Research - (2023) Volume 11, Issue 2
Orthodontic Sectors Applications for Wrong Positions of the Ankylosed Teeth by Dental Implant
Aseel Niema Hafith*, Waleed Shallal and Bakir Ghanem Murrad
*Correspondence: Aseel Niema Hafith, Department of Dentistry, Kut University College, Kut, Wasit, Iraq, Email:
Abstract
Background: Dental implants put incorrectly might cause cosmetic harm that is hard to fix with prostheses. Continuous anterior alveolar development causes anterior implants, such ankylosed teeth, to shift over time, causing infraocclusion. Misplaced dental implants have different therapies.
Method: The Orthodontic Bone Stretching approach utilizes partial osteotomies and high orthodontic pressures to move an implant in the improper location. The provided force improves cosmetic rehabilitation by repositioning the axis of implant and line of gingival. This relocation is made feasible by stretching bone in the operative region without rapid repositioning or mobilization. Implant repositioning instances handled using Orthodontic Bone Stretching.
Result: The cosmetic qualities of the face and smile were improved by orthodontic therapy and orthodontic bone stretching. In the palatal direction, the movement of the implant was 0.60 millimeters at the apexal and 7 millimeters at the edge of incisal. The superimpositions demonstrated that there was a movement of 4 millimeters in the palatal direction at the implant-abutment junction, and 7 millimeters at the incisal edge. Even though preventative periodontal care was being performed, plaque management was not particularly effective.
Conclusion: In each of the three examples that were given, the implant relocation was accomplished with the help of the orthodontic bone stretching method. Additionally, the prosthetic crowns in each of the patients' smiles were altered in order to achieve better cosmetic results.
Keywords
Malposition, Orthodontic, Stretching, Correcting, Implantingc
Introduction
In the front of the jaw, it's tough to achieve a flawless esthetic result and much harder to preserve it over time [1]. The anterior alveolar bone keeps growing even after puberty. Puberty begins the slowing process. Animal and clinical research shows implants don't track patient development. In younger individuals, immobility might cause infraocclusion and cosmetic difficulties. Open bite facial patterns and women are at danger [2]. Kylosed teeth also have this effect. In many situations, lack of growth around the implant causes misalignment of nearby teeth. The area surrounding the implant has no space to develop [3]. CFAO preparation and surgical guiding enhance implantology surgeries, leading to proper implant placement in most instances. CFAO preparation and surgical guiding. Incorrect implant placement might cause cosmetic failures [4]. If an implant is put too far buccally and lacks adequate angulation, the crown will be excessively lengthy and the gingival line will be misaligned. This causes aesthetic and practical problems [5]. This will be unattractive. This visual defect may worsen with gingival recession. (Example:) When improper placement is modest, a prosthetic customized framework abutment may be used [6]. This is a possible therapeutic [7]. Adjusting the prosthetic method cannot improve the esthetic look of large malposition. In these cases, the only options are to keep the implant in place or physically remove it. These are the only two options available [8]. Implant removal typically causes difficulties that require reconstructing soft and hard tissues and inserting a new implant [9]. This long and difficult therapy is the ideal for mispositioned implants with significant gingival recession or bone loss. Both disorders have terrible esthetic prognoses, hence this therapy is ideal [10]. Ankylosed teeth may resemble Osseo integrated implants due to how they develop or age. Ankylosed teeth act differently as they age [11]. Several surgical methods may reverse tooth ankylosis, each with its own pros and cons. This study describes these procedures as an alternate treatment for avulsion. As an alternative to implant removal, several treatment techniques for implant relocation are available if the implant has completely Osseo integrated and there are no hard or soft tissue defects surrounding it [12]. This is done to avoid removing the implant. First, consider segmental osteotomy and bone block displacement [13]. Osteotomy followed by distraction is another option. Orthodontic Bone Stretching, is a novel procedure for correcting ankylosed teeth with promising results [14- 16]. Given this procedure's effectiveness in moving ankylosed teeth, it would be fascinating to see whether it can also relocate implants [17-19]. For the purpose of explaining the relocation of three maxillary incisors that had been displaced by a malposition implant, this research employs the orthodontic bone stretching approach. These incisors were moved because of the implant.
