Case Report - (2023) Volume 11, Issue 1
Osteogenic Sarcoma: A Case Report
Pranali Wagh1*, Kanchan Bokade2, Samruddhi Gujar2 and Sonali Waware2
*Correspondence: Pranali Wagh, Department of Child Health Nursing, Smt Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India, Email:
Abstract
Background: Osteosarcoma (also called osteogenic sarcoma) is the most common type of cancer that starts in the bones. The cancer cells in these tumors look like early forms of bone cells that normally help make new bone tissue, but the bone tissue in an osteosarcoma is not as strong as that in normal bone. Aim: To know general idea about the condition of the disease. Objectives: Exploring knowledge of pharmacology, management of medicine, surgery and nursing. Result: Now my patient is discharge but he will come for follow up after 1 month. Conclusion: In this study, we mainly focus on expert surgical management and excellent nursing care helped in managing the complicated case very nicely. Over all the patient response was positive for conservative and nursing management and after treatment the patient was discharged without any postoperative complications and satisfaction with full recovery.
Keywords
Access, Aortic occlusion, Aortoiliaccclusion, Iliac occlusion
Introduction
Osteogenic Sarcoma (OS) is a primary malignant tumor of the bone, derived from primitive bone forming mesenchyme and characterized by the production of osteoid tissue or immature bone by the malignant proliferating spindle cell stroma [1,2]. Although primary bone tumors are rare in childhood, they are the sixth most common malignant neoplasms in children; in adolescents and young adults, they are the fourth most common malignant neoplasms, exceeded only by leukaemia, lymphomas and brain tumors. There are 600 new cases per year reported in the United States but it occurs at a much lesser rate in Singapore. Its incidence rates among individuals under 24 years were 3.9 per million in men and women in Singapore [3]. A Singapore cancer registry report by Shanmugaratnam K, et al. cites the incidence of OS over a 20 years period in Singapore as 20 cases per year [1].
Case Presentation
Here we are mentioning a very rare surgical case of osteogenic sarcoma disease. In this case, on physical examination and investigation 7 days was diagnosed osteogenic sarcoma. Although no premedication was administered, parental separation was peaceful. The operation room temperature was maintained at 20 degree celsius. The surgery is open biopsy from right proximal humures has been planned. Patient admitted in ortho ICU and surgery was planned during hospital stay treatment was going on i.v. fluids:
• 2 ns 500 ml @ 90 ml/hour.
• 2 rl 500 ml @ 90 ml/hour.
• Drugs: Injection pantoprazole 40 mg i.v. once daily.
• Antibiotic: Injection ceftriaxone+sulbactum 1.5 gm
i.v. twice daily × 5 day.
• Pain control: Injection diclofenac 75 mg, 50 mg IM
thrice daily.
• Other medications: After NBM release.
• Tab vitamin C 500 mg twice daily.
• Tab calcium 500 mg twice daily.
• Tab chymotrypsin 1 tab thrice daily.
Case history
A surgical case was taken by Acharya Vinoba Bhave Rural Hospital, DMIMS, Sawangi, Wardha, Maharashtra. After surgery, this complicated case was taken care nicely by the hospital because of expert surgical team management and excellent nursing care [2].
Patient information
We report Lalbabu Ojha 67 years male was admitted in ortho ICU presenting with complaint of pain and swelling over right shoulder since 1 month. After investigation He was diagnosed osteogenic sarcoma disease. Patient came to casualty on 10/09/2021 at 1.15 pm with chief complaint of pain and swelling over right shoulder for which he was admitted in ortho ICU in AVBRH after he under investigation such as CBC, CT chest, 20 ECO etc.
COVID-19, virus not identified, clinically epidemiologically diagnosed COVID-19, probable COVID-19, suspected COVID-19 general examination was done. He was diagnosed as aorto iliac occlusive disease.
Patient and his son is the bread winner of the family. These family income is 40000/- per month. Her family members had no any complaints of communicable and non-communicable diseases. He maintained good interpersonal relationship with family members and relatives and neighbors also. But due to this condition he had developed symptoms like irritability, anxiety and restlessness and found it difficult in bonding with his family. At the time of admission patient doesn’t have communicable and non-communicable disease.
