Research - (2022) Volume 10, Issue 7
Patients Perspectives on Polypharmacy: A Survey-Based Cross-Sectional Study
Aisha A Kassem1,2, Yosra Z Alhindi1*, Alaa H Falemban1,4, Asim M Alshanberi3, Nahla A Ayoub1,4 and Safaa M Alsanosi1
*Correspondence: Yosra Z Alhindi, Department of Pharmacology and Toxicology, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia, Email:
Abstract
Introduction: Management of chronic illnesses commonly includes a long-term pharmacological approach. Saudi Arabia has a great percentage of patients associated with multiple chronic diseases who need close attention and specialized care for their medications. Although this is a well-recognized problem, few studies have investigated medical prescription in connection to polypharmacy in Saudi Arabia. This study aims to elucidate patients’ perspectives on polypharmacy in primary healthcare (PHC) centers in the Makkah Region, Saudi Arabia. Method: A questionnaire-based cross-sectional study was conducted among patients attending PHC centers in the Makkah Region, Saudi Arabia (1 June to 31 November 2021). Patients aged 18 years and above who were taking prescribed or non-prescribed medications were included. Descriptive statistics were used to describe the participants' characteristics, and categorical variables were reported as frequencies and percentages. A Chi-square test was used to test the relation between variables. Results: In total, 213 participants were included in the study. Females represented 60% of the participants. In terms of the history of chronic diseases, 40% had hypertension and 34% had diabetes mellitus. As to the number of prescribed medications, 48% of participants mentioned that they took fewer than five, 29% took five, and 23% took more than five. As regards over-the-counter medications (OTC), 49% of the participants used OTC (21% used analgesics and 6% used antiallergics). Concerning side effects related to prescribed medications, about half of the participants experienced headache (51%), followed by muscle pain (23%), constipation or diarrhea (17%), and less than 10% for each of the remaining side effects. There was a significant relationship between the number of prescribed medications per day and the times patients forget to take their medications per week (P=0.045) and between the number of prescribed medications per day and the side effects related to prescribed medications (P<0.001). Conclusion: Polypharmacy is a serious issue of public concern. Physicians should be careful with the prescriptions they give to every patient, considering the risk and potential drug interactions that might accompany them. More longitudinal and prospective studies need to be done to detect the prevalence of polypharmacy in healthcare institutions in Saudi Arabia.
Keywords
Polypharmacy, Medical prescribing, Patient attitudes, Saudi Arabia
Introduction
Prescribing medications is a vital tool used by physicians to relieve symptoms and manage diseases [1]. It requires a thorough knowledge of the commonly prescribed medications and the principles of clinical pharmacology and therapeutics [2]. Furthermore, it requires the clinical skill to make decisions about potential benefits and risks and consider the evidence and factors relevant to the patient being treated [3]. The management of chronic illnesses commonly involves a long-term pharmacological approach. Although these medications effectively control diseases, their full benefits are often not realized because approximately 50% of patients do not take their medications as prescribed [4].
Multimorbidity and the associated use of many medications (polypharmacy) are common in the elderly population. The World Health Organization (WHO) defines polypharmacy as “the administration of many drugs at the same time or the administration of an excessive number of drugs” [5]. However, there is no agreed definition of polypharmacy, since definitions that include the therapy duration range from the use of two or more medications for more than 240 days (‘long-term use’) to five to nine medications used for 90 days or more [6,7]. In addition to increasing age, many factors contribute to polypharmacy, such as a lack of primary care providers to coordinate, multiple providers or pharmacies, copious prescribing, and self- treatment (such as over-the-counter (OTC) and herbal medications) [8,9]. Recently, physicians and researchers have studied polypharmacy to decrease or prevent its negative outcomes, such as adverse drug events, drug- drug interactions, medication non-adherence, and increased healthcare costs (for both the patient and the healthcare system) [9,10].
Saudi Arabia has a great percentage of patients afflicted with multiple chronic diseases who need close attention and specialized care for their medications [11]. Although it is a well-recognized problem, few studies have investigated medication prescribing in connection to polypharmacy in Saudi Arabia. This study aims to elucidate patients’ perspectives of polypharmacy by analyzing the various patterns of medication prescribing in PHC centers in the Makkah Region, Saudi Arabia.
Materials and Methods
Ethical approval
The study was approved by the Biomedical Research Ethics Committee, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia. Approval number: HAPO-02-K-012-2021-04-671, under the Declaration of Helsinki.
