Research - (2021) Volume 9, Issue 9
Oral Manifestations of COVID-19 Patients: Two Case Reports of Egyptian Patients
Malak Yousef Mohamed Shoukheba1*, Enas Ahmed Elgendy2 and Omar Mohamed Fayed3
*Correspondence: Malak Yousef Mohamed Shoukheba, Department of Oral Medicine, Periodontology, Oral diagnosis and Radiology, Faculty of Dentistry, Tanta University, Egypt, Email:
Abstract
Nowadays, Coronavirus disease (COVID-19) has emerged as a terrifying global health threat. Saliva and nasopharyngeal secretions can hold a high viral load, which threatens the dental profession and makes it at the top of the list of infection spread. Oral transmission has been considered to be one of the most important methods of COVID-19 infection. Change or loss of taste and smell sensation are the most important symptoms for covid-19 patients. The oral cavity offers clues about the health of the whole body and a mirror reflecting the state of your overall health. Many pieces of literature reporting that oral lesions could be a probable clinical characteristic of COVID-19. However, oral manifestations remain uncertain, and still a gap of knowledge about the impact of COVID-19 on the oral cavity. All the cases in this report detected by chance from daily life and the patients confirmed positive COVID after detection of the oral lesions. Our aim is to report additional cases of COVID patients with oral manifestation and its importance in the early diagnosis of COVID-19.
Keywords
COVID-19, SARS-CoV-2, Coronavirus, Oral manifestation, oral lesions
Introduction
Acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that emerged at 2019 is responsible for large-scale of illnesses and deaths around the world. It is caused by a single positive stranded RNA virus from the coronavirus (CoV) family of Coronaviridae [1].
The mode of transmission of SARS-CoV-2 occurs by droplets or contact transmission. Saliva can carry a risk of transmission of COVID-19, either by direct contact or indirect contact with contaminated stuff [2,3].
A study has noticed the presence of SARS-CoV-2 in the saliva of 91.7% COVID-19 patients, with a median viral load of 3.3 X 106 copies/ml [4], and the detection rate of SARS-CoV-2 has been reported to be higher in saliva than nasopharyngeal swabs [5]. The incubation period of COVID-19 ranged from 1 to14 day. Early detection of symptoms is life-saving [6]. Mucocutaneous manifestations can play a role in the early diagnosis [7].
The characteristic clinical symptoms of COVID-19 patients were high temperature, cough, sore throat, dyspnea, and muscle pain, with abnormal chest CT, whereas the less dominant symptoms were sputum secretion, headache, haemoptysis, and gastrointestinal disturbance. In progressive cases, pneumonia, myocardial damage, coagulation dysfunction, encephalopathy, organ failure, and death. A great number of studies reported that the mouth is one of the extra respiratory places that have shown manifestations in COVID-19 patients [8]. Moreover, recent reports revealed that xerostomia, change of taste and smell which might arise before the conventional signs of COVID-19 may represent as the first and only manifestations of the virus [9-11].
Common laboratory findings include bilateral or unilateral ground-glass opaqueness, and patchy shadowing on chest CT [12], and increases in neutrophil/lymphocyte ratio, serum D-dimer, and lactate dehydrogenase, in aggressive cases [13].
Current evidence indicated that angiotensin-converting enzyme 2 (ACE2) acts as the primary host cell receptor of the virus as it binds to ACE2 by the spike-like protein on its surface, hence, ACE2 works as a gateway into the cell for the coronavirus [14,15]. That is why the lung is the targeted organ for the virus because of high ACE2 expression on the lung cells.
Angiotensin is also expressed on the oral mucosa, especially in tongue and salivary gland cells, which might clarify the incident of losses of taste and oral ulceration due to the damage of keratinocytes and oral fibroblasts [14]. In this report, we reported many oral mucosal lesions that could be observed in COVID-19 positive patients.
Case Presentation
The patients we presented provided verbal consent through the phone to publish the characteristics and pictures of their cases in the condition that their identity is protected.
Case no: 1
A 55 years old female patient came to the oral medicine clinic of the faculty of dentistry at Tanta University on February 2021 complaining of multiple oral ulcers, burning sensation, dry mouth, and lip ulcer oozing blood. When we asked her about any other symptoms she gave the history of fever increase at night, bone pain, difficulty breathing, and headache. She said that fever and pain all over the body started first and after 5 days the ulceration erupted and she cannot eat or swallow.
