Research - (2021) Volume 9, Issue 2
Parents View Regarding Various Influencing Factors on Child Behavior in the Dental Clinic
Prerna Jain and Deepa Gurunathan*
*Correspondence: Deepa Gurunathan, Department of Paediatric and Preventive Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
Paediatric dentists promote the dental health status of children and also provide health educational information and knowledge for parents. Parents’ oral health knowledge and good care practices are important in preventing premature loss of primary teeth and can effectively reduce the risk of future decay in permanent teeth. A cross-sectional study was conducted among parents who bring their children to dental clinics in Saveetha Dental College and Hospitals, Chennai. Parents completed a close-ended questionnaire within the treatment hours (72 parents). The questionnaire is divided into 4 separate categories. The questionnaire assessed parental views on the following 4parameters: dentist, dental clinical settings, dental treatments and child related factors. The data collected will be analyzed using descriptive statistics. This study shows that there are various influencing factors which drive a child to the dental clinic. Toothache accounts for 54% of the reasons a child visits the dental clinic. 51% of the children underwent restorative (filling) procedures, as we know that saving a tooth is more important than the removal of the tooth from the oral cavity. The most important aspect which is required for the success of a paediatric dentist is dependent not only on the technique applied and the skills but most importantly on the child and their parents. Thus, we would like to conclude that perception of parents among dental treatment plays the most significant role in a child's behaviour in the dental clinic.
Keywords
Paediatric dentist, Children, Influencing factors, Toothache, Dental caries
Introduction
Paediatric dentists promote the dental health status of children and also provide health educational information and knowledge for parents. According to the American Academy of Pediatric Dentistry (AAPD) and the American Academy of Pediatrics (AAP), a child should visit the dentist once in every six months after the presence of the first tooth or child’s first birthday [1]. A dental home can be defined as an ongoing relationship between dentist and patient, which includes all aspects of oral health care delivered in a comprehensive, continuously accessible, coordinated and family centered way [2]
Dental caries and periodontal diseases can be effectively prevented by plaque removal, which serves as a standard to evaluate oral hygiene [3]. Parents and guardians can be considered gatekeepers for the oral healthcare of children, by which their knowledge, belief and attitude on oral health may directly, or indirectly, influence early childhood oral health [4]. Understanding parental perceptions about early childhood oral health is important in order to develop effective preventive measures and treatment for the child since parent’s health beliefs, behaviours, and practices usually have a direct or an indirect influence on their children’s dental health [5]. In some cases, It has been reported that parents who are more likely to have positive attitudes towards dentistry and oral health were more likely to have children with better dental health [6]. It can also be believed that, parents who understand the importance of primary teeth are more likely to have children who do not have caries [7]. Another report says that parents’ positive dental attitudes resulted in children with fewer carious teeth, better oral hygiene, and having received more dental care [8].
Oral health plays a very important role in the general well-being of individuals, and parents' behavior and attitudes influence the oral health of their children [9]. Parents’ oral health knowledge and good care practices are important in preventing premature loss of primary teeth and can effectively reduce the risk of future decay in permanent teeth [10]. Early dental visits are also very effective and essential preventive practice for young children. It gives an opportunity for dental professionals to detect early caries lesions, evaluate dental development, provide anticipatory guidance and dietary counselling, and motivate parents towards adopting preventive behaviours [11]. Moreover, exposing children to the dental office at an early age helps them to adapt and become familiar with dental environments which possibly improves the likelihood of better behaviour and tolerance with future dental treatment [12].
Management of children in the paediatric clinic has become a complex balancing act which involves the child, parent and the dentist. To provide dental care for children good communication skills are necessary [13]. Paediatric dentists usually recommend behaviour guidance methods for a particular child depending upon their health history , dental needs, type of treatment required, special health care need, the consequences of no treatment, their emotional and intellectual development, the parents’ preferences, dentist’s preferences and skills [14]. Lack of cooperation in a child affects the successful completion and quality of necessary dental procedures as well as raises some degree of stress in the dentist. The management of children with noncooperative and disruptive behaviour in the dental clinic has seen to be a major challenge to the dental practitioners. Some children do not always accommodate plans designed for them as there are many factors which can influence the behaviour of children in the dental situation. Though some factors are not under the control of a clinician but knowledge of certain aspects and influences on a child's behaviour can be of major help in clinical practice [15].