Study design
A cross-sectional study was conducted among patients attending PHC centers in the Makkah Region, Saudi Arabia. Patients aged 18 years and above who were taking any prescribed or non-prescribed medications were included. They were randomly approached by sending them the electronic questionnaire over six months (1 June to 30 November 2021). The purpose of the research was explained to participants in the questionnaire. They were also informed that participation was voluntary.
Questionnaire tool
The questionnaire was adapted from a previous study by Schiøtz et al. [12]. It was designed in English and translated into Arabic by proficient speakers of both languages. Experts provided their feedback and opinions to improve the questionnaire, and their suggestions were incorporated into the final version, which contained 19 questions and was designed using online cloud-based questionnaire development software (Google Forms). The questionnaire was divided into three main parts: sociodemographic information, including gender, age, education level, and history of chronic diseases; medication prescription; patients’ perspectives on polypharmacy.
Data collection
Social media platforms were used to distribute the questionnaire. All responses to the questionnaire were downloaded from the Google Forms website and held on a secure server. We received a complete case analysis of the answers provided by respondents who completed all 19 questions from the three -part survey. Participants who provided incomplete responses to the questionnaire were excluded. The data were collected from the spreadsheets provided by Google Forms and transferred to Microsoft Excel.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 22.0 (SPSS Inc., Chicago, IL, USA). All categorical variables were presented as frequencies and percentages (%). A Pearson Chi-square test was used to test the differences between variables. Statistical significance was determined at a P-value of <0.05.
Results
In total, 220 questionnaires were collected, of which seven were excluded because they had incomplete answers. Consequently, 213 questionnaires were included in this study. The participants’ demographic characteristics are shown in Table 1. Females represented 60% of the participants included in the study. In terms of age group, participants belonging to the 30–49 years and more than 50 years had equal percentages (40%), followed by 8–29 years (19%). Most participants (82%) had undergraduate education, 17% had basic education (including elementary, intermediate, and high school), and only 2% had postgraduate education. Concerning the history of chronic diseases, 40% had hypertension, 34% had diabetes mellitus, 12% had asthma, 7% had depression, and the rest had the following diseases: osteoporosis, rheumatoid arthritis, chronic obstructive pulmonary diseases (COPD), and thyroid disorders. Regarding OTC medications, 49% of the participants used OTC, 21% used analgesics, and 3% used antiallergics.
| Demographics | Numbers (%) (N= 213) |
|---|---|
| Age | |
| 18-29 | 41 (19%) |
| 30-49 | 86 (40%) |
| 50 or more | 86 (40%) |
| Gender | |
| Female | 128 (60%) |
| Male | 85 (40%) |
| Educational level | |
| Basic | 37 (17%) |
| Undergraduate | 174 (82%) |
| Postgraduate | 2 (1%) |
| History of chronic diseases | |
| Hypertension | 86 (40%) |
| Diabetes mellitus | 73 (34%) |
| Asthma | 26 (12%) |
| Depression | 15 (7%) |
| Others | 67 (365) |
| Use of OTC medications =105(49%) | |
| Analgesics | 44 (21%) |
| Antiallergics | 6 (3%) |
| Antiacids | 1 (0%) |
Table 1: Demographic characteristics of participants.
As regards the number of prescribed medications, 48% of participants mentioned that they took less than five, while 29% took five, and 23% took more than five prescribed medications, as shown in Figure 1. In terms of how many times per week patients forgot to take their prescribed medications, the highest percentage (43%) mentioned that they rarely forgot, followed by one to two times (30%), never forget (18%), three to four times (8%), and more than four times (1%), as shown in Figure 2.
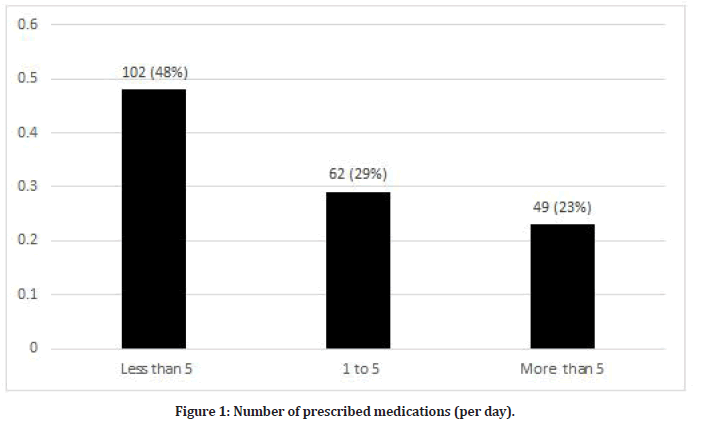
Figure 1: Number of prescribed medications (per day).