On admission his vital sign were normal but systolic and diastolic blood pressure was 120/80 mm of Hg, while cardiac inspection and percussion it was distended. Overall this condition was managed by administration of intravenous fluid and antibiotic treatment. Blood investigation was done [3].
Physical examination: His physical examination was done.
General examination
General appearance and behavior
• Body built–moderate.
• Nourishment–moderately nourished.
• Gait and posture–erect.
• Grooming and hygiene–well maintained.
• Rapport–established.
Mental status
• Consciousness–conscious.
• Orientation–oriented to time, place, person.
• Attention–attentive.
General parameter
• Height–159 cm.
• Weight–35 kg.
• BMI–20.
Vital sign
• Temperature–98.6 degree F.
• Pulse–86 beats/min.
• Respiration–22 breath/min.
• Blood pressure–110/70 mmHg.
Head to foot examination
Scalp
• Symmetry–symmetrical.
• Scars–not present.
Face
• Symmetry–symmetrical.
Eye
• Eyebrows–symmetrical.
• Eyelids–no inflammation.
• Pupil–equally reacting to light and accommodation.
• Vision–normal.
Nose
• Symmetry–symmetrical.
• Deviated nasal septum–not present.
• Discharge/bleeding–not present.
Ears
• Symmetry–symmetrical to eyelids.
• Discharge–not present.
• Bleeding–not present.
• Hearing acquity–normal.
Mouth and pharynx
• Halitosis–not present.
• Chilosis–not present.
• Teeth–white color.
• Pharyngitis–not present.
Neck
• Range of motion–normal.
• Lymph node–not enlarged.
Chest
• Inspection–no scars, lesions found.
• Palpation–no lump or nodules found.
• Percussion–no fluid or gas collection present.
• Auscultation–S1+S2 heard.
Abdomen
• Inspection–no scars, lesion found.
• Palpation–rise of local temperature present.
• Bony tenderness ellicited over right shoulder and
proximal humerus.
• Shoulder ROM restricted due to pain active finger and
thumb rom distal circulation intact.
Diagnostic assessment
The laboratory test were conducted and results were: Hemoglobin 12.5 gm/dl (13-15.5 gm/dl) and total RBC count was 6.03, total WBC count 14000, total platelet count 3.35, urea 26, creatinine 0.2, sodium 137; potassium 3.6, total biliribun level is 0.8 globulin (calculated parameter) is 2.0 [4].
CT chest
Extensive calcification and adjacent extra plural fat thickening along the pleura on postro lateral aspect in right lower pnemothorax, along with mild volume less in adjoining right middle and lower lobe sequel to old healed infective pleural pathology.
Centrilobular emphysema in bilateral upper lobes and part of apical basal segment of left lower lobe (Figure 1).
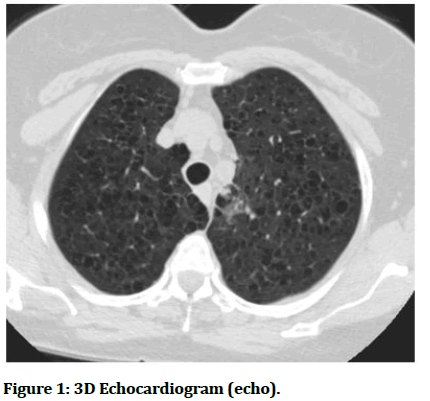
Figure 1: 3D Echocardiogram (echo).
• Hypertensive heart disease.
• Mild concentric left ventricular hypertrophy.
• Good biventricular function LVE F–60%.
• Grade I IV diastolic dysfunction.
• No clot or effusion, no co-relation of aorta.
• No pulmonary hypertension.
Bilateral lower limb arterial Doppler
Findings are highly suggestive of moderate right aortoiliac narrowing and significant narrowing at proximal common femoral artery level suggested CT aorta iliac and lower limb angiograph.