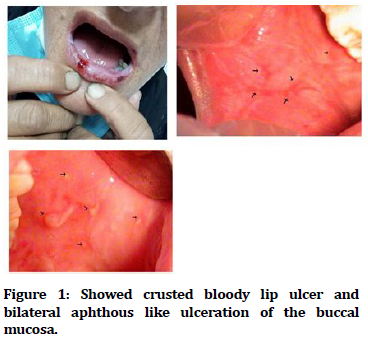
Her medical history is positive for hypertension, anemia, and kidney stone and she is on aspirin and antihypertension drugs concor 5 mg. The intra-oral examination revealed several ulcers located bilaterally on the cheek mucosa (similar to aphthous ulcer) and hemorrhagic crusted lesion on the fissured lower lip (Figure 1).
Figure 1. Showed crusted bloody lip ulcer and bilateral aphthous like ulceration of the buccal mucosa.
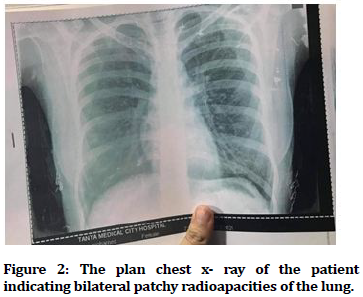
We instructed her to make a chest x-ray (Figure 2) and consult a chest physician and do investigations for COVID -19. We prescribed her Hexitol mouth wash and Oracure gel for ulcers. After 2 days the patient phoned me and confirmed that she is positive corona and started the protocol of the treatment.
Figure 2. The plan chest x- ray of the patient indicating bilateral patchy radioapacities of the lung.
Case no: 2
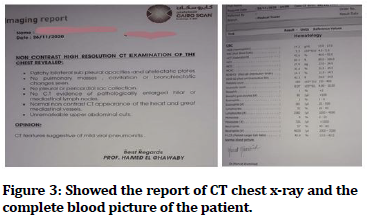
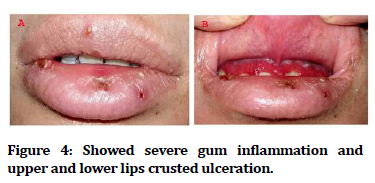
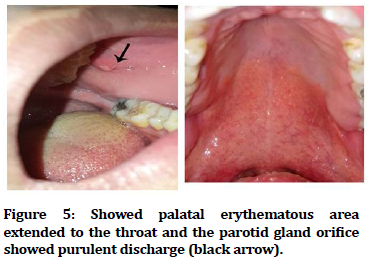
A 22-year-old female medical student, Cairo university, tested positive for COVID-19 on November 2020 by chest CT x-ray, complete blood picture CBC (Figure 3) and C reactive protein and PCR from nasopharynx swap, the patient communicated with us through phone as she was complaining from severe gum inflammation and upper and lower lip crusted lesion and ulceration (Figure 4). After she had taken the protocol of treatment she started to complain from posterior palatal atrophic erythematous area extended to the throat and the parotid gland office showed purulent discharge with bilateral pain in the parotid gland (black arrow) (Figure 5). We asked the patient to take photographs of the oral lesions and to send them to us. We prescribed for her mouth wash (chlorhexidine 0.12 %) and instructed her to drink enough water, lemon drops, or vitamin C lozenges to stimulate salivary wash and to do massage to the gland and she is already on the antibiotic.
Figure 3. Showed the report of CT chest x-ray and the complete blood picture of the patient.
Figure 4. Showed severe gum inflammation and upper and lower lips crusted ulceration.
Figure 5. Showed palatal erythematous area extended to the throat and the parotid gland orifice showed purulent discharge (black arrow).
Discussion
Diagnosis of COVID-19 is solely reliant on the classic respiratory symptoms that are common with other chest diseases. Additionally, some laboratory investigations including leukopenia with lymphopenia, increase Creactive proteins and decrease procalcitonin levels are good-established diagnostic aids [12,13]. Most of the physician ignores the oral manifestation of the systemic infection or diseases. Oral manifestations of COVID are often not highly recorded due to ignorance of intraoral inspection during hospital admission or examination of the patients and most of the patients were in quarantine [16]. The oral cavity is the gate to the internal medicine and internal organs that physicians should observe during the examination of the patients.
Current research shows that coronavirus raps human cells by angiotensin-converting enzyme-2 receptors causing inflammation in the associated organs and tissues [17]. The expression of ACE-2 receptors in the buccal mucosa and salivary glands, and the highest detection rate of SARS-CoV-2 RNA in saliva [18], could explain the correlation between the reported oral lesions and the COVID virus.