Methods
Orthodontic Bone Stretching (OBS)
Surgery requirements
It is possible to exert control not only over the bone level but also over the osseointegration of the implant. The procedure of selecting where the implant should go includes the use of images, dental casts, and imaging analysis as some of its constituent parts. The orthodontic preparation process may be used to treat a malocclusion, which is a more precise term for a misalignment of the teeth. The implant is not included in this preparation in any way.
Surgical methods
The patient will be prescribed prednisolone 50 mg twice daily for four days, amoxicillin 1 gram twice daily for seven days, paracetamol 1 gram twice daily for three days, and a 0.15 percent chlorhexidine solution for washing twice daily beginning 20 hours after surgery and continuing for seven days. These medications should be taken in addition to a 0.15 percent chlorhexidine solution for washing twice daily. In addition to these drugs, you will be instructed to wash your hands twice day with a solution of chlorhexidine that contains 0.15 percent. Following the administration of a local anesthetic, the surgical procedure may then be carried out either on the buccal side of the mouth or the palatal side of the mouth, depending on the sort of movement that has to be carried out. When doing a deep cortectomy, the surgeon will remove not just the cortical bone but also a large portion of the cancellous bone. On the other hand, they do not in any manner influence the cortex that is opposite to the implant, nor do they allow for any change in the position of the implant. An incision known as a palatal sulcular incision will be created in the patient's gums during the surgical process known as palatal side surgery. During this procedure, the teeth that are in close proximity to the implant will also be incised. In addition to this, a mucoperiosteal flap will be mirrored in order to expose the alveolar bone. This flap will have its complete thickness taken into account. This cut is made along the axis of the proposed relocation, and one vertical deep corticotomy incision is conducted across the whole of the implant on both sides. This is achieved while preserving a safe distance between the implant and the teeth that are situated in close proximity to it in the mouth. The two vertical incisions need to grow increasingly closer together as they advance toward the peak of the structure in order to avoid blocking the flow of movement and prevent the structure from collapsing. Following this, a third ultrasonic incision will be created in the subapical apex region of the implant.
The process is now finished after this step. This cut connects the two vertical incisions that came before it. the incisions were done in the previous step. During surgical operations that are conducted on the buccal side of the mouth, ultrasonic incisions are produced. This side of the mouth is referred to as the buccal aspect of the mouth. It is possible to make the incision for the full-thickness mucoperiosteal flap at the junction of the connected gingiva. This will allow the flap to cover the whole thickness of the mucoperiosteum. Because of this, the flap will be able to span the whole thickness of the mucoperiosteum. Because of this, the implant's soft tissue connection will be maintained, and at the same time, recession will not occur.
Requirements after surgery
As soon as the procedure is finished, a continuous heavy orthodontic loading of between 140 and 250 g is applied to the implant along the same axis as the relocation. This loading is intended to move the implant into its new position. It is crucial that the orthodontic pressures do not go beyond the anchoring value of the teeth that are next to the affected teeth. Sutures are often removed after a week and a half has passed after the procedure.
Once every two weeks, the patient will have an appointment with the orthodontist to have the traction reactivated. This will continue until the process of relocation has been completed. One may see a difficult implant osseous movement somewhere between one and twenty-five days after the procedure. After the implant has been relocated to the correct position, a new arch wire will be placed next to it over a period of time ranging from three to seven months in order to monitor the advancement. After the appliance has been removed, the prosthodontic restoration may need to be updated (if this is necessary) in order to get an aesthetic result that is more to the patient's liking.
Dental computed tomography
Computed tomography is carried out immediately following the conclusion of the relocation project that was carried out with success. Cloud-Compare is the name of the piece of software that is used in order to complete the task of doing a three-dimensional superimposition comparison of these data with the presurgical computational tomography. This comparison is carried out in order to ensure that the patient will have the best possible surgical outcome. Data are obtained in each of the three dimensions throughout the process of carrying out the orthodontic bone stretching procedure. These data may be used to manage the movement of the implant, and they can also be used to quantify the quantity of bone that is being stretched.