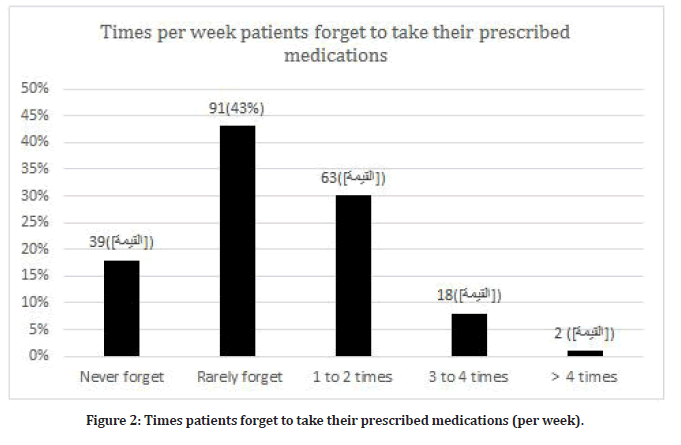
Figure 2: Times patients forget to take their prescribed medications (per week).
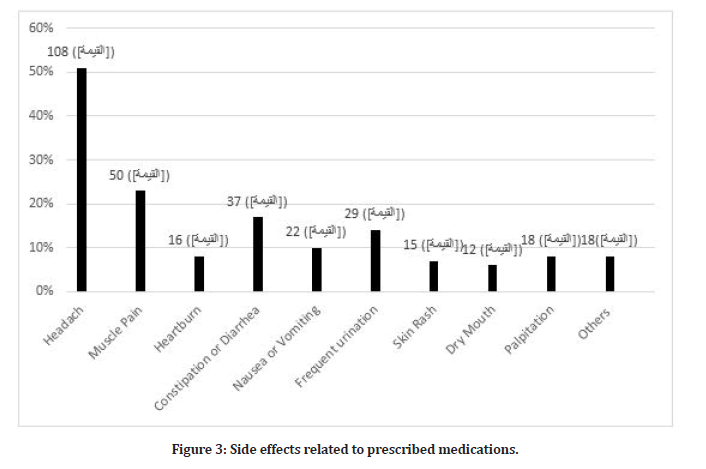
Figure 3: Side effects related to prescribed medications.
Concerning side effects related to the prescribed medications, about half of the participants experienced headache (51%), followed by muscle pain (23%), constipation or diarrhea (17%), frequent urination (14%), nausea or vomiting (10%), and less than 10% for other side effects, as shown in Figure 3.
As shown in Table 2, As regards patients’ perspectives on polypharmacy, 60% of the participants stated that their physician recommended diet or exercise with the prescribed medications, 75% stated that their pharmacist or physician explained to them how to use the medications, and 58% said that the pharmacist or physician did not explain to them the possibility of adverse drug reactions and drug-drug interactions. Almost half of the participants replied that they did not follow the recommendations of their treating physician, 82% said that they agreed if their pharmacist or physician decided to deprescribe a drug, 42% answered that if there was a prescribed medication, they did not believe was important, they sometimes ignored it. Further, 40% of participants said they used herbal medicine, and 43% believed that more drugs prescribed by the physician meant that the physician had more experience. Over half (56%) of the participants said they used medications prescribed at multiple hospitals or PHC centers to make sure that they were treated well. While 67% believed they had enough knowledge about the indications and proper use of their medications, 40% believed that taking many prescribed medications affected the quality of their lives.
