Research - (2022) Volume 10, Issue 1
OPG and CBCT-A More Reliable Source for Human Identification? Perception Based Web Survey among Dentist
Nandita R and Abirami Arthanari*
*Correspondence: Abirami Arthanari, Department of Forensic Odontology, Saveetha Institute of Medical and Technical Sciences, Saveetha University, India, Email:
Abstract
Introduction: An orthopantomogram is a panoramic scanning dental X-ray of the upper and lower jaw. An OPG is a wide view x-beam of the lower face, which shows all the teeth of the upper and lower jaw on a solitary film. It exhibits the number, position, and development of the multitude of teeth including those that have not yet surfaced or emitted. The OPG consists of a rotating arm with the X-ray source at one end and the film mechanism at the opposite extremity. AIM: The aim of the present study is to analyse the knowledge of OPG and CBCT among dentists. Materials and methods: Self-administered questionnaire of close-ended questions was prepared, and it was distributed among dental students from February to March 2021 through the online survey “google forms”. Data was analysed with the SPSS version (22.0). Descriptive statistics as percent were calculated to summarise qualitative data. Results: The questionnaire was distributed among 200 participants. 89.5% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics. 71.5% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region. 82.5% of the participants disagreed that OPG is better to see the root resorption. 81% of the participants agreed CBCT can be used for superimposition to evaluate the pre-post treatment changes. Conclusion: Dental practitioners had overall good knowledge and awareness on the more reliable source for human identification. In comparison with the experience of a dentist, 5-10 years of experience had good knowledge and awareness regarding the more reliable source for human identification.
Keywords
CBCT, OPG, Survey, Maxilla, 3D imaging, Eco friendly
Introduction
An orthopantomogram is a panoramic scanning dental Xray of the upper and lower jaw. An OPG is a wide view xbeam of the lower face, which shows all the teeth of the upper and lower jaw on a solitary film. It exhibits the number, position, and development of the multitude of teeth including those that have not yet surfaced or emitted [1]. The OPG consists of a rotating arm with the X-ray source at one end and the film mechanism at the opposite extremity. Advantages of OPGs are broad anatomic coverage, low patient radiation dose, convenience of examination, used in patients unable to open mouth etc. [2]. They require less time; cause no discomfort, painless and traumatic. Because of the diminished sharpness and clearness, it can't be utilized to analyse caries. It can't be utilized to decide interdental bone misfortune because of similar components (low sharpness) and furthermore the changes in periodontal ligament are deceiving [3]. Indications of orthopantomogram are third molars, evaluation of trauma, large lesion, and tooth development, intolerant to intraoral procedures.
Factors for interpretation are principle of image formation, techniques of patient positioning, and Radiographic appearance of normal anatomic structures etc., [4]. An OPG additionally exhibits the number, position, and development of the multitude of teeth including those that have not yet surfaced or emitted through the gum. It is unique in relation to the close-up x-beams dental specialists take of individual teeth. It shows less fine detail, however a lot more extensive zone of view [5]. This can be especially valuable to check hard to see zones like wisdom teeth, or the improvement of a child’s jaw and teeth. It is likewise regularly used to check your jaw joint, the TMJ (temporomandibular joint), at times called the CMA (crania-mandibular articulation), particularly if you grind your teeth [6].
Cone beam computed tomography (or CBCT, additionally referred to as C-arm CT, cone beam, volume CT, or flat panel CT) is a clinical imaging procedure comprising Xbeam figured tomography where the X-beams are dissimilar, shaping a cone [7]. CBCT has become progressively significant in treatment planning and determination in implant dentistry, ENT, orthopaedics, and interventional radiology (IR), in addition to other things. Maybe because of the expanded access to such innovation, CBCT scanners are presently finding numerous utilizations in dentistry, for example, in the fields of oral medical procedure, endodontics and orthodontics [8]. Coordinated CBCT is additionally a significant device for quiet situating and verification in image guided radiation treatment (IGRT). The scanning software gathers the information and recreates it, producing what is named an advanced volume made from three-dimensional voxels of anatomical information that would then be able to be controlled and imagined with particular programming [9]. CBCT imparts numerous similarities to traditional (fan beam) CT however there is significant contrasts, especially for reconstruction. CBCT has been depicted as the highest quality level for imaging [10]. Our team has extensive knowledge and research experience that has translate into high quality publications [11-30]. The aim of this study is to analyse the perceptions among various dentists about OPG and CBCT.