Interventional processes of study
Class 1 samples of study
Patients expressed a wish to have the diastema in their maxillary incisors closed. Patients were in fantastic overall condition and had had a dental implant in their jaw about 7 years before. Both the clinical and radiological evaluations confirmed the existence of healthy soft tissues as well as an Osseo implant that was flawlessly integrated and had been used to effectively replace the right maxillary central incisor. Both examinations were successful. The orthodontic treatment was unable to reposition the implant, therefore the setup revealed a major malposition that did not permit the possibility of a new prosthetic restoration. This eliminated the prospect of a new prosthetic restoration being possible. The protrusion of the maxillary and mandibular incisors was expected to be reduced by following the prescribed orthodontic treatment plan. For the patient's appearance to return to normal, either repositioning the implant or removing it entirely was required. The primary stage in the treatment management was to address the mandibular incisor protrusion by avulsing the right mandibular central incisor, which was necrotic and had a very black enamel. This was done in order to address the mandibular incisor protrusion. The tooth was extracted in its entirety as a result of this procedure. After that, it was necessary to bridge the gap in the lower jaw as well as the maxillary anterior diastema, and in the end, the implant either required to be relocated or it was extracted. Orthodontic preparation to close the mandibular extraction space and the maxillary incisor diastema was done with a.020x.030 stainless steel wire on the maxilla, excluding the implant, and with a.021x.030 SSW in the lower arch. Both of these wires were placed on the maxilla. This was carried out in order to accomplish the goals that were set. After the teeth were realigned, it was decided that the site of the implant was not favorable to a new prosthetic rehabilitation, and this was validated. This conclusion was reached after it was established that the implant could not be moved. In spite of the fact that the patient already had acceptable osseointegration of the implant and a suitable prosthetic crown, an orthodontic bone stretching technique was nevertheless advised to them as the best course of action. Ultrasonic incisions were made on the palatal side in preparation for the repositioning of the implant by an anterior-to-posterior movement. Right away, orthodontic forces were used in order to move the implant towards the palatal direction once the flap had been closed. In order to apply these stresses, an elastic chain was attached to the implant and the arch wire, and 5 ounces of intermaxillary elastics were also used. The patient was responsible for switching out the elastics twice per day, while the orthodontist was responsible for reactivating the elastic chain once per week for the first month, and then once every 20 days following that. After the first 75 days of therapy, the implant crown was aligned with the incisors that were around it, and after the subsequent 75 days of treatment, the relocation result was fixed with a.025x.030 SSW. It was determined that the prosthetic crown would be kept, and a permanent retainer would be bonded to the front of the upper arch to hold it in place. After therapy had been completed for 18 months, the teeth's alignment and general look were examined and found to be unchanged.
Class 2 samples of study
They had an open bite face pattern, were in good health, and had no problems that would impede surgery. 11 months after the ankylosed tooth was extracted, the implant was Osseo integrated and surrounded by healthy soft tissues. The gingival line alignment was not maintained during implant placement, and the condition deteriorated over time to the point where a screw-retained restoration couldn't be employed. Orthodontic therapy and bone stretching were indicated to straighten the maxillary teeth and move the implant in a screw-retained restoration-compatible position. This was done to avoid implant location worsening due to alveolar growth. During orthodontic preparation, a cosmetic interim crown was affixed. Tooth repair was too big; thus screw was inserted on buccal side. After orthodontic treatment for the malocclusion,.025x.030 SSW were placed on both arches and additional hooks on the lower arch. At the end of the preparation, a new interim restoration in the implant axis was produced. This restoration was anatomical. The maxillary arch wire was adjusted to accommodate the new temporary screwed crown in the implant axis. This was done to detect whether the implant was put incorrectly and to guide implant traction movement. One horizontal incision was made in the keratinized gingiva during surgery. This preserved the papillae and raised a fullthickness mucoperiosteal flap at the buccal location. Vertical ultrasonic corticotomies were done on either side of the implant. These corticotomies ascended toward the incisal margin underneath the remaining soft tissues. Horizontal osteotomy connects two vertical osteotomies apically. To regulate the front teeth's position, a trans-palatal anchor was implanted. Immediately after surgery, an elastic chain was employed to create constant orthodontic traction. The system was completed by attaching an inter-maxillary elastic to the implant crown's bonded bracket and the lower arch wire hooks. Adjusting the trans palatal arch improved implant mobility during traction. After 75 days of traction, the implant and provisional crown were placed, and the space was filled. The 75-day stabilization featured a final.025 x.030 SSW. After removing the orthodontic equipment, a retainer and final restoration were bonded. Before the twisted zirconium rehabilitation, this was done.