| Statement | Yes | No | Sometimes | Total |
|---|---|---|---|---|
| My physician recommended diet or exercise with the prescribed medications. | 127 (60%) | 66 (31%) | 20 (9%) | 213 (100%) |
| My pharmacist or physician explained to me how to use the medications. | 159 (75%) | 28 (13%) | 26 (12%) | 213 (100%) |
| My pharmacist or physician explained to me the possibility of adverse drug reactions and drug-drug interactions. | 69 (32%) | 123 (58%) | 21 (10%) | 213 (100%) |
| I follow the recommendations of my treating physician. | 54 (25%) | 105 (49%) | 54 (25%) | 213 (100%) |
| I will agree if my pharmacist/physician decides to deprescribe any drug. | 174 (82%) | 11 (5%) | 28 (13%) | 213 (100%) |
| There is some prescribed medication that I believe is not important, and I ignore using it sometimes. | 62 (29%) | 90 (42%) | 61 (29%) | 213 (100%) |
| I use herbal medicine. | 85 (40%) | 77 (36%) | 51 (24%) | 213 (100%) |
| I believe that when the physician prescribes many drugs; he or she is highly experienced (more drugs = more experience). | 91 (43%) | 73 (34%) | 49 (23%) | 213 (100%) |
| I use prescribed medications from multiple hospitals or primary healthcare centers to make sure that I am treated well. | 54 (25%) | 120 (56%) | 39 (18%) | 213 (100%) |
| I have enough knowledge about the indications and proper use of my medications. | 161 (76%) | 24 (11%) | 28 (13%) | 213 (100%) |
| I believe that taking many prescribed medications affects the quality of my life. | 85 (40%) | 81 (38%) | 47 (22%) | 213 (100%) |
Table 2: Patients’ perspectives on polypharmacy.
As shown in Table 3, there was a significant relationship between the number of prescribed medications per day and the times patients forget to take their medications per week (P=0.045) and between the number of prescribed medications per day and the side effects related to prescribed medications (P<0.001).
| [1] Times patients forgot to take their medications per week | |||||||
|---|---|---|---|---|---|---|---|
| Times/week I forget to take my medications | Total | ||||||
| Never | Rarely | 1 to 2 times | 3 to 4 times | More than 4 | |||
| No. of prescribed medications per day | Less than 5 | 23 | 42 | 25 | 11 | 1 | 102 |
| 5 | 14 | 22 | 19 | 6 | 1 | 62 | |
| More than 5 | 2 | 27 | 19 | 1 | 0 | 49 | |
| Total | 39 | 91 | 63 | 18 | 2 | 213 | |
| Pearson Chi-square | P=0.045 | ||||||
| [2] Side effects related to prescribed medications | |||||||
| Side effects related to prescribed medications | |||||||
| Yes | No | Total | |||||
| No. of prescribed medications per day | Less than 5 | 46 | 56 | 102 | |||
| 5 | 24 | 38 | 62 | ||||
| More than 5 | 38 | 11 | 49 | ||||
| Total | 39 | 91 | 108 | ||||
| Pearson Chi-square | P<0.001 | ||||||
Table 3: Relationship between the number of prescribed medications per day and [1] times patients forgot to take their medications per week and [2] side effects related to prescribed medications. Statistical significance was determined at a P-value of <0.05.
Discussion
This study aimed to elucidate patients’ perspectives on polypharmacy and the various patterns in medication prescribing in PHC centers in the Makkah Region, Saudi Arabia. Polypharmacy can have serious consequences, particularly in old-age patients [13]. Multiple side effects such as falls, depression, frailty, and cognitive impairment have been associated with polypharmacy[14,15].
In the current study, nearly half of the participants (around 48%) were taking fewer than five medications per day, while around 23% were taking more than five medications per day. These results were higher than most of the studies assessing patterns of prescriptions in Saudi Arabia [16], India [17], Singapore [18], and the USA [19]. A possible reason for this difference is that the sample size was smaller, which is considered one of the limitations of this study.
The most common recorded comorbidity was hypertension, followed by diabetes and depression. Moreover, the most common OTC medications taken were analgesics. In addition, very few of the participants forgot to take their medications daily. This can be because around 40% of the participants were aged 30 to 50. However, there was a significant difference between the number of prescribed medications per day and the number of times patients forgot to take their medications per week. This means that polypharmacy can increase the risk of non-adherence to medications by forgetting to take them. This result parallels multiple studies that assessed polypharmacy and forgetting to follow the therapy and its impact on the patient’s quality of life [20-22].
Regarding the most common side effects related to the prescribed medications, headache appears at around 51% in our study, followed by muscle pain, constipation, diarrhea, frequent urination, and nausea or vomiting as the smallest percentage [23,24]. Headache is a common symptom and headache disorders are among the most common disorders affecting the nervous system, with a prevalence of 48.9% in the general population [5]. Headaches have a major impact on an individual’s quality of life, forcing massive costs to healthcare and indirectly to the economy overall. Only a small percentage of headache disorders need specialist involvement. The majority can be successfully treated in PHC centers with a correct clinical diagnosis that requires no special investigation [6].
