic religious resorts will help in the treatment of the illness. Family members of the patients’ supernatural beliefs were assessed, the data showed that 87.3% believed in sorcery/witchcraft, 95.2% in ghosts, 96.8% in spirit intrusions [15-17].
92.1% of the family members believed in sorcery as the aetiology of the illness,93.7% in ghosts as the cause of illness, 92.1% in spirit intrusions, 82.5% in divine wraths as etiology of illness, 63.5% in planetary influences, 68.3% in karma as the cause of illness, 33.3% in stress as the cause of illness, 30.2% in chemical imbalance. 93.7% of the family members believed that only prayers and magic religious resorts can lead to improvement of illness. The one year follow up data suggested that 8 patients (12.7%) of the sample were re-classified to a diagnosis of schizophrenia 5 patients (7.9%) of the sample had a change in diagnosis to bipolar affectivedisorder.3(4.8%) of the sample had a recurrence of acute psychosis. 37 patients (58.73%) had maintained a stable diagnosis of acute and transient psychotic disorder at the end of one year. 10 patients (15.87%) of the study sample had dropped out during the study Stability of diagnosis of acute and transient psychotic disorder has been researched in may follow up studies. The data given by the Madras longitudinal Study 75% were asymptomatic at the end of 10 years of follow up.
In a comparative study- Roscommon Family Study, acute and transient psychotic disorders follow up- 26.2% were diagnosed to have schizophrenia and 17.6% were diagnosed to have bipolar disorder. Affective disorders and psychotic disorders had some overlap of symptoms.
Acute and transient psychotic disorder as a third psychosis, in his study 12.6% had been diagnosed to have schizophrenia at the end of 4 year follow up. Similar results had been obtained in their follow up study of acute and transient psychosis. These results data are in thesame line of results in the study that we had conducted [18,19].
At the end of one year follow up of the patients who had stable diagnosis of acute and transient psychotic disorder, the supernatural beliefs and religious coping were re assessed. The belief in sorcery/witchcraft was 39%, in ghosts 32%, spirit intrusions 43%, divine wraths 72%, planetary influence 46%, karma 62 %, stress 67%, chemical imbalance54%. The patient’s family members beliefs were assessed and the results showed that 28% believed in sorcery, 39% in ghosts, 34% in spirit intrusions, 66% in divine wraths, 30% in planetary influences, 52% in karma,49% in stress and 62% in chemical imbalance.
Patients supernatural and religious beliefs with revised diagnosis of Bipolar affective disorder at the end of one year were, 77% in sorcery/witchcraft, 78% in ghosts, 71% in spirit intrusions, 67% in divine wraths,29% in planetary influence,36% in karma,43% in stress and 53% in chemical imbalance [20].
Patients’ family members beliefs at the end of one year were, sorcery 69%, ghosts70%, spirit intrusions 73%, divine wraths 64%, planetary influence 51%, karma 63%, stress 58%, chemical imbalance53%. Patients supernatural beliefs with revised diagnosis of schizophrenia was, sorcery/ witchcraft 73%, ghosts 79%, spirit intrusions 81%, divine wraths65%, planetary influence 62%, karma 66%,stress 25%, chemical imbalance 25%.
Patients’ family members supernatural beliefs were ghosts 79%, spirit intrusions 84%, divine wraths 81%, planetary influence76%, karma 68%, stress 39%, chemical imbalance 36% [21,22].
Patient’s supernatural beliefs with diagnosis of relapse of acute psychosis were sorcery 88%, ghosts 89%, spirit intrusions 92%, divine wraths 87%, planetary influence 85%, karma 84%, stress 22%, and chemicalimbalance14%. Patients’ family members supernatural beliefs were sorcery 89%, ghosts 91%, spirit intrusions 88%, divine wraths95%, planetary influence 82%, karma 88%, stress 13%, chemical imbalance13% [23].
There is significant reduction in certain areas of supernatural beliefs though a few areas remain high. The patients and family members of patients with stable diagnosis of acute and transient psychotic disorder have high beliefs in stress and chemical cause as the etiology of the illness at the end of one year in comparison with the other groups (schizophrenia, relapse of psychosis). Relapse of acute psychosis episode patients and family members supernatural and religious beliefs remained to be high even in the subsequent episode.
Conclusion
Patients and family members supernatural and religious beliefs with diagnosis of acute and transient psychotic disorder were assessed through a course of one year. Almost all the patients and family members had sought magic religious treatments prior to psychiatric treatment and had high supernatural beliefs in the form of sorcery/witchcraft/, evil spirits, ghosts, planetary influences, divine wraths and karma and low beliefs in stress and chemical imbalance as the cause of illness. About 3/4thof the study population had retained their diagnosis of Acute and transient psychotic disorders at the end of one-year follow up.