The aim of this study is to find a more reliable source for human identification amongst OPG and CBCT.
Material and Methods
Study design
A cross sectional study was conducted through an online survey from February to March 2021 among dentists.
Study subjects
A simple random sampling was used to select the study participants.
Inclusion criteria: All the dentists who were willing to participate were included.
Ethical considerations
The questionnaire was distributed among 200 participants. Returning the filled questionnaire was considered as implicit consent as a part of the survey. Ethical approval for the study was obtained from the Institutional Review Board (IRB), Saveetha Dental College.
Study methods
Self-administered questionnaire of close-ended questions was prepared, and it was distributed among dental practitioners and specialists from February to March 2021 through the online survey “Google forms”. The collected data were checked regularly for clarity, competence, consistency, accuracy, and validity. Demographic details were also included in the questionnaire.
Statistical analysis
Data was analysed with the SPSS version (22.0). Descriptive statistics as percent were calculated to summarise qualitative data. Chi square test was used to analyse and the confidence level was 95% and of statistical significance P<0.05.
Finally, the result was presented by using bar charts, pie charts and percentage tables.
Results
The questionnaire was distributed among 200 participants. Of the 200 participants, 53.4% of the participants were male while 46.6% of the participants were female. 33.3% of the participants had 0-5 years of experience, 33.3% of the participants had 5-10 years of experience while 33.3% of the participants had years of experience.
75.6% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics. 79% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region. 74.6% of the participants disagreed that OPG is better to see the root resorption.
62% of the participants agreed CBCT can be used for superimposition to evaluate the pre-post treatment changes. 91% of the participants agreed OPG is a more reliable source for human identification. 81.3% of the participants agreed that CBCT has lower radiation exposure as compared to OPG.
13.3% of the participants agreed that pre implant planning was the different purposes of using OPG, 12.3% of the participants agreed that post implant planning was the different purposes of using OPG, 17.6% of the participants agreed that impactions was the different purposes of using OPG while 56.6% of the participants agreed that root canal planning was the different purposes of using OPG. 13.3% of the participants agreed that pre implant planning was the different purposes of using CBCT, 12.3% of the participants agreed that post implant planning was the different purposes of using CBCT, 56.6% of the participants agreed that none of these were the different purposes of using CBCT.
13.3% of the participants agreed that board anatomic coverage was the advantage of using OPG, 12.3% of the participants agreed that cost effective was the advantage of using OPG, 17.6% of the participants agreed that low patient radiation exposure was the advantage of using OPG, 56.6% of the participants agreed that convenience of examination was the advantage of using OPG (Figure 1-15).
Figure 1. Pie chart showing the gender of the participants. 53.33% of the participants were male while 46.67% of the participants were female.
Figure 2. Pie chart showing the year of experience of the participants. 33.33% of the participants had 0-5 years of experience, 33.33% of the participants had 5-10 years of experience while 33.33% of the participants had more than 10 years of experience.

Figure 3. Pie chart showing that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics. 75.6% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics.
Figure 4. Pie chart showing that OPG is the preferred mode of 3D imaging for the head and neck region. 79% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region.
Figure 5. Pie chart showing that OPG is better to see the root resorption. 74.6% of the participants disagreed that OPG is better to see the root resorption.
Figure 6. Pie chart showing that CBCT can be used for superimposition to evaluate the pre-post treatment changes. 62% of the participants agreed CBCT can be used for superimposition in order to evaluate the pre-post treatment changes.
Figure 7. Pie chart showing that OPG is a more reliable source for human identification. 91% of the participants agreed OPG is a more reliable source for human identification.
Figure 8. Pie chart showing that CBCT has lower radiation exposure as compared to OPG. 81.3% of the participants agreed that CBCT has lower radiation exposure as compared to OPG.
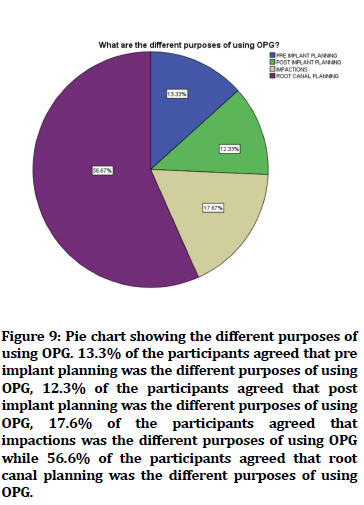
Figure 9. Pie chart showing the different purposes of using OPG. 13.3% of the participants agreed that pre implant planning was the different purposes of using OPG, 12.3% of the participants agreed that post implant planning was the different purposes of using OPG, 17.6% of the participants agreed that impactions was the different purposes of using OPG while 56.6% of the participants agreed that root canal planning was the different purposes of using OPG.
