Research - (2022) Volume 10, Issue 4
Pediatric Scrotal Ultrasound for Detection of Infertility Etiology
*Correspondence: Yousif Abdallah, Department of Radiological Science and Medical Imaging, College of Applied Medical Sciences, Majmaah University, 11952, Majmaah, Saudi Arabia, Email:
Abstract
Purpose: The scrotum is an important organ in the reproductive system of male, as it comprises the testicle, which it in charge of manufacture sperm for preservation posterity of human being. Infertility has an apparent effect in most marital disputes. The main objective of this study is to detect scrotal diseases in children that may lead to infertility using ultrasonography. Methods: The cross-sectional study was performed on one hundred and ten pediatric patients who were submitted to the ultrasound department for scrotal examination. Different ultrasound modes were used in this survey to evaluate the participant's scrotum along with taking medical history and final physical examination. Both outcomes were compared to assess the efficiency of ultrasound Results: Out of 110 patients, the majority of abnormal ultrasound findings were an infection, varicocele, and hydrocele (30 cases, 18 cases, and 12 cases) have respectively. 98.04% and 75% were values of ultrasound sensitivity and specificity, respectively in diagnosing scrotal pathologies. Conclusion: At present, ultrasound offers high-quality services to assessment the scrotum of children according to several aspects include safety, perfect, dependable, and economical investigative techniques. These characteristics have enabled ultrasound to be an effective method in evaluating most diseases in the human body, especially diseases of the scrotum.Keywords
Pediatrics, Scrotal diseases, Ultrasonography, Infertility
Introduction
A human male has an external pouch that includes the important reproductive organs of men is known as scrotum [1]. It is considered the safe place for the testicles and is entrusted with providing the appropriate conditions for them [2].The variety of the scrotum formation before birth made it a fertile environment for the development of various diseases [3]. Epididymoorchitis is an inflammation condition of epididymis and testis, more common in boys over 6 years [4].The defect of venous system of testicular led to condition called a varicocele, it mostly exited left side [5]. A hydrocele was gathering of liquid substance in scrotum around a testis, it usual finished without any Medical intervention [6-8]. Testicular torsion is an urgent situation occurs when testis turns around within its pouch, and prevents its particular blood supply [9]. The presence of the testicle in an uncommon location after birth, is an infrequent birth defect called a testicular ectopy [10]. When abdominal parts exist in the groin, then expansion inside the scrotum, this condition known as inguinal hernia [11]. Among urogenital system neoplasms in children the frequency of testicular ones is uncommon [12]. Before it issued Miskin and Bain their statement about dealing with sonography as a new examination method for the scrotum; the physical examination is the common [13]. Assessment of the scrotum carried out by using grayscale ultrasound combined with a method of Doppler [14]. Today ultrasound with different modes plays a great role in the detection of any diseases related to scrotum [15]. By using ultrasound scan with multiple a manifestations of scrotal diseases it aimed to get appropriate finding [16]. According to the decrease in the blood vessels of the testis in children is not easy to report the flux [17]. Due to vague features of scrotal diseases, its defiance, for the health care professional to detect it [18]. Some scrotal abnormalities consider causes of infertility if left without treatment such as varicocele, infection and testicular torsion [19].
Materials and Methods
This a cross-sectional study carried out on 110 children age between 1 - 15 who were sent to the ultrasound departments at different Children hospitals in Khartoum state over a duration of 21 months from May 2020 to January 2021. The local ethics committee of hospital granted permission to conduct the survey. The inclusion criterion was children with an appearance of any scrotal diseases in the physical investigation. The exclusion criteria those who didn't agree to give consent. The participants underwent a general assessment, and their medical chart was reviewed. Ultrasonography performed using (ALOKA SSD-3500), apparatus with a highfrequency linear transducer (5-10 MHz). Examinations start with the child lay on his back; a series of images have taken in various views that cover scrotum, inguinal, and abdominal area if it’s necessary [20]. The accuracy of the ultrasound was defined by matching of the final examinations results (Tables 1 and Table 2).
| Ultrasound | Clinical assessment | Total | |
|---|---|---|---|
| Findings | Disease | Non-Diseased | |
| Positive | A(true +ve) | B (False +ve) | A+B |
| Negative | C (false –ve) | D (true –ve) | C+D |
| Total | A+C | B+D | A+B+C+D |
Table 1:Data analysis was done by the following table.
| Sensitivity | A/A +C X 100 |
| Specificity | D/B + D X 100 |
Table 2: Sensitivity and specificity calculation methods.