Supernatural and religious beliefs of patients and family members with stable diagnosis of acute and transient psychotic disorder at the end of one year was significantly low and believed more in stress and chemical imbalance as an aetiology of the illness. Supernatural and religious beliefs of patients and family members with a revised diagnosis of bipolar affective disorder, schizophrenia and relapse of acute and transient psychosis episode remained high even at the end of one year of follow up, the highest being in the relapse of acute psychosis group followed by schizophrenia group and bipolar affective group.
The belief in supernatural causation of the illness reins high even at the end of one year follow up. This calls for greater community and patient level education about the cause and treatability of psychiatric disorders. The findings of the present study can help in understanding the cultural vicissitudes of treatment of psychiatric disorders.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Malhotra S. Acute and transient psychosis: A paradigmatic approach. Indian J Psychiatr 2007; 49:233.
- Varma VK, Malhotra S, Yoo ES, Jiloha RC, Finnerty MT, Susser E. Course and outcome of acute non-organic psychotic states in India. Psychiatric quarterly. 1996 Sep;67(3):195-207.
- VarmaVK, MalhotraS, JilohaRC. Acute non-organic psychotic states in India: Symptomatology. Indian J Psychiatry 1992; 34:89-101.
- Malhotra S, Varma VK, Malhotra A. Classification of acute nonorganic psychotic states in India. Int J Mental Health 1992; 21:6-32.
- Indian Council of medical Research. Final report of phenomenology and natural history of acute psychosis. ICMR: New Delhi 1985.
- Das SK, Malhotra S, Basu D. Family study of acute and transient psychotic disorders: Comparison with schizophrenia. Soc Psy Psychiatr Epidem1999; 34:328-332.
- Susser E, Varma VK, Mattoo SK, et al. Long-term course of acute brief psychosis in a developing country setting. Br J Psychiatry 1998; 173:226-230
- Malhotra S, Gupta N, Gill S. Recurrence in acute and transient psychosis: Paper presented at the 13th World Congress of Psychiatry. Cairo, Egypt 2005; 10-15.
- Grover S, Davuluri T, Chakrabarti S. Religion, spirituality, and schizophrenia: a review. Indian J Psychol Med 2014; 36:119-124.
- Mohr S, Borras L, Gillieron C, et al. Spirituality, religious practices and schizophrenia: Relevance for the clinician. Revue Med Issues 2006; 2:2092-2024.
- Mohr S, Perroud N, Gillieron C, et al. Spirituality and religiousness as predictive factors of outcome in schizophrenia and schizo-affective disorders. Psychiatr Res 2011; 186:177-182.
- Mohr S. The relationship between schizophrenia and religion and its implications for care. Swiss Med Weekly 2004; 134.
- Koenig HG. Research on religion, spirituality, and mental health: A review. Canadian J Psychiatr 2009; 54:283-291.
- Zagozdzon P. Religiosity and health in epidemiological studies. Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego. 2012; 32:349-353.
- Kornreich C, Aubin HJ. Religion and brain functioning (part 2): Does religion have a positive impact on mental health?. Revue Med de Bruxelles 2012; 33:87-96.
- Balhara YP, Yadav T. A comparative study of beliefs, attitudes and behaviour of psychiatric patients and their care givers with regards to magico-religious and supernatural influences. J Med Sci 2012; 12:10-17.
- Angermeyer MC, Matschinger H. Relatives beliefs about the causes of schizophrenia. Acta Psychiatr Scand 1996; 93:199-204.
- Banerjee G, Roy S. Determinans of help seeking behaviour of families of schizophrneic patients attending a teaching hospital in India: An indegenous explanatory model. Int J Soc Psychiatry 1998; 44:199-214.
- Chakraborty A, Bhattacharya D. Witchcraft beliefs and persecutory ideas in Bengali culture. Indian J Soc Psychiatry 1985; 1:231-243.
- Kurihara T, Kato M, Reverger R, et al. Beliefs about causes of schizophrenia among family members: a community-based survey in Bali. Psychiatric Services 2006; 57:1795-1799.
- Prabhu G. Mental illness, public attitudes, and public education. Indian J Clin Psychol 1983; 10:13-26.
- Srinivasan TN, Thara R. Beliefs about causation of schizophrenia: Do indianfamilies believe in supernatural causes? Soc Psychiatr Epidemiol 1981; 36:134-140.
- Verghese A, Beig A. Public attitudes towards mental illness: The vellore study. Indian J Psychiatry 1974; 16:8-12.
Author Info
C Prarthana Saraswathi and S Nambi*
Department of Psychiatry, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: C Prarthana Saraswathi, S Nambi, One Year Follow-Up Study of Acute and Transient Psychosis with Specific Focus on Cultural Factors Influencing the Course and Outcome s, J Res Med Dent Sci, 2021, 9 (5):234-241.
Received: 03-Apr-2021 Accepted: 21-May-2021