Figure 10. Pie chart showing the different purposes of using CBCT. 13.3% of the participants agreed that pre implant planning was the different purposes of using CBCT, 12.3% of the participants agreed that post implant planning was the different purposes of using CBCT, 56.6% of the participants agreed that none of these were the different purposes of using CBCT.
Figure 11. Bar graph showing the advantages of using CBCT. 13.3% of the participants agreed that board anatomic coverage was the advantage of using OPG, 12.3% of the participants agreed that cost effective was the advantage of using OPG, 17.6% of the participants agreed that low patient radiation exposure was the advantage of using OPG, 56.6% of the participants agreed that convenience of examination was the advantage of using OPG.
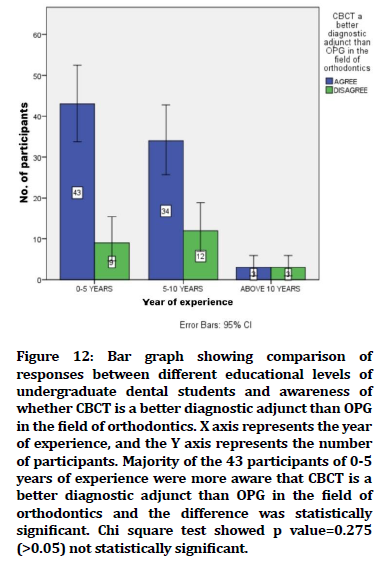
Figure 12. Bar graph showing comparison of responses between different educational levels of undergraduate dental students and awareness of whether CBCT is a better diagnostic adjunct than OPG in the field of orthodontics. X axis represents the year of experience, and the Y axis represents the number of participants. Majority of the 43 participants of 0-5 years of experience were more aware that CBCT is a better diagnostic adjunct than OPG in the field of orthodontics and the difference was statistically significant. Chi square test showed p value=0.275 (>0.05) not statistically significant.
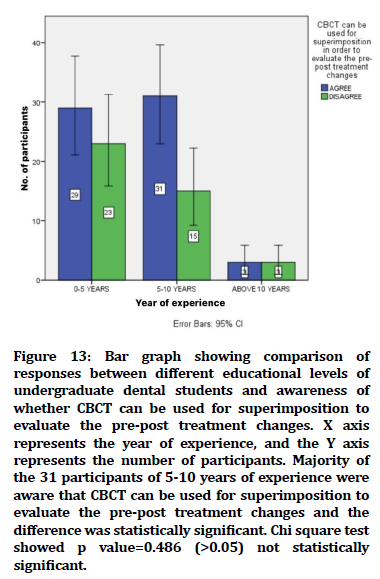
Figure 13. Bar graph showing comparison of responses between different educational levels of undergraduate dental students and awareness of whether CBCT can be used for superimposition to evaluate the pre-post treatment changes. X axis represents the year of experience, and the Y axis represents the number of participants. Majority of the 31 participants of 5-10 years of experience were aware that CBCT can be used for superimposition to evaluate the pre-post treatment changes and the difference was statistically significant. Chi square test showed p value=0.486 (>0.05) not statistically significant.
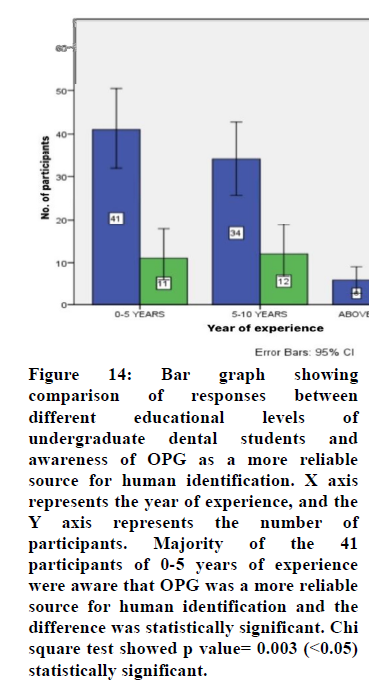
Figure 14. Bar graph showing comparison of responses between different educational levels of undergraduate dental students and awareness of OPG as a more reliable source for human identification. X axis represents the year of experience, and the Y axis represents the number of participants. Majority of the 41 participants of 0-5 years of experience were aware that OPG was a more reliable source for human identification and the
difference was statistically significant. Chi square test showed p value= 0.003 (<0.05) statistically significant.