In Saudi Arabia, polypharmacy is common among adult patients, especially those older than 60 [8]. The literature also shows that polypharmacy can affect the overall process of medication and the management of patients [25]. Clinical studies show that polypharmacy in hypertensive and diabetic patients is high, with a higher rate in older diabetics [26,27]. Moreover, another study performed in Riyadh states that there is an extremely high prevalence of polypharmacy in their patients and that polypharmacy seems to be a great issue in PHC centers, which will require more restricted pharmacovigilance and repeated review [28].
In the current study, regarding patients’ perspectives on medication prescription, more than half of the participants answered that their physician recommended diet or exercise with the prescribed medications and that their pharmacist or physician explained to them how to use the medications. On the other hand, more than half of the participants also said that the pharmacist or physician did not explain to them the possibility of drug- drug interactions. Comparable results were observed in a study that examined the patients' attitudes towards prescribing medications and therapeutics management. This suggested that if we want to enhance the quality of drug prescription, physicians’ education and training must be improved to offer better management and relations with patients.
Furthermore, around 40% of the participants in this study admitted to using herbal medicines. This use can have an impact on the patients’ lives (or life) as many of them take prescribed medications and do not tell their physicians about the herbs they are already taking, which can lead to interactions or toxicity [29]. Almost half of the participants (49%) responded that they did not follow the recommendations of their treating physician. Moreover, 42% said that if there was a prescribed medication that they believed was not important, they would sometimes not use it. Therefore, physicians should educate the patients about their medications to identify their own preferences and understand the serious consequences of medication non-adherence [30]. Interestingly, the participants said that they used prescribed medications from multiple hospitals or PHC centers to make sure they were treated well. In addition, some participants believed they had enough knowledge about the indications and proper use of the medications. An explanation for these statements is that more than half of the participants believed that a greater number of medications equaled more experience and a better outcome. However, only 40% of the participants admitted that taking many prescribed medications affected the quality of their lives.
Limitations
A few limitations should be considered when reading the results of this study. First, our study may not be representative because of the study design (online survey), Second, the study did not determine classes or subclasses of medications associated with polypharmacy. Even with these limitations, the present study will add to the knowledge in this area as we still have a limited number of studies addressing polypharmacy. As well, we included patients who were taking medications, both prescribed and non-prescribed, while previous studies focused on polypharmacy in certain drug classes or diseases.
Conclusion
In conclusion, polypharmacy is a serious issue of public concern, particularly in older populations with growing multiple morbidities. Therefore, the appropriate following of policies and guidelines to ensure that appropriate and beneficial medications are prescribed is essential. In clinical healthcare systems, professionals such as physicians should be careful with every prescription they give to every patient, given the risk and the potential drug interactions that might accompany it. Longitudinal and prospective studies are recommended to detect the prevalence of polypharmacy in healthcare institutions in Saudi Arabia.
References
- Velo GP, Minuz P. Medication errors: Prescribing faults and prescription errors. Br J Clin Pharmacol 2009; 67:624-628.
- Maxwell SR. Rational prescribing: The principles of drug selection. Clin Med 2016; 16:459-464.
- Vahdat S, Hamzehgardeshi L, Hessam S, et al. Patient involvement in health care decision making: A review. Iran Red Crescent Med J 2014; 16:e12454.
- Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc 2011; 86:304-314.
- Slabaugh SL, Maio V, Templin M, et al. Prevalence and risk of polypharmacy among the elderly in an outpatient setting: A retrospective cohort study in the Emilia-Romagna region, Italy. Drugs Aging 2010; 27:1019-1028.
- Mortazavi SS, Shati M, Keshtkar A, et al. Defining polypharmacy in the elderly: A systematic review protocol. BMJ Open 2016; 6:e010989.
- Nishtala PS, Salahudeen MS. Temporal trends in polypharmacy and hyperpolypharmacy in older New Zealanders over a 9-year period: 2005–2013. Gerontology 2015; 61:195-202.
- Martinez KA, Linfield DT, Gupta NM, et al. Patient and physician factors contributing to polypharmacy among older patients. Curr Med Res Opin 2022; 38:123-130.
- Maggiore RJ, Gross CP, Hurria A. Polypharmacy in older adults with cancer. Oncologist 2010; 15:507-522.
- Chumney EC, Robinson LC. The effects of pharmacist interventions on patients with polypharmacy. Pharm Pract 2006; 4:103-109.
- Alsuwaidan A, Almedlej N, Alsabti S, et al. A comprehensive overview of polypharmacy in elderly patients in Saudi Arabia. Geriatrics 2019; 4.