Understanding parental perceptions on various factors influencing child behaviour in the dental clinic is crucial and it presents an opportunity to carefully work together and select the best treatment method to make the child’s visit as safe, effective and comfortable as possible.
Our department is passionate about child care, we have published numerous high quality articles in this domain over the past 3 years [16-34]. With this inspiration we planned to pursue research on parents perception regarding the factors influencing child behaviour in dental clinics.
Materials and Methodology
Participant selection
The data was collected from the parents who visited the paediatric dental clinic of Saveetha Dental College and Hospitals, Chennai for the dental treatment of their child and were requested to participate in the study. The parents who willingly agreed to participate in the study were included for analysis.
Questionnaire design and selection
A questionnaire was designed for the study to be answered by parents. The questionnaire was initially assessed among few parents and then it was modified according to the changes and corrections made by the parents according to their preferences. It consisted of personal details which included age and gender of the child & parent/guardian, address of the participant. Pertaining to this, the child’s dentist visit number was taken into consideration for the analysis. A specific identification number was given for each participant for better data collection.
The questionnaire consisted of 17 close ended questions. It was focused on 4 different parameters which included child related factors, dental clinical settings, dentist and dental treatment. Parents were given the questionnaire and were required to complete the questions within the treatment time (Figure 1).
Figure 1. Questionnaire.
Inclusion/exclusion criteria
The inclusion criterias for the study are parents of children with normal development and children should have a minimum of one previous dental treatment visit. The exclusion criterias include parents of children who require special needs or have associated systemic conditions.
Statistical analysis
From collected information, data were tabulated, processed and a descriptive analysis was performed.
Results and Discussion
The results of the study shows that 72 parents participated in the study of which, 25 male and 47 female parents participated in the study. The age group of the children ranges from 3 to 15 years. The results were analysed according to the parents whose child has undergone a minimum of one dental visit.
As we can see in the results, there are various influencing factors which drive a child to the dental clinic. Toothache accounts for 54% of the reasons a child visits the dental clinic, parent’s advice being 28% and a small group of children visiting the dental clinic due to a dentist’s advice. This shows that children are more prone to dental caries at a very young age which brings them to a dental clinic. The effect of child’s behaviour was also considered according to the experiences taken from friends or family, which shows that 12 children were strongly affected by the previous dental experiences, 22 children occasionally had an effect and for about 38 children this did not affect or stop them from visiting a dental clinic. Past dental experiences are seen to have an impact on the behaviour of the child as the child becomes very anxious and reluctant for a dental treatment.
When questioned about the preference of dental appointments, 64% of the parents felt that mornings were the most comfortable as they wanted the treatment of their child to be completed at the earliest. 25% and 11% of the parents preferred afternoons and evenings as their dental appointments because they did not want the child to compromise on school timings. According to the results, only 53 out of 72 children had consumed breakfast before the dental treatment and were found to be very cooperative during the treatment. Out of which 41 children had a carbohydrate rich diet, 9 children were enriched with a protein rich diet and 3 children had a fat rich diet.
Pertaining to the results, 50% of the children enjoyed themselves in the playroom, 28% of the children interacted more in the treatment room and the remaining children preferred staying in the reception room. Dentistry decoration is very important and influential for children; and it should be designed in such a way to give children a sense of relaxation and comfort. 81% of the children are more comfortable with a female dentist because they indulge the children in stories and create a comfortable rapport for them whereas 11% children say male dentists and to the other 8% of the children, the gender of the dentist does not affect their behaviour in the dental clinic. It was found that 6 children were comfortable with the dentist wearing a dental coat as it is blue in colour in Saveetha Dental college and Hospitals. 16 children found that wearing only a mask was a better way of interaction, 24 children preferred mask and protective glasses and a majority, 36% children wanted the dentist to be in a full attire of mask, dental coat and protective glasses. This shows that the children also feel that a dental attire should be followed by their respective dentist. 51% of the children underwent restorative (filling) procedures, as we know that saving a tooth is more important than the removal of the tooth from the oral cavity. Whereas extraction and scaling (cleaning) were the other two procedures which the child undergoes in equal numbers. When the respective treatments were performed to a child, 39% had anxious behaviour, 25% were scared, 24% were more anxious and only a small amount of 12% were very confident when the treatment was on process. When analysed about the behaviour the child underwent during the sound and noise of the instruments, a majority of 45 children were immediately anxious, 18 children were impatient and only 9 children were very brave and confident during the process. This shows that the dental procedures and instruments have a major impact on the behaviour of the child in dental clinics (Figures 2-6).