Although some clinical findings have proposed an association between oral changes and SARS-CoV-2 infection, there is yet a query about the pathophysiologic base of these manifestations, whether they are due to direct viral infection, co-infections, due to anxiety drug reactions, or side effects [19].
Another point of view is the medications used in the treatment for COVID that could undesirably affect oral mucosa leading to many infections (viral, fungal, and bacterial infection) and oral ulcerations due to the altered immune system and the decreased salivary secretion [20].
At the same time, we cannot ignore these manifestations as they may be the only manifestation in early infection by the virus or occurs in an asymptomatic COVID case, therefore, complete ignorance may result in a miss diagnosis of a positive case resulting in more infection spread and complications [21]. At the same time the study of these manifestations and paying attention to them will grant the early diagnosis and isolation of the patients.
The most frequently noticed oral manifestation is oral ulcers in different areas of the mouth (54.1%) [22]. White coating of the tongue features, dysgeusia, ageusia, petechiae, reddish macules, sores, necrotizing gingival conditions, gingivitis, and erythema multiforme-like lesions were recorded as a result of the altered immune system [23].
Our first case was complaining of burning sensation, dry mouth, and lip ulcer, this may be due to decreased salivary secretion as a possible complication of chronic sialadenitis initiated by COVID-19 [16]. Salivary glands can serve as a source for a dormant infection that may be revived with a risk of chronic sialadenitis [24]; therefore, any change in salivary glands or their secretions may be an alarm to the physicians to pay more attention.
In the second case, the patient was complaining of pain in the parotid gland and by examination, we found pus in the orifice of the stensen duct of the gland indicating suppurative sialadenitis this can be explained by the effect of the virus on the salivary gland and the high viral load in the glands where it replicates.
Crusted ulcer of the Lip lesion in this case also resemble erythema multiform lesion and like this lesion was reported in a brief review of more than 170 cases done by Eghbali [25], three out of four patients developed erythema multiforme-like outbreaks, in the form of palatal macules and petechiae, and one presented with three viscules in the inner lip mucosa [26]. This might be due to the exaggerated immune reaction to COVID-19 which stimulates the Langerhans' cells and lymphocytes, to initiate Vasculitis [27].
Ciccarese et al. [28] described a 19-year-old female patient with COVID-19, who was complaining of macules, papules, and petechiae on the lower extremities on physical examination. It also was observed erosions, ulcers, and blood scabs on the labial mucosa, as well as petechiae on the palate and gums.
Kahraman et al. [29] also reported the incidence of a largely erythematous surface in the oropharynx and oral petechiae and numerous prominent pustular. Coronavirus causes inflammation and exaggerated immune reactions, which can cause overproduction of cytokines. Lymphopenia takes place after the T-cell attack and innate/ acquired immune responses, causes altered lymphopoiesis and increased apoptosis of lymphocyte [21].
So, while waiting for conclusive, accessible data on pathognomonic oral lesions of COVID-19, the report of differential diagnoses for oral erythematous, ulcerative condition or purpura should also add SARS-CoV-2 infection as likelihood and the patient should be conscious and must be tested if needed.
Based on the present information, it is not easy to prove whether these manifestations are direct sequelae of COVID-19 or due to extra causes such as coinfection, or reactions to the used drugs.
We need more longitudinal studies aimed to explain oral manifestation due to coronavirus, and clarify the mechanisms of the development of these oral lesions because there is no confirmed evidence to prove that the described petechiae, ulcers, and vesiculobullous lesions represent intraoral signs of SARS-CoV-2 infection.
References
- Ludwig S, Zarbock A. Coronaviruses and SARS-CoV-2: A brief overview. Anesth Analg 2020; 31:93-96.
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Intern. J of Oral Sci, 2020,12(1), 1–6.
- Speth MM, Singer-Cornelius T, Obere M, et al. Olfactory dysfunction and sinonasal symptomatology in COVID-19: Prevalence, severity, timing, and associated characteristics. Otolaryngol Head Neck Surg 2020; 163:114–120.
- Kapoor P, Chowdhry A, Kharbanda OP, et al. Exploring salivary diagnostics in COVID-19: A scoping review and research suggestions. BDJ Open 2021; 7:8.
- Iwasaki S, Fujisawa S, Nakakubo S, et al. Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva. J Infect 2020; 81:e145-e147.