Class 3 samples of study
Patients were referred so that the infraocclusion on the right maxillary first incisor may be corrected with a prosthodontic restoration. These individuals have been treated by implant treatment a significant amount of time ago. They did not offer any risks associated with the surgical treatment and were in excellent overall health; nonetheless, they smoke a lot and have made the decision to cut down on their habit in the near future. At the time of the clinical examination, the patient was found to have chronic periodontitis, the right maxillary first incisor had been replaced with an implant with infraocclusion, and the patient had a crown that had a slight palatal position. Both the soft and hard tissues close to the implant, as well as the osseointegration, were stable. The face skeletal pattern exhibited norm divergent characteristics. The exact implant location came about as a result of several years of uninterrupted alveolar development. Given the favorable location of the palatal implants at the time of the operation, which occurred many years in the past, the correct axis was preserved, and there was no buccal side effect movement. A fresh restoration with screws might have been done, but the prosthetic rehabilitation required to adjust for the infraocclusion would have produced an unsatisfactory outcome, with a crown that was excessively long and an erroneous gingival line alignment. For this reason, periodontal therapy was planned first before orthodontic preparation and implant relocation at the appropriate level utilizing the orthodontic bone stretching approach. Before surgery, orthodontic preparation consisted of aligning the patient's teeth but omitting the implant, and a.025 x.030 SSW was put on the maxillary and mandibular arches using a special appliance. Following the completion of the alignment phase, the infraocclusion on the incisor prosthodontic crown was significantly exacerbated as compared to the incisal edge of the surrounding teeth. An overlay nickeltitanium arch wire with a thickness of.016 was put on the maxillary teeth, including the implant, just before surgery. The orthodontic bone stretching operation was conducted on the buccal side, and the implant's soft tissue connection was preserved throughout the process. Immediately after the surgical procedure, orthodontic pressures were administered. The patient was checked in with the orthodontic practitioner once every 15 days for traction reactivation. The movement was finally halted after 65 days of orthodontic traction treatment. A fresh operation was going to be performed on the palatal side. In the immediate aftermath of the surgical procedure, orthodontic traction was given along the intended axis. The mobility of the implant was enabled by the stretching of the bone. After the tooth had been stabilized, a new crown and a retainer were glued onto it.
Results
Throughout the whole of the orthodontic traction therapy and surgical procedures that were carried out, there were zero incidences of any kind of difficulty. According to the results of the control computed photographic examination, none of these three patients had any issues with the osseointegration or displacement of their implants. We were able to depict the movement that occurred as a result of the bone stretching events by superimposing images that were taken both before and after the operation. In the first example, it was determined that a new prosthodontic restoration was not required after the implant was moved. This conclusion was reached about class 1. After doing some research and thinking over the situation, we came to this conclusion. A change to the look of the face and grin was made possible via the use of orthodontic therapy and orthodontic bone stretching.
When viewed in the palatal direction, the mobility of the implant was measured to be 0.56 millimeters at the apex and 6.56 millimeters at the incisal edge. These measurements were taken. The implant that was located in class 2 was successfully shifted after the patient underwent traction for a period of three months, and the final prosthodontic restoration was completed. The calculated photographic superimpositions showed that there was movement of 4 millimeters in the palatal direction at the junction of the implant and the abutment, and 7 millimeters at the incisal edge of the prosthetic tooth. Even though there was a lot of resistance to movement in the occlusal direction in instance 3, the implant was nevertheless moved after a period of five months (6 months after the second surgery). It was determined that the degree of displacement at the incisal edge was 4 millimeters, and a recent prosthodontic repair was performed in order to generate an esthetic outcome that was more desirable. Despite the provision of preventative periodontal therapy, the management of plaque did not prove to be very fruitful. Show the numbers (Figures 1 to 9).
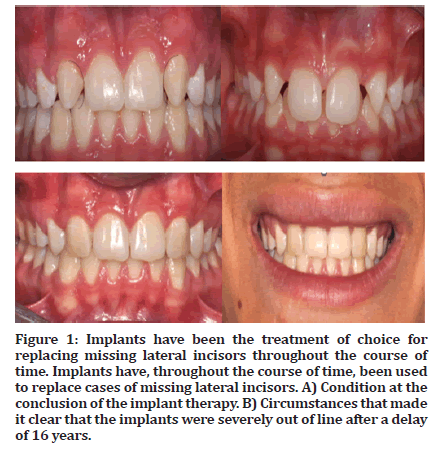
Figure 1: Implants have been the treatment of choice for replacing missing lateral incisors throughout the course of time. Implants have, throughout the course of time, been used to replace cases of missing lateral incisors. A) Condition at the conclusion of the implant therapy. B) Circumstances that made it clear that the implants were severely out of line after a delay of 16 years.