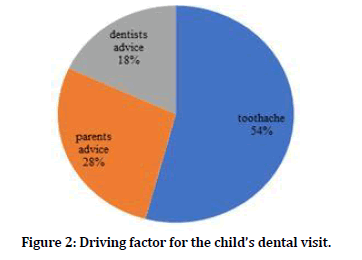
Figure 2. Driving factor for the child’s dental visit.
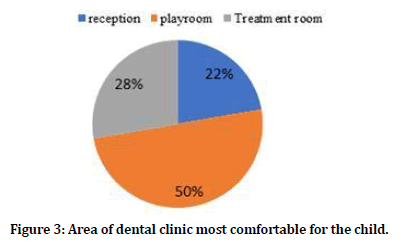
Figure 3. Area of dental clinic most comfortable for the child.
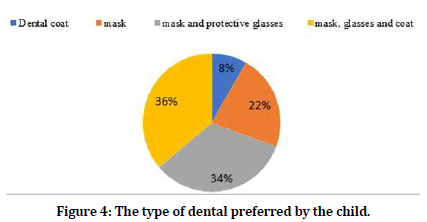
Figure 4. The type of dental preferred by the child.
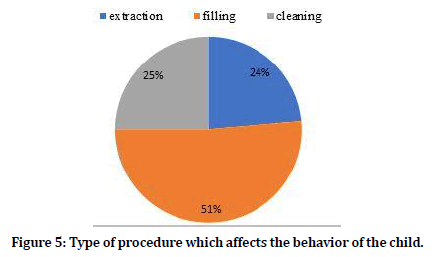
Figure 5. Type of procedure which affects the behavior of the child.
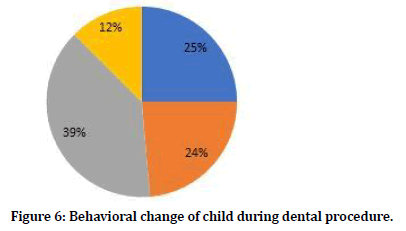
Figure 6. Behavioral change of child during dental procedure.
Parents and family members are considered to be among the first sources of primary information which the child receives about its oral habits, which undoubtedly has a long term influence in determining the future of a child's oral health status. This pilot study assessed parental perception on various influencing factors which determine a child's behaviour in the dental clinic.
There are various influencing factors which drive a child to the dental clinic, toothache being the most important and concerned complaint of a child. In this study more than half of the children come to dental clinics with the complaint of toothache. According to authors like Brill WA, the most common emotional upsets seen during dental treatment of a child are anxiety and fear, which might originate from a previous traumatic experience in the dental clinic or during hospitalisation for other reasons. He also said that depending on the age, behaviour at the first recall visit may be influenced by having undergone a dental procedure after the initial examination [35]. Pertaining to this, the effect of child’s behaviour in this study was also taken into account which shows that the majority of children were either strongly or occasionally affected by the previous dental experiences, and only a few children whose past dental experience did not have any effect on the dental treatment.Dental appointments play a major role in determining the child’s comfort in the dental clinic. Most of the parents felt morning appointments were the most comfortable for the child as they wanted the treatment of the child to be completed at the earliest. Whereas there were other parents who preferred afternoons and evenings as their dental appointments because they were concerned about the schooling of the child. Diet usually affects the cognitive ability and behaviour in children and adolescents. The diet of the child determines their behaviour in the dental clinic and is a major factor in the dental procedure. Overall, the literature given by Bellisle F [36] suggests that good regular dietary habits are the best way to ensure optimal mental and behavioural performance at all times. In contrast, children and adolescents with poor nutritional status are exposed to alterations of behavioural functions by dietary measures. According to the results of our study only 53 out of 72 children had consumed breakfast before the dental treatment and were found to be very cooperative during the treatment. The other children who did not consume breakfast before dental procedure, were found to be cranky and non-cooperative during the treatment.