- Christelle Elias, Abel Sekri, Pierre Leblanc, et al. The incubation period of COVID-19: A meta-analysis. Intern J of Infec Diseas 2021; 104:708-710.
- Young TK, Shaw KS, Shah JK, et al. Mucocutaneous manifestations of multisystem inflammatory syndrome in children during the COVID-19 pandemic. Dermatol 2021; 157:207-212.
- Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. Br Med J 2020; 368:606.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506
- Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur Arch Otorhinolaryngol 2020; 277:2251–2261.
- Tsuchiya H. Oral symptoms associated with COVID-19 and their pathogenic mechanisms: A literature review. Dent J 2021; 9:32.
- Hefeda MM. CT chest findings in patients infected with COVID-19: Review of literature. Egyptian J Radiol Nuclear Med 2020; 51:239.
- Kermali M, Khalsa RK, Pillai K, et al. The role of biomarkers in diagnosis of COVID-19–A systematic review. Life Sci 2020; 254: 117788.
- Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382:1177-1179.
- Ciaglia E, Vecchione C, Puca AA. COVID-19 infection and circulating ACE2 levels: Protective role in women and children. Front Pediatr 2020; 8:206.
- El Kady DM, Gomaa EA, Abdella WS, et al. Oral manifestations of COVID-19 patients: An online survey of the Egyptian population. Clin Exp Dent Res 2021; 10.
- Peng Zhou, Xing-Lou Yang, Xian-Guang, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature 2020; 579:270-273
- Vinayachandran D, Balasubramanian S. Is gustatory impairment the first report of an oral manifestation in COVID-19? Oral Dis 2021; 27:748–749.
- Sampson V, Kamona N, Sampson A. Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br Dent J 2020; 228:971-975.
- Dziedzic A, Wojtyczka R . The impact of coronavirus infectious disease 19 (COVID-19) on oral health. Oral Dis 2021; 27:703-706.
- Etemad-Moghadam S, Alaeddini M. Is SARS-CoV-2 an etiologic agent or predisposing factor for oral lesions in COVID-19 patients? A concise review of reported cases in the literature. Int J Dent 2021; 18:6648082.
- Bemquerer LM, de Arruda JAA, Soares MPD, et al. The oral cavity cannot be forgotten in the COVID-19 era: Is there a connection between dermatologic and oral manifestations?. J Am Acad Dermatol 2021; 84:e143-e145.
- Halboub E, Al-Maweri SA, Alanazi RH, et al. Orofacial manifestations of COVID-19: A brief review of the published literature. Braz Oral Res 2020; 34:e124.
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020; 323:1843-1844.
- Eghbali Zarch R, Hosseinzadeh P . COVID-19 from the perspective of dentists: A case report and brief review of more than 170 cases. Dermato Therap 2021; 34:e14717.
- Jimenez-Cauhe J, Ortega-Quijano D, Carretero-Barrio I, et al. Erythema multiforme-like eruption in patients with COVID-19 infection: Clinical and histological findings. Clin Exp Dermatol 2020; 45:892-895.
- Guerini-Rocco E, Taormina SV, Vacirca D, et al. SARS-CoV-2 detection in formalin-fixed paraffin-embedded tissue specimens from surgical resection of tongue squamous cell carcinoma. J Clin Pathol 2020; 73:754-757.
- Ciccarese G, Drago F, Boatti M, et al. Oral erosions and petechiae during SARSâ?CoVâ?2 infection. J Med Virol 2020; 6:1-4.
- Kahraman FC, ÇaÅ?kurlu H. Mucosal involvement in a COVIDâ?19â?positive patient: A case report. Dermatol Ther 2020; 10:e13797.
Author Info
Malak Yousef Mohamed Shoukheba1*, Enas Ahmed Elgendy2 and Omar Mohamed Fayed3
1Department of Oral Medicine, Periodontology, Oral diagnosis and Radiology, Faculty of Dentistry, Tanta University, Egypt2Department of Oral Medicine, Periodontology, Oral diagnosis and Radiology, Faculty of Dentistry, Kafr El-Sheikh University, Egypt
3Faculty of Medicine, Egypt Cairo University, Egypt
Citation: Malak Yousef Mohamed Shoukheba, Enas Ahmed Elgendy, Omar Mohamed Fayed, Oral Manifestations of COVID-19 Patients: Two Case Reports of Egyptian Patients, J Res Med Dent Sci, 2021, 9(9): 44-47
Received: 12-Jul-2021 Accepted: 06-Sep-2021