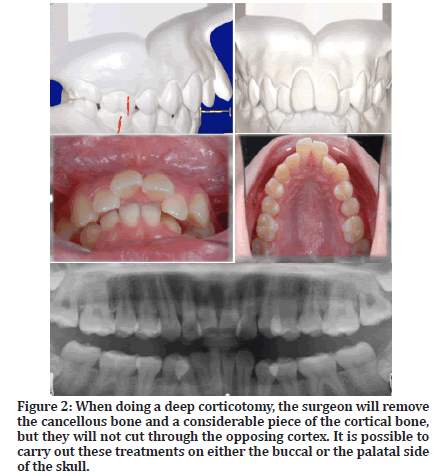
Figure 2: When doing a deep corticotomy, the surgeon will remove the cancellous bone and a considerable piece of the cortical bone, but they will not cut through the opposing cortex. It is possible to carry out these treatments on either the buccal or the palatal side of the skull.
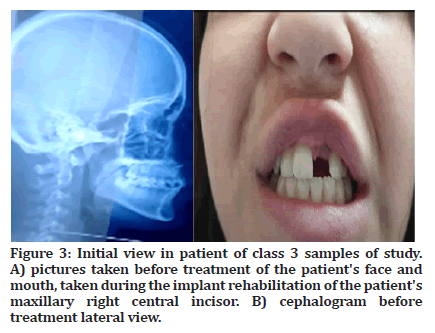
Figure 3:Initial view in patient of class 3 samples of study. A) pictures taken before treatment of the patient's face and mouth, taken during the implant rehabilitation of the patient's maxillary right central incisor. B) cephalogram before treatment lateral view.
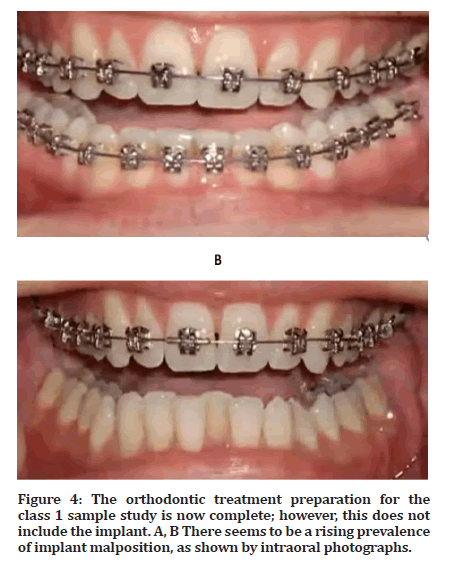
Figure 4:The orthodontic treatment preparation for the class 1 sample study is now complete; however, this does not include the implant. A, B There seems to be a rising prevalence of implant malposition, as shown by intraoral photographs.
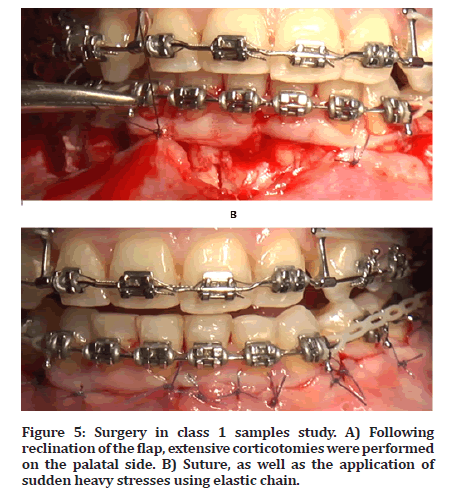
Figure 5:Surgery in class 1 samples study. A) Following reclination of the flap, extensive corticotomies were performed on the palatal side. B) Suture, as well as the application of sudden heavy stresses using elastic chain.
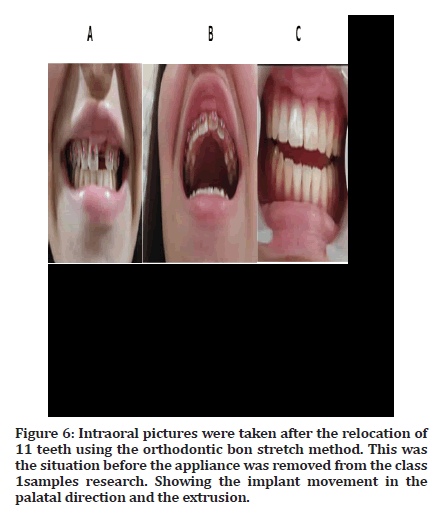
Figure 6:Intraoral pictures were taken after the relocation of 11 teeth using the orthodontic bon stretch method. This was the situation before the appliance was removed from the class 1samples research. Showing the implant movement in the palatal direction and the extrusion.