American Academy of Pediatric Dentistry (AAPD) reveals that the orientation and environment of the dental environment plays an important role in determining the child‘s behaviour during the treatment [37]. Out of which, the play area in the dental clinic is designed with the use of child friendly colours like yellow and blue in the dental workplace could enhance a positive dental attitude in the child's mind. A study by Umamaheshwari N, Asokan S, Kumaran TS showed that children had positive reactions to bright colours like pink, blue, red and negative emotions for dark colours like brown, black, gray [38]. Another study by Cimbalo RS, Beck KL, Sendziak DS [39] concluded that children viewing happy scenes generally used yellow, blue, green and orange colour, whereas when viewing sad scenes, they tend to use red, black and brown. It was shown in our study that the children are very comfortable and happy in a colourful and pleasant environment.
Gender of the dentist has an impact on the child’s behaviour as well. A study conducted by Nagendran Jayavel Pandiyan, Amitha Hedge showed that 43% of parents agreed that a dentist's gender has an impact on a child's behaviour in dental clinics [40]. This has a major influence on our study as a greater number of children are more comfortable with a female dentist because they indulge the children in stories and create a comfortable rapport for them. Wright GZ, Kupietzky A quoted that when it comes to apparel for the dental team, there has been a developing concern that professional clothing and white lab coat worn by the dentist can increase anxiety levels in children. If a child has had previous poor experiences with a professional or doctor in a white coat, it is possible that these fears could be generalised to the dental environment [14]. But in our study it was found that only a few children were comfortable with the dentist wearing a dental coat which was blue in colour, some children found that wearing only a mask was a better way of interaction whereas the majority of children preferred the dentist to be in a full attire of mask of dental coat, mask and protective glasses. A mask during dental treatment represents a stressor for the young child, and so it is recommended to introduce the child to the dental environment without the use of a protective mask.
There are various dental procedures which the child undergoes in a dental clinic, the most important being restorative, extraction and cleaning. In a study conducted by Versloot J, Hoogstraten J, there was a positive correlation seen between levels of dental anxiety, psychological functioning and anxiety behaviour after the dental treatment [41]. In our study as well, half the number of the children underwent restorative treatment because parents wanted to save a tooth in the oral cavity rather than extract it. Extraction and scaling (cleaning) were the other two procedures which the child underwent in equal numbers. The dentist should also pay attention to the child’s attitude when dealing with them in the dental clinic in order to gain the child’s confidence and trust.
When the respective treatments were performed in a child, they were different behavioural patterns which were noticed in the child like anxious, scared and confident behaviour. Most of the children experienced scared and anxious behaviour where only a small group of children were very confident during the treatment. The behaviour of the dentist and dental staff members are the primary tools used to guide the behaviour of the pediatric patient. The dentist’s attitude, body language, and communication skills are crucial in creating a positive dental visit for the child and also to gain trust from the child and parent [42]. Furthermore, the sound and noise of the dental instruments during the procedure also created an increase in the anxiety levels of children which shows that a majority of children were immediately anxious, some of the children were impatient and only a few of them were very brave and confident during the process. Similar studies conducted by Appukuttan DP showed that 77% of parents agreed that types of procedures such as dental drilling / restoration and sight of instruments cause anxiety and fear in children [43].
Conclusion
In this study, we conclude that most of the parents believe that the dental appointments, the attire of the dentist as well as the dental procedure have a major influence in the manner in which the child behaves in the dental clinic.
Acknowledgement
The authors of this study would like to express their gratitude towards everyone who facilitated and enabled us to carry out this study successfully.
Conflict of Interest
None declared.
References
- Foy JM. For the american academy of pediatrics task force on mental health. Enhancing pediatric mental health care: Algorithms for primary care. Pediatrics 2010; 125:S109–S125.