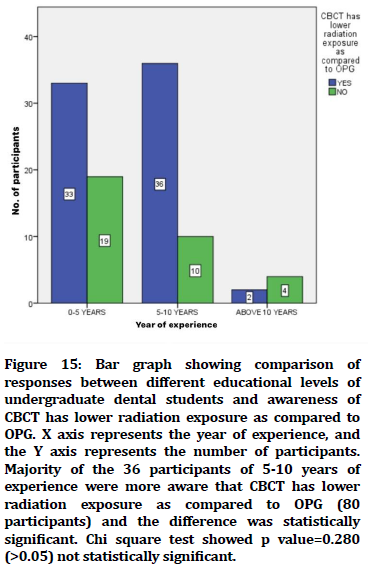
Figure 15. Bar graph showing comparison of responses between different educational levels of undergraduate dental students and awareness of CBCT has lower radiation exposure as compared to OPG. X axis represents the year of experience, and the Y axis represents the number of participants. Majority of the 36 participants of 5-10 years of experience were more aware that CBCT has lower radiation exposure as compared to OPG (80 participants) and the difference was statistically significant. Chi square test showed p value=0.280 (>0.05) not statistically significant.
Discussion
In the present study, 75.6% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics. A similar study, the author concluded that 87.8% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics [31]. In contrast, the author concluded that 68% of the participants agreed that CBCT was a better diagnostic adjunct than OPG in the field of orthodontics [32].
In the present study, 79% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region. A similar study, the author concluded that 70.8% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region [31]. In contrast, the author concluded that 47% of the participants disagreed that OPG is the preferred mode of 3D imaging for the head and neck region [33].
In the present study, 74.6% of the participants disagreed that OPG is better to see the root resorption. In contrast, the author concluded that 96.7% of the participants disagreed that OPG is better to see root resorption [34].
In the present study, 62% of the participants agreed CBCT can be used for superimposition in order to evaluate the pre-post treatment changes. In contrast, the author concluded that 58.1% of the participants agreed CBCT can be used for superimposition in order to evaluate the pre-post treatment changes [34].
In the present study, 81.3% of the participants agreed that CBCT has lower radiation exposure as compared to OPG. In contrast, the author concluded that 57% of the participants agreed that CBCT has lower radiation exposure as compared to OPG [35]. A similar study, the author concluded 70% of the participants agreed that CBCT has lower radiation exposure as compared to OPG [36].
In the present study, 13.3% of the participants agreed that pre implant planning was the different purposes of using OPG, 12.3% of the participants agreed that post implant planning was the different purposes of using OPG, 17.6% of the participants agreed that impactions was the different purposes of using OPG while 56.6% of the participants agreed that root canal planning was the different purposes of using OPG. A similar study, the author concluded that 17.5% of the participants agreed that pre implant planning was the different purposes of using OPG, 23.5% of the participants agreed that post implant planning was the different purposes of using OPG, 37.5% of the participants agreed that impactions was the different purposes of using OPG while 21% of the participants agreed that root canal planning was the different purposes of using OPG [37].
In the present study, 13.3% of the participants agreed that pre implant planning was the different purposes of using CBCT, 12.3% of the participants agreed that post implant planning was the different purposes of using CBCT, 56.6% of the participants agreed that none of these were the different purposes of using CBCT. In contrast, the author concluded that 30% of the participants agreed that pre implant planning was the different purposes of using CBCT, 25% of the participants agreed that post implant planning was the different purposes of using CBCT, 25% of the participants agreed that both pre implant planning and post implant planning was the different purposes of using CBCT. The limitation of this study was biased sampling, an equal number of participants can be included from different years of experience to get more accuracy in the results. The future scope of this study is that it can be expanded widely to include an equal number of participants to assess the awareness and knowledge on OPG and CBCT.