Pre-operative care
Weight monitored was done as per doctors ordered and maintained intake and output strictly. Doctors tried to treat this condition with the help of conservative management i.e. patient admitted in ortho ICU and surgery was planned during hospital stay treatment was going on injection heparin 1000 IU/hr, 2 ml/hr IV, Tab azee 500 MG OD, inj 0.1 mg IV OD, tab folite 5 mg, OD before start surgical operation preparation written consent was taken by patient or patients relative. Patient is NBM for surgery before 6 hour. Physical and psychological preparation was done of patient preoperatively. All these condition were very threatful to patient.
Surgery surgical bypass
The most common minimally invasive treatment is the placement of the slent in your aorta an iliac arteries. This procedure is commonly done at same time as acalcuter directed angiogram. Right iliac artery angioplasty has been planned.
Post-operative care
Post operatively patient shifted in surgery ICU; semi fowler’s position was given, 4 hourly Ryle’s tube aspiration. Post operatively continuous cardiac monitoring was done, SPO2 monitored, injection ceftriaxone 200 mg IV BD, injection amikacin 70 mg OD, injection pan 20 mg OD, injection Emset, injection PCM 100 mg IV TDS, Syrup augmentin duo 25 ml BD. On day 2nd patient shifted in ward.
Nursing management
Postoperatively patient was under strict observation of on duty staff. Intravenous fluid administered as per calculated. Observed and record the character of the drainage postoperatively. Care of wound and daily dressing was done. Drainage care was taken and maintains intake and output 2 hourly. Vital signs were recorded strictly. Overall her response was positive for treatment and patient condition too improved progressively. Excellent nursing care was given of patient reported to nursing staff that, patient was very satisfied about nursing care. Complete discharge procedure was explained by nursing staff to the patient family members along with medication prescribed at home as advised by surgeon. The patient was discharged after 14 days without any complications.
Patient visited regularly at OPD for his daily routine checkup, during this period routine checkup was done and he had no any complaints, therefore no furthermore evaluation was found [5].
Discussion
This was a very rare surgical case of osteogenic sarcoma disease, Lalbabu Ojha 67 years male was admitted in MICU presenting with complaint of pain in right lower limb since 1 month. After investigation He was diagnosed aortoiliac occlusive disease. Patient came to casualty on 27/12/2020 at 1.15 pm with chief complaint of right lower limb for which he was admitted in MICU in AVBRH after he under investigation such as CBC, CT chest, 20 ECO etc. COVID-19, virus not identified, clinically epidemiologically diagnosed COVID-19, probable COVID-19, and suspected COVID-19. General examination was done. He was diagnosed as aortoiliac occlusive disease. Although no premedication was administered, parental separation was peaceful. The operation room temperature was maintained at 20 degree celsius. The surgery is peripheral angiography and right iliac artery angioplasty has been planned. Patient admitted in medicine ICU and surgery was planned during hospital stay treatment was going on injection heparin 1000 IU/hr, 2 ml/hr IV, tab azee 500 MG OD, injection 0.1 mg IV OD, tab folite 5 mg OD.
The report is unusual case of acute MI and aortoiliac occlusive disease at the same time as type I. This patient is likely to have a pre-existing severe peripheral arterial disease that has never diagnosed or symptomatic due to his lifestyle. Patient having history of chewing tobacco and obesity has contributed. The factors are responsible for that, percutaneous trans luminal angioplasty was done and that time vascular disease was detected. In STEMI setting aortoiliac occlusion developed because of there are two leading hypothesis, it is responsible for both out patient had pre-existing peripheral arterial disease, during angioplasty to know the demonstrated by difficulty of gaining femoral access. Firstly sudden osteogenic sarcoma because the rupture of pre-existing plaque and secondly the catheter are used that the procedure may have dislodged a thrombus that triggers an immediate aortoiliac occlusion; or catheters that travel through already severely stenosed abdominal aorta may have caused complete obstruction and immediate symptoms distally. In closing, there are two important thoughts that we leave for interventional cardiologists to consider. The first is to be careful when handling the wire and catheter at all times and, even more so, in patients with a history of peripheral vascular disease or risk factors indicating its presence. In this case, the only significant risk factors were obesity, tobacco abuse, sedentary lifestyle and acute STEMI presentation. Although no reported history of claudication and femoral pulse were intact on presentation, distal lower extremity pulse decreased. Decreased distal lower extremity pulses should indicate the presence of pre-existing peripheral vascular disease and alert wire and catheter manipulation. Although it is still unclear what precipitated the aortoiliac occlusion of this patient, it is likely that the actual catheter caused a physical obstruction of the already severely stenosed aorta [6].