- Ramos-Gomez FJ, Crystal YO, Ng MW, et al. Pediatric dental care: Prevention and management protocols based on caries risk assessment. J Calif Dent Assoc 2010; 38:746–761.
- Kuppuswamy VL, Murthy S, Sharma S, et al. Oral hygiene status, knowledge, perceptions and practices among school settings in rural South India. Oral Health Dent Manag 2014; 13:146–154.
- Weinstein P. Motivational interviewing concepts and the relationship to risk management and patient counseling. J Calif Dent Assoc 2011; 39:742–745.
- Saied-Moallemi Z, Virtanen JI, Tehranchi A, et al. Disparities in oral health of children in Tehran, Iran. Eur Archives Paediatr Dent 2006; 7:262–264.
- Eijkman MA, Houwink B, de With C. Some aspects of patient education by the dentist for mothers of young children. Ned Tijdschr Tandheelkd 1978; 85:304–315.
- Schroth RJ, Brothwell DJ, Moffatt MEK. Caregiver knowledge and attitudes of preschool oral health and early childhood caries (ECC). Int J Circumpolar Health 2007; 66:153–167.
- Skeie MS, Espelid I, Riordan PJ, et al. Caries increment in children aged 3-5 years in relation to parents’ dental attitudes: Oslo, Norway 2002 to 2004. Community Dent Oral Epidemiol 2008; 36:441–450.
- Gurunathan D, Shanmugaavel A. Dental neglect among children in Chennai. J Indian Society Pedodont Preventive Dent 2016; 34:364.
- Shalan T, Erickson PR, Hardie NA. Primary incisor decay before age 4 as a risk factor for future dental caries. Pardiatr Dent 1997; 19:37-41.
- Ramos-Gomez F, Jue B, Bonta CY. Implementing an infant oral care program. J Calif Dent Assoc 2002; 30:752–761.
- Ghanim AM, Hussein AS, Abu-Hassan MI, et al. Parent’s perception on the importance of their children's first dental visit (A cross-sectional pilot study in Malaysia). J Oral Dent Res 2013; 1:23–28.
- Chandrapooja J. Behavioural management techniques in pediatric clinic. Int J Pharm Biological Sci 2016; 6:10–15.
- Wright GZ, Kupietzky A. Behavior management in dentistry for children. John Wiley & Sons 2014.
- Chaudhary N, Ahlawat B, Kumar A. Factors affecting children’s behaviour in the dental office. J Pharm Biomed Sci 2015; 5.
- Ravikumar D, Ramakrishna M, Sharma N, et al. Evaluation of McNamara’s analysis in South Indian (Tamil Nadu) children between 8-12 years of age using lateral cephalograms. J Oral Biol Craniofac Res 2019; 9:193–197.
- Ravikumar D, Gurunathan D, Gayathri R, et al. DNA profiling of Streptococcus mutans in children with and without black tooth stains: A polymerase chain reaction analysis. Dent Res J 2018; 15:334.
- Ravikumar D, Jeevanandan G, Subramanian EMG. Evaluation of knowledge among general dentists in treatment of traumatic injuries in primary teeth: A cross-sectional questionnaire study. Eur J Dent 2017; 11:232–237.
- Ravindra V, Rekha V, Annamalai S, et al. A comparative evaluation between dermatoglyphic patterns and different terminal planes in primary dentition. J Clin Exp Dent 2018; 10:e1149–e1154.
- Ravindra V, Rekha CV, Annamalai S, et al. A comparative evaluation between cheiloscopic patterns and the permanent molar relationships to predict the future malocclusions. J Clin Exp Dent 2019; 11:e553–e557.
- Govindaraju L, Jeevanandan G, Subramanian EMG. Comparison of quality of obturation and instrumentation time using hand files and two rotary file systems in primary molars: A single-blinded randomized controlled trial. Eur J Dent 2017; 11:376–379.
- Govindaraju L, Jeevanandan G, Subramanian EMG. Knowledge and practice of rotary instrumentation in primary teeth among indian dentists: A questionnaire survey. J Int Oral Health 2017; 9:45.
- Nair M, Jeevanandan G, Vignesh R, et al. Comparative evaluation of post-operative pain after pulpectomy with k-files, kedo-s files and mtwo files in deciduous molars -A randomized clinical trial. BDS 2018; 21:411.