Results
The population of the study consists of one hundred and ten subjects, the age extended from one year to fifteen years with an average age of 10.38 ± 3.20 years. The majority of cases found in the age group of 11-15 years (74 cases –67.3%), the least of cases were in the age group 0–5 years (11 cases–10%) Table 3.
| Age group (years) | Frequency | (%) |
|---|---|---|
| 0-5 | 11 | 10 |
| 10-Jun | 25 | 22.7 |
| 15-Nov | 74 | 67.3 |
Table 3: Age distribution of the study participants.
The common finding of the study is an infection (26.36%) followed by varicocele(16.36%) then hydrocele (11.82%). The percentage of testicular torsion, tumors, Other conditions in this study were (7.27, 9.09 and, 9.09 respectively). An Inguinal hernia and ectopic testicle represent the minimum occurrence (5.45%, 4.55% respectively). There were 11 children (10%) show a normal scrotum sonographic appearance (Table 4). Figures 1-3 showed the ultrasound findings.
| Ultrasonography findings | Frequency | (%) |
|---|---|---|
| Normal | 11 | 10 |
| Infection | 30 | 26.36 |
| Varicocele | 18 | 16.36 |
| Hydrocele | 12 | 11.82 |
| Testicular torsion | 8 | 7.27 |
| Ectopic testicle | 5 | 4.55 |
| Inguinal hernia | 6 | 5.45 |
| Tumors | 10 | 9.09 |
| Other conditions | 10 | 9.09 |
Table 4: Findings of ultrasound in the study participants.
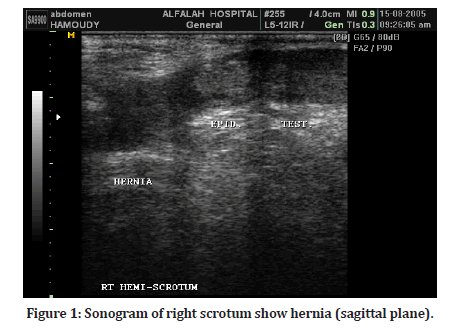
Figure 1: Sonogram of right scrotum show hernia (sagittal plane).
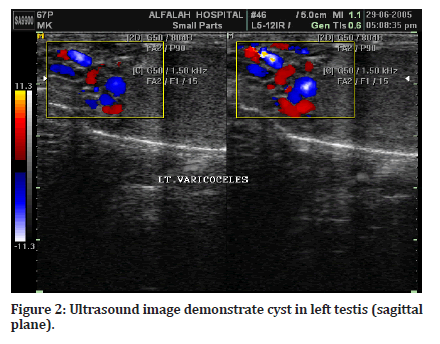
Figure 2:Ultrasound image demonstrate cyst in left testis (sagittal plane).
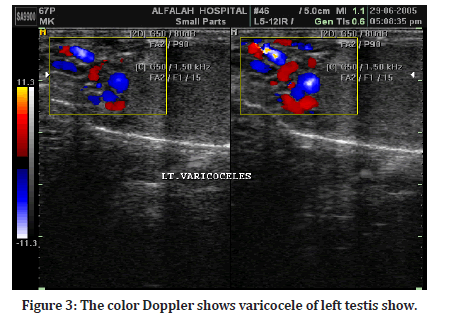
Figure 3:The color Doppler shows varicocele of left testis show.
Ultrasound was a perfect method for detecting scrotal abnormalities it illustrated extremely sensitive and specific(98.04% and 75% respectively). Another hand, it had a peaked positive and negative predictive rate (98.04% and 75% respectively) in Table 5.
| Ultrasound Finding | Final Finding | |
|---|---|---|
| Disease present | Disease absent | |
| Disease present | 100 | 2 |
| Disease absent | 2 | 6 |
| Total | 102 | 8 |
| Sensitivity=98.04%, Specificity=75% | ||
Table 5: Findings of ultrasound and the final diagnosis.