Conclusion
The report is unusual case of acute MI and aortoiliac occlusive disease at the same time as type I. This patient is likely to have a pre-existing severe peripheral arterial disease that has never diagnosed or symptomatic due to his lifestyle. Patient having history of chewing tobacco and obesity has contributed. These factors are responsible for symptomatic presentation, it can occur during transluminal percutaneous period.
The presence of significant peripheral vascular disease, significant cardiac risk factors and/or difficulty in accessing the femoral artery should be advised by transfemoral approach during percutaneous transluminal angiography. This approach can precipitate aortoiliac occlusion and/or thromboembolism to the lower extremities. We encourage interventional cardiologists to:
• Take extra caution when handling wire and catheter.
• Strongly consider using a transradial.
Acknowledgement
The author thanks to Dr. Seema Singh, professor and principal, Smt. Radhikabai Meghe Memorial College of Nursing. Datta Meghe Institute of Medical Sciences, Sawangi, Wardha for her timely support and valuable suggestions. Mrs. Vaishali Taksande, professor, Department of OBGY, Mrs. Jaya Gawai, Dean, Department of MHN, Mr. Bibin Kurian HOD of child health nursing DMIMS (DU) for her continuous support and valuable suggestions. The author also thanks Mrs. Maurya, professor, department of child health nursing. For her timely supports. The Authors are also grateful to authors/editors/publishers of all those articles, journals and books, from where the literature for this article has been reviewed and discussed.
Ethical Approval
Not applicable.
Patient Inform Consent
While preparing case report and for publication patient’s informed consent has been taken.
Conflict of Interest
The author declares that there are no conflicts of interest.
Funding
Not applicable.
Reference
- Leriche R, Morel A. The syndrome of thrombotic obliteration of the aortic bifurcation. Ann Surg 1948; 127:193–206. [Crossref][Googlescholar][Indexed]
- Kappert A. Pathogenesis and clinical aspects of the acute occlusion syndrome. Verh Dtsch Ges Inn Med 1972; 78:544–550. [Googlescholar][Indexed]
- Surowiec SM, Isiklar H, Sreeram S, et al. Acute occlusion of the abdominal aorta. Am J Surg 1998; 176:193–197. [Crossref][Googlescholar][Indexed]
- Iliopoulos JI, Howanitz PE, Pierce GE, et al. The critical hypogastric circulation. Am J Surg 1987; 154:671–675. [Crossref][Googlescholar][Indexed]
- Mahendrakar SM, Sandhu HS, Khan AH, et al. Leriche syndrome: Acute onset painful paraplegia of vascular origin with catastrophic consequences. J Clin Diagn Res 2017; 11:OD22–OD23. [Crossref][Googlescholar][Indexed]
- Olsofka JN, Carrillo EH, Spain DA, et al. The continuing challenge of fournier’s gangrene in the 1990’s. Am Surg 1999; 65:1156–1159. [Crossref][Googlescholar][Indexed]
Author Info
Pranali Wagh1*, Kanchan Bokade2, Samruddhi Gujar2 and Sonali Waware2
1Department of Child Health Nursing, Smt Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India2Department of Medical Surgical Nursing, Smt Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi, Wardha, Maharashtra, India
Received: 07-Nov-2022, Manuscript No. JRMDS-22-57055; , Pre QC No. JRMDS-22-57055 (PQ); Editor assigned: 10-Nov-2022, Pre QC No. JRMDS-22-57055 (PQ); Reviewed: 24-Nov-2022, QC No. JRMDS-22-57055; Revised: 08-Dec-2022, Manuscript No. JRMDS-22-57055 (R); Published: 18-Jan-2023