- Jeevanandan G, Ganesh S, Arthilakshmi. Kedo file system for root canal preparation in primary teeth. Indian J Dent Res 2019; 30:622–624.
- Panchal V, Jeevanandan G, Subramanian E. Comparison of instrumentation time and obturation quality between hand K-file, H-files, and rotary Kedo-S in root canal treatment of primary teeth: A randomized controlled trial. J Indian Soc Pedod Prev Dent 2019; 37:75–79.
- Subramanyam D, Gurunathan D, Gaayathri R, et al. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Eur J Dent 2018; 12:67–70.
- Vignesh R, Sharmin D, Rekha CV, et al. Management of complicated crown-root fracture by extra-oral fragment reattachment and intentional reimplantation with 2 years review. Contemp Clin Dent 2019; 10:397–401.
- Ramadurai N, Gurunathan D, Samuel AV, et al. Effectiveness of 2% Articaine as an anesthetic agent in children: Randomized controlled trial. Clin Oral Investig 2019; 23:3543–3550.
- Panchal V, Gurunathan D, Shanmugaavel AK. Smartphone application as an aid in determination of caries risk and prevention: A pilot study. Eur J Dent 2017; 11:469–474.
- Panchal V, Jeevanandan G, Subramanian EMG. Comparison of post-operative pain after root canal instrumentation with hand K-files, H-files and rotary Kedo-S files in primary teeth: a randomised clinical trial. Eur Arch Paediatr Dent 2019; 20:467–472.
- Jeevanandan G, Govindaraju L. Clinical comparison of Kedo-S paediatric rotary files vs manual instrumentation for root canal preparation in primary molars: A double blinded randomised clinical trial. Eur Arch Paediatr Dent 2018; 19:273–278.
- Samuel SR, Acharya S, Rao JC. School interventions-based prevention of early-childhood caries among 3-5-year-old children from very low socioeconomic status: two-year randomized trial. J Public Health Dent 2020; 80:51–60.
- Ramakrishnan M, Dhanalakshmi R, Subramanian EMG. Survival rate of different fixed posterior space maintainers used in Paediatric Dentistry - A systematic review. Saudi Dent J 2019; 31:165–172.
- Vishnu Prasad S, Kumar M, Ramakrishnan M, et al. Report on oral health status and treatment needs of 5-15 years old children with sensory deficits in Chennai, India. Spec Care Dentist 2018; 38:58–59.
- Brill W. The effect of restorative treatment on children’s behavior at the first recall visit in a private pediatric dental practice. J Clin Pediatr Dent 2002; 26:389–393.
- Bellisle F. Effects of diet on behaviour and cognition in children. Br J Nutrition 2004; 92:S227–S232.
- https://paperpile.com/app/p/f3d19279-557e-085e-900f-81e84e900fb0
- Umamaheshwari N, Asokan S, Kumaran T. Child friendly colors in a pediatric dental practice. J Indian Society Pedodont Preventive Dent 2013; 31:225.
- Cimbalo RS, Beck KL, Sendziak DS. Emotionally toned pictures and color selection for children and college students. J Genetic Psychol 1978; 133:303–304.
- Pandiyan NJ, Hedg A. Child behaviour in the dental clinic: Parent’s perception regarding various influencing factors. Pesquisa Brasileira Odontopediatr Clín Integrada 2017; 17:1–6.
- Versloot J, Veerkamp JSJ, Hoogstraten J. Dental anxiety and psychological functioning in children: Its relationship with behaviour during treatment. Eur Archives Paediatr Dent 2008; 9:36–40.
- AlSarheed M. Children’s perception of their dentists. Eur J Dent 2011; 5:186–190.
- Appukuttan D. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmetic Investigational Dent 2016; 35.
Author Info
Prerna Jain and Deepa Gurunathan*
Department of Paediatric and Preventive Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Prerna Jain, Deepa Gurunathan, Parents View Regarding Various Influencing Factors on Child Behavior in the Dental Clinic, J Res Med Dent Sci, 2021, 9 (2): 194-200.
Received: 14-Nov-2020 Accepted: 05-Feb-2021