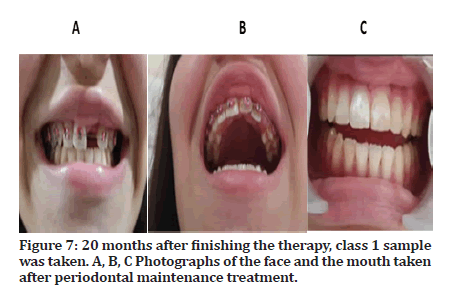
Figure 7:20 months after finishing the therapy, class 1 sample was taken. A, B, C Photographs of the face and the mouth taken after periodontal maintenance treatment.
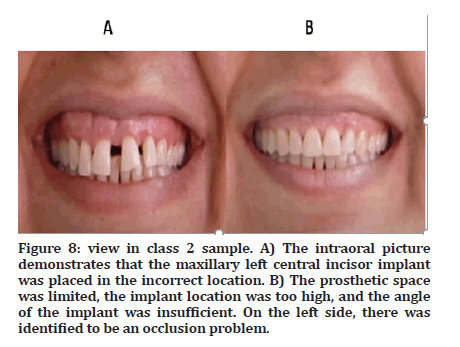
Figure 8:view in class 2 sample. A) The intraoral picture demonstrates that the maxillary left central incisor implant was placed in the incorrect location. B) The prosthetic space was limited, the implant location was too high, and the angle of the implant was insufficient. On the left side, there was identified to be an occlusion problem.
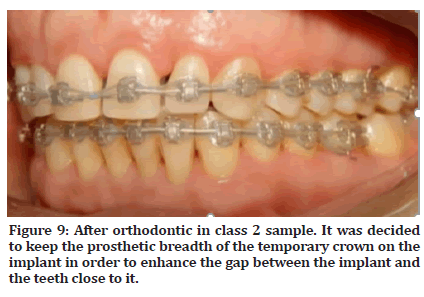
Figure 9:After orthodontic in class 2 sample. It was decided to keep the prosthetic breadth of the temporary crown on the implant in order to enhance the gap between the implant and the teeth close to it.
Discussion
Incorrectly positioned implants may be caused by surgical issues, such as an inability to put the implant properly or an initial insertion error. Front jaw implants complicate orthodontic treatment. Any tooth, except the implant, may be moved. Infraposition occurs when there is insufficient alveolar growth surrounding an osseointegrated implant compared to neighboring teeth, which are still developing verticall. Inflation. Buccal describes infraposition. Implant buccalization may result. Segmental osteotomies effectively moved implants, according to studies. This operation will reposition and secure the bone implant block. Bone transplants may create mobility issues. The trans-palatal device was modified to minimize inhibiting palatal mobility of temporary screwed crown implant relocation with osteotomy to stabilize unrestorable malpositioned implants. Malpositioned implants were fixed. Stacchi et al's 15-case Italian investigation enabled this modification. Alveolar vascularization is required. Bone maintenance requires soft tissue connection. Soft tissue stretching may impede vascularization and implantosseous mobility. Stopping minute block movements might impede healing. The implant must be put correctly to be permanently fastened after surgery. Distraction osteogenesis may assist. After osteotomies and callus formation, rigorous strength training delays block mobility, resulting in soft and hard tissue augmentation. This is progressive augmentation. Managing each region's block will be difficult. The distractor restricts movement to one axis. This limitation creates improper distraction vectors [20-23]. Using specialized equipment to facilitate mobility is challenging and costly. The orthodontic bon stretch technique moves ankylosed teeth and implants. Bon stretch exclusively osteotomizes the buccal (or palatal) alveolar bone. Bone and connective tissues retain vascularization. Partial osteotomies immobilize implantbone, therefore block stabilization is unneeded. Deep corticotomies are less invasive than complete osteotomies and lower block resistance. Frequent full osteotomies. Osteotomy is complete. Orthodontic force can't move an osseointegrated implant because dental arch anchoring resistance is smaller. Because of orthodontic bone stretch, implant repositioning may be done without ligaments. Tooth displacement develops after two or three weeks of traction, as with ankylosed teeth. Orthodontic bone stretch involves implant anchors. It's evident. Orthodontic preparation is key to controlling implant tissues, according to our study. The patient's neighboring teeth need at least 3 mm of room for deep corticotomy incisions and implant repositioning. Best results are attained by aligning orthodontic traction with the vertical incisions, which should converge toward the apex. If the loading force is along a different axis or the corticotomies converge, the implant won't move [24]. To prevent bone healing and increase remaining palatal or buccal bone, use fast, continuous force. Corticotomy promotes alveolar bone