- Schiøtz ML, Frølich A, Jensen AK, et al. Polypharmacy and medication deprescribing: A survey among multimorbid older adults in Denmark. Pharmacol Res Perspect 2018; 6:e00431.
- Alharbi FF, Alharbi SF, Salih SB, et al. Correlates of psychotropic polypharmacy in outpatient psychiatric clinics of two military tertiary hospitals in Saudi Arabia. J Family Community Med 2019; 26:213-220.
- Pana A, Sourtzi P, Kalokairinou A, et al. Sarcopenia and polypharmacy among older adults: A scoping review of the literature. Arch Gerontol Geriatr 2022; 98:104520.
- Khezrian M, McNeil CJ, Murray AD, et al. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf 2020; 11:2042098620933741.
- Wastesson JW, Morin L, Tan EC, et al. An update on the clinical consequences of polypharmacy in older adults: A narrative review. Exp Opinion Drug Safety 2018; 17:1185-1196.
- Bawazir SA. Prescribing patterns of ambulatory care physicians in Saudi Arabia. Annals Saudi Med 1993; 13:172-177.
- Biswas NR, Biswas RS, Pal PS, et al. Patterns of prescriptions and drug use in two tertiary hospitals in Delhi. Indian J Physiol Pharmacol 2000; 44:109-112.
- Masood SM, Adhikari P. Prevalence of common geriatric giants among patients attending geriatric clinic of a tertiary care hospital. J Indian Academy Geriatr 2020; 16:68.
- Souliotis K, Giannouchos TV, Golna C, et al. Assessing forgetfulness and polypharmacy and their impact on health-related quality of life among patients with hypertension and dyslipidemia in Greece during the COVID-19 pandemic. Quality Life Res 2022; 31:193-204.
- Foley L, Larkin J, Lombard-Vance R, et al. Prevalence and predictors of medication non-adherence among people living with multimorbidity: A systematic review and meta-analysis. BMJ Open 2021; 11:e044987.
- Balkhi B, AlQahtani N, Alwhaibi M, et al. Prevalence and factors associated with polypharmacy use among adult patients in Saudi Arabia. J Patient Safety 2021; 17:e1119-24.
- Stovner L, Hagen K, Jensen R, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia 2007; 27:193-210.
- Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf 2014; 13:57-65.
- Alwhaibi M, Balkhi B, Alhawassi TM, et al. Polypharmacy among patients with diabetes: A cross-sectional retrospective study in a tertiary hospital in Saudi Arabia. BMJ Open 2018; 8:e020852.
- Asiri YA, Al-Arifi MN. Polypharmacy and patterns in drug prescribing at a primary healthcare centre in the Riyadh region of Saudi Arabia. Int J Pharma Practice 2011; 19:123-128.
- Aljawadi MH, Khoja AT, Alaboud NM, et al. Prevalence of polypharmacy and factors associated with it among Saudi Older adults - results from the Saudi national survey for elderly health (SNSEH). Saudi Pharm J 2022; 30:230-236.
- Figueiras A, Caamaño F, Gestal-Otero JJ. Influence of physician's education, drug information and medical-care settings on the quality of drugs prescribed. Eur J Clin Pharmacol 2000; 56:747-753.
- Rombolà L, Scuteri D, Marilisa S, et al. Pharmacokinetic interactions between herbal medicines and drugs: Their mechanisms and clinical relevance. Life 2020; 10.
- Kleinsinger F. The unmet challenge of medication nonadherence. Perm J 2018; 22:18-33.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Aisha A Kassem1,2, Yosra Z Alhindi1*, Alaa H Falemban1,4, Asim M Alshanberi3, Nahla A Ayoub1,4 and Safaa M Alsanosi1
1Department of Pharmacology and Toxicology, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia2Department of Pharmacy, King Abdullah Medical complex, Jeddah, Saudi Arabia
3Department of Community Medicine, Faculty of Medicine, Umm Al Qura University, Makkah, Saudi Arabia
4Saudi Toxicology Society, Umm Al-Qura University, Makkah, Saudi Arabia
Received: 02-Jul-2022, Manuscript No. JRMDS-22-68309; , Pre QC No. JRMDS-22-68309 (PQ); Editor assigned: 04-Jul-2022, Pre QC No. JRMDS-22-68309 (PQ); Reviewed: 19-Jul-2022, QC No. JRMDS-22-68309; Revised: 22-Jul-2022, Manuscript No. JRMDS-22-68309 (R); Published: 29-Jul-2022