Conclusion
Dental practitioners had overall good knowledge and awareness on the more reliable source for human identification. In comparison with the experience of a dentist, 5-10 years of experience had good knowledge and awareness regarding the more reliable source for human identification. It is recommended that dentists and specialists should be more exposed and motivated about the reliable source for human identification during their dental education to be prepared for future practice of utilizing OPG and CBCT.
Acknowledgement
The author would like to thank the department Forensic Odontology, Saveetha Dental College and Hospital, Chennai, for helping with research.
Author Contribution
I carried out literature research, data collection, data analysis and manuscript writing. Dr Abirami Arthanari conceived the study, participated in its design, and coordinated and provided guidance to draft the manuscript. All the authors have equally contributed in developing the manuscript.
Conflict of Interest
Nil.
Source of Funding
• Saveetha Institute of Medical and Technical Science, Saveetha Dental College.
• Faamys Fashions.
References
- Hsu HC, Jozsef G, Formenti SC. Daily CBCT versus biweekly CBCT versus portal imaging for partial breast irradiation. Int J Radia Oncol 2012; 84:S734.
- Aditya A, Lele S, Aditya P. Current status of knowledge, attitude, and perspective of dental practitioners toward cone beam computed tomography: A survey. J Oral Maxillofac Radiol 2015; 3:54.
- Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Canad Dent Asso 2006; 72:75.
- Scarfe WC, Angelopoulos C, de Azevedo BC, et al. Dental and maxillofacial cone beam computed tomography. Handbook of X-Ray Imag 2017; 867â??86.
- Abdelkarim A. Orthodontic radiographs: Guidelines for the use of radiographs in clinical orthodontics. Am J Orthodont Dentofac Orthoped 2016; 149:141-2.
- Horner K, Barry S, Dave M, et al. Diagnostic efficacy of cone beam computed tomography in paediatric dentistry: A systematic review. Euro Arch Paediatr Dent 2020; 21:407-26.
- Aps JK. Cone beam computed tomography in paediatric dentistry: Overview of recent literature. Eur Arch Paediatr Dent 2013; 14:131-40.
- Katheria BC, Kau CH, Tate R, et al. Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatr Dent 2010; 32:304-9.
- Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 1: physical principles. Am J Neuroradiol 2009; 30:1088-95.
- Santhakumar P, Prathap L. Awareness on preventive measures taken by health care professionals attending COVID-19 patients among dental students. Euro J Dent 2020; 14:S105-9.
- Mathew MG, Samuel SR, Soni AJ, et al. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: Randomized controlled trial. Clin Oral Investig 2020; 24:3275-80.
- Sridharan G, Ramani P, Patankar S, et al. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med 2019; 48:299â??306.
- Hannah R, Ramani P, Ramanathan A, et al. CYP2 C9 polymorphism among patients with oral squamous cell carcinoma and its role in altering the metabolism of benzo [a] pyrene. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 130:306-12.
- Antony JVM, Ramani P, Ramasubramanian A, et al. Particle size penetration rate and effects of smoke and smokeless tobacco products - An invitro analysis. Heliyon 2021; 7:e06455.
- Sarode SC, Gondivkar S, Sarode GS, et al. Hybrid oral potentially malignant disorder: A neglected fact in oral submucous fibrosis. Oral Oncol 2021; 105390.
- Hannah R, Ramani P, WM Tilakaratne, et al. Author response for “Critical appraisal of different triggering pathways for the pathobiology of pemphigus vulgarisâ??A review”. Wiley 2021.
- Chandrasekar R, Chandrasekhar S, Sundari KKS, et al. Development and validation of a formula for objective assessment of cervical vertebral bone age. Prog Orthod 2020; 21:38.
- Subramanyam D, Gurunathan D, Gaayathri R, et al. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Eur J Dent 2018; 12:67â??70.
- Jeevanandan G, Thomas E. Volumetric analysis of hand, reciprocating and rotary instrumentation techniques in primary molars using spiral computed tomography: An in vitro comparative study. Eur J Dent 2018; 12:21â??6.
- Ponnulakshmi R, Shyamaladevi B, Vijayalakshmi P, et al. In silico and in vivo analysis to identify the antidiabetic activity of beta sitosterol in adipose tissue of high fat diet and sucrose induced type-2 diabetic experimental rats. Toxicol Mech Methods 2012; 29:276â??90.