Discussion
According to their less risk, precision and uncomplicated ultrasound is the method of choice in assessment scrotal. In the present study, infection of the scrotum represents the highest percentage of 30 child patients (26.36%) out of 110 participants. This finding was supported by Rizvi et al. [18], which reported that most cases recorded by sonography were infection of the scrotum. And with Anderson et al. [21] who stated that the occurrence of epididymitis in children was 65% in study carried out in 2001. In contrast research done by Ibrahim [22] reported that before puberty, infection of scrotum was an infrequent. This current study revealed that the occurrence of varicocele and hydrocele among children was common; this result was matched to the finding of Tijani, et al. [23] and Tekgul et al. [24] in a study of Nigerian patients. And also, with the finding of previous studies, et al. [25] who stated that varicocele was widespread in age near puberty. This result was noncompliant with Simonsen et al. [26] and Pogorelić, et al. [27] who said that it related to age and most common in adulthood. In the current research, the percent of testicular torsion (TT) was slight low (7.27%). This outcome was in accord with Ashley et al. [28] who stated that TT was rare before puberty. Ectopic testicle demonstrated less frequency in this study 5 child out of 110 participants. This finding was matched with review performed by Hutson et al. [29] and Rahul et al. [30] who found that the occurrence of ectopic testicle about 1-4.5%. In this study the percentage of inguinal hernia was 5.45%. This finding was in agreement with Chow et al. [31] who found that this condition was more present in elderly people. The outcome of tumors in this study was 9.09%. This was compliant with Chung et al. [12] who stated that in Korea the prevalence of testicular tumors was uncommon in children under 4 years age. The increasing rate of scrotal diseases, One of the causes of male infertility [24]. Sensibility and precision of ultrasonography modality, Make it at the forefront of patterns of diagnosis of scrotum diseases.
Conclusion
Ultrasound becomes a suitable modality for evaluation of the scrotum due to its perfect, secure, low-cost, and reliable.
Acknowledgements
Special thanks to colleagues in areas of study.
Funding Acknowledgement
The author received no specific grants from any funding agency in the public, commercial, or non-profit-sectors.
Conflict Of Interest Statement
There are no financial or other relations that could lead to a conflict of interest.
References
- Patil V and Shetty S. Role of ultrasound and colour Doppler in scrotal pain. Int J Sci Res 2014; 3:178-183.
- Garcia RA, Sajjad H. Anatomy, abdomen and pelvis, scrotum. Stat Pearls 2019.
- Rosevear HM, Mishail A, Sheynkin Y, et al. Unusual scrotal pathology: An overview. Nat Rev Urol 2009; 6:491-500.
- Banyra O, Shulyak A. Acute epididymo-orchitis: Staging and treatment. Cent European J Urol 2012; 65:139-143.
- de los Reyes T, Locke J, Afshar K. Varicoceles in the pediatric population: Diagnosis, treatment, and outcomes. CUAJ 2017; 11:34-39.
- Palmer LS. Hernias and hydroceles. Pediatr Rev 2013; 34:457-464.
- Clarke S. Pediatric inguinal hernia and hydrocele: An evidence-based review in the era of minimal access surgery. J Laparoendosc Adv Surg Tech A 2010; 20:305-9PDF.
- https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Paediatric-Urology-2022.pdf
- Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and managements. Am Fam Physician 2013; 88:835-840.
- Gadelkareem RA, Shahat AA, Reda A, et al. Ectopic testis: An experience of a tertiary-level urology center at Upper Egypt. Annals Pediatr Surg 2020; 16:1-9.
- Subramanyam BR, Balthazar EJ, Raghavendra BN, et al. Sonographic diagnosis of scrotal hernia. Am J Roentgenol 1982; 139:535-538.
- Chung JM, Lee SD. Overview of pediatric testicular tumors in Korea. Korean J Urol 2014; 55:789-796.