turnover in animal studies. Indeed. Orthodontic bon stretch employs piezo. Piezo cuts are small and accurate highly recommended. Compared to standard instruments, piezotomes improve bone activity. Ultrasonic cutting helps orthodontic bone stretching. Clinicians agree. This requires research. Class 3 immobility needed more surgery. Nicotine may have altered this patient's bone stretch technique movement. The patient's habitual smoking supports this. Smoking slows bone turnover and increases orthopedic surgical complications. Smoking increases treatment time and tooth movement. Smoking slows tooth and bone mobility. Bone stretching uses fast, sustained stresses, unlike bone distraction. Due to the partial bone incisions, a callus is not required. Orthodontic appliance movement uses lower pressures (150–200 g) and may move in either direction. This case series exhibited osseointegration despite boneimplant movement. Animal models and human patients using osseointegrated implants as orthodontic anchors had no periimplant bone alterations. Both were similar. Animals were given 120, 1900, and 2800 grams of osseointegrated implant pressure. The experiment was stressed. Loading force didn't affect bone-to-implant contact (osseointegration). After 11 weeks of pressure, no clinical implant displacement occurred, and periimplant probing never surpassed 3mm. Orthodontic pressures of 200 to 600 g don't hinder osseointegration or bone-to-implant contact false. In an animal model, increasing orthodontic force from 120 to 330 g every 21 days improves osseointegration. Continuous, regulated orthodontic force achieves this [25-28]. Becker and colleagues used an animal model to illustrate that stressed implants may migrate through bone. The implants moved. Implant movement under orthodontic forces causes cortical bone stretching [29-30].
Conclusion
The orthodontic bone stretch method appears like it might be fascinating since it gives surgeons another option for the repair of implants that are placed in the wrong location. The capability of managing motions in any and all directions enables the implant to be driven towards the desired end location. This method may be paired with orthodontic therapy, which is often required for the cosmetic rehabilitation of anterior implants that are located in the incorrect position. To evaluate the predictability of the orthodontic bone stretch operation in comparison to osteotomy and distraction, more controlled studies would be very helpful and would need to be carried out.
References
- Bousquet P, Barthélemi S, Artz C, et al. The application of orthodontic bone stretching for correcting malpositioned dental implants Head Face Med. 2021; 17:1-1.
- Chan TK. Use of interdental distraction osteogenesis for orthodontic tooth alignment and correction of maxillary hypoplasia: A case report. Br J Oral Maxillofac Surg 2003; 41:185-187.
- Shetye PR. Update on treatment of patients with cleft-Timing of orthodontics and surgery. Semin Orthod 2016; 22:45-51.
- Stacchi C, Barlone L, Rapani A, et al. Modified orthodontic bone stretching for ankylosed tooth repositioning: A case report. Open Dent J 2020; 14.
- Ramesh A, Vellayappan R, Ravi S, et al. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile–A case series. J Indian Soc Periodontol 2019; 23:290.
- Xie Y, Zhao Q, Tan Z, Yang S. Orthodontic treatment in a periodontal patient with pathologic migration of anterior teeth. Am J Orthod Dentofacial Orthop 2014; 145:685-693.
- Motro M, Will LA. Success with TADs: Evidence and experience. Tempor Anchorage Devices Clin Orthod 2020: 747-755.
- Baumgaertel S. Three top indications for the use of orthodontic mini screws. Information from Orthodontics & Orthodontics 2020 ;52:197-202.
- Tang Z, Gao Y, Chen Y, et al. Development of a systematic course on orthodontic Temporary Anchorage Devices (TADs) for orthodontic residency program. Res Square 2021.