- Sundaram R, Nandhakumar E, Haseena Banu H. Hesperidin, a citrus flavonoid ameliorates hyperglycemia by regulating key enzymes of carbohydrate metabolism in streptozotocin-induced diabetic rats. Toxicol Mech Methods 2012; 29:644â??53.
- Alsawalha M, Rao CV, Al-Subaie AM, et al. Novel mathematical modelling of Saudi Arabian natural diatomite clay. Mater Res Express 2019; 6:105531.
- Yu J, Li M, Zhan D, et al. Inhibitory effects of triterpenoid betulin on inflammatory mediators inducible nitric oxide synthase, cyclooxygenase-2, tumor necrosis factor-alpha, interleukin-6, and proliferating cell nuclear antigen in 1, 2-dimethylhydrazine-induced rat colon carcinogenesis. Pharmacogn Mag 2020; 16:836.
- Hema Shree K, Ramani P, Sherlin H, et al. Saliva as a diagnostic tool in oral squamous cell carcinoma: A systematic review with meta-analysis. Pathol Oncol Res 2019; 25:447â??53.
- Zafar A, Sherlin HJ, Jayaraj G, et al. Diagnostic utility of touch imprint cytology for intraoperative assessment of surgical margins and sentinel lymph nodes in oral squamous cell carcinoma patients using four different cytological stains. Diagn Cytopathol 2020; 48:101â??10.
- Karunagaran M, Murali P, Palaniappan V, et al. Expression and distribution pattern of podoplanin in oral submucous fibrosis with varying degrees of dysplasia â?? an immunohistochemical study. J Histotechnol 2019; 42: 80â??6.
- Sarode SC, Gondivkar S, Gadbail A, et al. Oral submucous fibrosis and heterogeneity in outcome measures: A critical viewpoint. Future Oncol 2021; 17:2123â??6.
- Raj Preeth D, Saravanan S, Shairam M, et al. Bioactive zinc(II) complex incorporated PCL/gelatin electrospun nanofiber enhanced bone tissue regeneration. Eur J Pharm Sci 2021; 160:105768.
- Prithiviraj N, Yang GE, Thangavelu L, et al. Anticancer compounds from starfish regenerating tissues and their antioxidant properties on human oral epidermoid carcinoma kb cells. Pancreas 2020; 155â??6.
- Sugumaran S, George AM, Arvind Kumar S, et al. Knowledge, awareness, and practice of cone-beam computed tomography among orthodontists: a survey. J Ind Orthodont Soci 2018; 42: 255â??64.
- Haney E, Gansky SA, Lee JS, et al. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofacial Orthop 2010; 137:590â??7.
- Balabaskaran K, Srinivasan AL. Awareness and attitude among dental professional towards CBCT. J Dent Medi Sci 2013; 10:55â??59.
- Liedke GS, da Silveira HED, da Silveira HLD, et al. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endodont 2009; 35: 233â??5.
- Hol C, Hellén-Halme K, Torgersen G, et al. How do dentists use CBCT in dental clinics? A Norwegian nationwide survey. Acta Odontol Scand 2015; 73:195â??201.
- Patil NA, Gadda RB, Salvi R. Cone beam computed tomography: adding the third dimension. J Contemp Dentis 2012; 2:84â??8.
- Cattaneo PM, Bloch CB, Calmar D, et al. Comparison between conventional and cone-beam computed tomography-generated cephalograms. Am J Orthod Dentofacial Orthop 2008; 134:798â??802.
- Rhee CH, Choi YK, Kim YI, et al. Correlation between skeletal and dental changes after mandibular setback surgery-first orthodontic treatment: Cone-beam computed tomography-generated half-cephalograms. Kor J Orthodont 2015; 45:59.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Nandita R and Abirami Arthanari*
Department of Forensic Odontology, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, IndiaCitation: Nandita R, Abirami Arthanari, OPG and CBCT-A More Reliable Source for Human Identification? Perception Based Web Survey among Dentist, J Res Med Dent Sci, 2022, 10(1): 203-211
Received: 10-Dec-2021, Manuscript No. JRMDS-21-41541; , Pre QC No. JRMDS-21-41541 (PQ); Editor assigned: 13-Dec-2021, Pre QC No. JRMDS-21-41541 (PQ); Reviewed: 27-Dec-2021, QC No. JRMDS-21-41541; Revised: 30-Dec-2021, Manuscript No. JRMDS-21-41541 (R); Published: 06-Jan-2022