- Prajapati N, Madhok R, Tapasvi C, et al. High frequency & color doppler ultrasound evaluation of scrotal and testicular pathologies. Int J Res Health Sci 2014; 2:153-61.
- Rathi R, Gothechal L, Gujjar R. Role of high-resolution ultrasonography and color doppler in scrotal pathology. Indian J Basic Appl Med Res 2016; 5:461-465.
- Rao M, Arjun K. Sonography of scrotal trauma. Indian J Radiol Imaging 2012; 22:293-97.
- Cokkinos D, Antypa E, Kalogeropoulos I, et al. Contrast-enhanced ultrasound performed under urgent condition.Indications, review of the technique, clinical examples and limitations. Insights Imaging 2012; 4:185-198.
- Dudea S, Ciurea A, Chiorean A, et al. Doppler applications in testicular and scrotal disease. Med Ultrason 2010; 12:43-51.
- Rizvi S, Ahmad I, Siddiqui M, et al. Role of color doppler ultrasonography in evaluation of scrotal swellings: Pattern of disease in 120 patients with review of literature. Urol J 2011; 8:60-65.
- Porth CM, Matfin G. Pathophysiology: Concepts of altered health states. 8th Ed. Philadelphia, PA: Lippincott Williams and Wilkins 2008.
- Klin B, Zlotkevich L, Horne T, et al. Epididymitis in childhood: A clinical retrospective study over 5 years. Israel Med Assc J 2001; 3:833-855.
- Anderson PA, Giacomantonio JM. The acutely painful scrotum in children: Review of 113 consecutive cases. Canadian Med Assoc J 1985; 132:1153-1155.
- Ibrahim MZ, Tabari AM, Igashi JB, et al. Scrotal doppler ultrasound evaluation in Zaria, Nigeria. Niger J Basic and Clin Sci 2016; 13:89-93.
- Tijani KH, Oyende BO, Awosanya GO, et al. Scrotal abnormalities and infertility in West African men: A comparison of fertile and sub-fertile men using scrotal ultrasonography. Afr J Urol 2014; 20:180-183.
- Simonsen PE, Meyrowitsch DW, Makunde WH, et al. The pattern of microfilaraemia and clinical manisfestations in three endemic communities of northeastern Tanzania. Acta Trop 1995; 60:179–187.
- Pogorelic Z, Neumann C, Jukic M. An unusual presentation of testicular torsion in children: A single-centre retrospective study. Can J Urol 2019; 26:10026-32.
- Ashley RA, Barthold JS, Kolon TF. Cryptorchidism: Pathogenesis, diagnosis, treatment and prognosis. Urol Clin North Am 2010; 37:183-193.
- Hutson JM, Balic A, Nation T, et al. Cryptorchidism. Semin Pediatr Surg 2010; 19:215-224.
- Rahul BG, Ravindranath GG. Incidence of inguinal hernia and its type in a study in a semiurban area in Andhra Pradesh, India. Int Surg J 2016; 3:1946-1949.
- Chow A, Purkayastha S, Athanasiou T, et al. Inguinal hernia. BMJ Clin Evid 2009; 4:1-20.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
1Department of Radiological Science, College of Applied Medical Sciences, Taif University, Taif, Saudi ArabiaDepartment of Radiological Science and Medical Imaging, College of Applied Medical Sciences, Majmaah University, 11952, Majmaah, Saudi Arabia
Citation: Bahaaedin A Elkhader, Yousif Abdallah, Pediatric Scrotal Ultrasound for Detection of Infertility Etiology, J Res Med Dent Sci, 2022, 10 (4):132-136.
Received: 01-Apr-2022, Manuscript No. JRMDS-22-59831; , Pre QC No. JRMDS-22-59831 (PQ); Editor assigned: 04-Apr-2022, Pre QC No. JRMDS-22-59831 (PQ); Reviewed: 18-Apr-2022, QC No. JRMDS-22-59831; Revised: 22-Apr-2022, Manuscript No. JRMDS-22-59831 (R); Published: 29-Apr-2022