- Camci H. Vakaya Uygun Mini Vida Seçimi. Turkiye Klinikleri J Dent Sci 2017; 23.
- https://acikbilim.yok.gov.tr/handle/20.500.12812/63689
- Giudice AL, Rustico L, Longo M, et al. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J Orthod 2021; 51:199-216.
- Watted N, Witt E, Bill JS. A therapeutic concept for the combined orthodontic surgical correction of angle Class II deformities with short‐face syndrome: Surgical lengthening of the lower face. Clin. Orthod Res 2000; 3:78-93.
- Epistatu D, Baco A, Dogioiu F, et al. A complex treatment with orthodontic modification of the alveolar axis for implant insertion in a patient over 65 years of age with a thin periodontal biotype. Rom J Stomatol 2021; 67:240.
- Yadav LA, Mattoo KA, Kapoor AD, et al. Factors associated with post core correction of malpositioned teeth. Int J Res Med Sci Technol 2015; 1:3-5.
- Shetye P. Orthodontic management of patients with cleft lip and palate. APOS Trends Orthod 2016; 6:281.
- Lohmiller RM. Modified Grassline technique for orthodontic space closure. Eur J Esthet Dent 2006; 1:30-51.
- Miller Jr PD, Allen EP. The development of periodontal plastic surgery. Periodontol 1996; 11:7-17.
- Machado AW, MacGinnis M, Damis L, et al. Spontaneous improvement of gingival recession after correction of tooth positioning. Am J Orthod Dentofac Orthop 2014; 145:828-835.
- Alwan AM, Tavakol AJ. Investigating the protective role of rhodanese enzyme against cyanide, the cytotoxic by-product of amygdalin, in HDF and L929 Cell Lines. Lett Drug Des Discov 2022; 19.
- Alwan AM, Afzaljavan F, Tavakol Afshari J, et al. The impact of CYP19A1 variants and haplotypes on breast cancer risk, clinicopathological features and prognosis. Mol Genet Genomic Med 2021; 9:1705.
- Alwan M, Afzaljavan F. Significance of the estrogen hormone and single nucleotide polymorphisms in the progression of breast cancer among female. Arch Razi Inst 2022; 77:943.
- Alwan AM, Afshari JT. In Vivo growth inhibition of human caucasian prostate adenocarcinoma in nude mice Induced by amygdalin with metabolic enzyme combinations. Biomed Res Int 2022.
- Eschler JO. The functional anatomy of the masticatory system in functional jaw orthopaedics. Eur J Orthod 1969; 219-230.
- Allen EP. Surgical crown lengthening for function and esthetics. Dent Clin N Am 1993; 37:163-179.
- Grayson BH, Santiago PE. Treatment planning and biomechanics of distraction osteogenesis from an orthodontic perspective. Sem orthod 1999; 5:9-24.
- Hanson PR, Melugin MB. Orthodontic management of the patientundergoing mandibular distraction osteogenesis. Sem orthod 1999; 5:25-34.
- de Avila ÉD, de Molon RS, de Barros-Filho LA, et al. Correction of malpositioned implants through periodontal surgery and prosthetic rehabilitation using angled abutment. Case Rep Dent 2014.
- Voudouris JC, Woodside DG, Altuna G, et al. Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 2. Results and conclusions. Am J Orthod Dentofa Orthop 2003; 124:13-29.
- Stansbury CD, Evans CA, Miloro M, et al. Stability of open bite correction with sagittal split osteotomy and closing rotation of the mandible. J Maxillofac Surg 2010; 68:149-59.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Aseel Niema Hafith*, Waleed Shallal and Bakir Ghanem Murrad
Department of Dentistry, Kut University College, Kut, Wasit, IraqCitation: Aseel Niema Hafith, Waleed Shallal, Bakir Ghanem Murrad, Orthodontic Sectors Applications for Wrong Positions of the Ankylosed Teeth by Dental Implant, J Res Med Dent Sci, 2023, 11(2):74-81.
Received: 01-Feb-2023, Manuscript No. jrmds-23-88715; Accepted: 03-Feb-2023, Pre QC No. jrmds-23-88715; Editor assigned: 03-Feb-2023, Pre QC No. jrmds-23-88715; Reviewed: 17-Feb-2023, QC No. jrmds-23-88715; Revised: 21-Feb-2023, Manuscript No. jrmds-23-88715; Published: 28-Feb-2023
