Research - (2021) Volume 9, Issue 7
Peri-Implant Soft and Hard Tissues Evaluation around Immediately Placed New Implant Design: Randomised Clinical Study
Amr Zahran1, Ahmed Mortada2, Maha Bahammam3 and Walid Elamrousy4*
*Correspondence: Faculty of Dentistry. Walid Elamrousy, Department of Periodontology and Oral Medicine, Kafrelsheikh University, Egypt, Email:
Abstract
Purpose: The present prospective randomized study aimed to assess and compare the influence of immediately placed, immediately restored, newly designed platform switched (PFS) Maxi-Z plus dental implant on marginal bone level (MBL) and the peri-implant soft tissues versus platform matched (PFM) Maxi-Z dental implant. Materials and methods: A total of 114 endosseous implants in 50 patients with different implant designs (PFS (n=25 patients, 58 implants), and PFM (n=25 patients, 56 implants)) were reviewed for implant mobility, MBL, and pink esthetic score (PES) for 1 year of the insertion. Results: Upon comparing changes of the clinical and radiographic parameters between the two groups, the changes of Periotest M values, MBL changes, and PES changes from baseline to 6 months were found to be significantly improved in the study group when compared to control group. Conclusion: Within the present study limitations, results concluded that PFS implants demonstrated better conditions regarding peri-implant soft tissue and cause minimal MBL loss.
Keywords
Dental implants, Periodontal disease.
Introduction
Hard- or soft-tissue defects around dental implant sites are multifactorial, including normal natural physiological resorption following exodontia, infection, trauma, periodontitis, abnormal growth and development, anatomical preconditions, mechanical force overload, thin gingival biotype, lack of or narrow keratinized mucosa, malpositioning of implants, systemic diseases and implant design. The severity of the resulting defect may increase with the existence of multiple factors together [1].
Nowadays, delayed placement of dental implants without socket preservation approach causes not only unaesthetic outcomes but also unpredictable bone loss and prolonged healing time. On the other hand, immediate implant placement represents the treatment choice for socket’s walls preservation after the extraction and improved aesthetic outcomes [2,3].
Traditional implant loading approach implies 3-6 months load-free healing period. Recently published studies have revealed non-significant difference in terms of success of dental implants and marginal bone alterations between immediate and delayed loading [4,5].
Interestingly, different implant design characteristics had been confirmed to affect the overall implant success [6]. In 2006 Lazzara and Porter first introduced the platformswitching (PFS) concept by connecting a narrow abutment to a wider implant fixture leading to inward shifting the contour of the abutment [7]. That PFS approach was found to preserve MBL and peri-implant soft tissue [8].
Maxi-Z plus dental implant fixture with tapered body (OsteoCare™ Implant System, London, United Kingdom) has been modified by 45-degree chamfer to the outer diameter of implant external form, also the thread external thread continued to 0.3 mm from the implant top. This unique implant design is tailored for immediately placedimmediately loaded dental implants.
However, little evidence on the role of implants’ neck designs on peri-implant hard and soft tissue preservation. In the present prospective study, we aimed to assess peri-implant hard and soft tissue outcomes around specially designed PFS dental implant fixture inserted immediately in freshly extracted sockets followed by immediate temporization.
Materials and Methods
In this prospective comparative study, 50 healthy individuals (26 males and 24 females), with age range 18-45 years who require replacement of two or more unrestorable permanent maxillary anterior or premolar teeth due to root fracture, endodontic failure or unrestorable crown fracture, were enrolled in the present study from April 2020 to May 2021 (Figure 1). Institutional research ethical approval by the institutional review board of the faculty of medicine in Assiut University was obtained before start of the study (number 17300586) and was registered in clinical trials registration with number NCT04905758. All participants signed written informed consent.
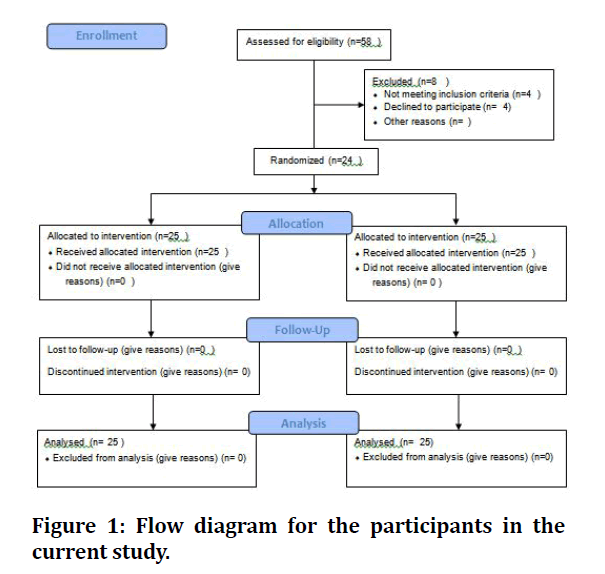
Figure 1: Flow diagram for the participants in the current study.
Inclusion Criteria included good oral hygiene with good periodontal condition and no periapical lesions. Exclusion criteria included local or systemic disease interfering with implantation, smoking, betel nut chewing, tobacco chewing, alcoholics, pregnants, parafunctional habits, persistent periodontal disease, or inadequate bone.
Presurgical scaling and root planning, oral hygiene instructions and radiographic examination were done (Figures 2 and 3). Patients were randomly categorized using computer software into 2 groups: control group (25 patients) used platform matching (PFM) dental implant (Maxi-Z dental implant fixture, OsteoCare™ Implant System, London, United Kingdom) and study group (25 patients) used platform switching (PFS) dental implant (Maxi-Z plus dental implant fixture, OsteoCare™ Implant System, London, United Kingdom).
Figure 2: Presurgical scaling, root planning and radiographic examination.
Figure 3: Oral hygiene.
Surgical procedures
Full thickness mucoperiosteal flap was reflected, and then traumatic tooth extractions were performed under local anaesthetic. Buccal bone plate integrity was confirmed using osteotomy probe followed by osteotomy preparation with Ultra 3.25mm drill extending 3-5mm apical to the fresh socket apex. Dental implants were inserted 3-5 mm beyond the socket base and 1-2 mm below the level of crestal bone with at least 30N/cm primary stability (Figure 4). Then abutment was prepared and screwed to the fixture and the flap was sutured (Figure 5). Temporary crown was adjusted to be completely out of functional occlusion and finally cemented within 48 hours of the surgery (Figure 6). Subjects stick to postoperative instructions including chlorhexidine 0.12% rinsing twice daily for 10 days, antibiotic Augmentin® 1g tablet (Medical Union Pharmaceutical Co. Egypt) twice daily for 5 days, and analgesic Brufen® 200 mg (Khaira Pharmaceutical Co., Egypt) t.d.s for 5 days. Sutures were removed after 2 weeks. 6 months later, the provisional acrylic resin restorations were replaced by final zirconium restorations.
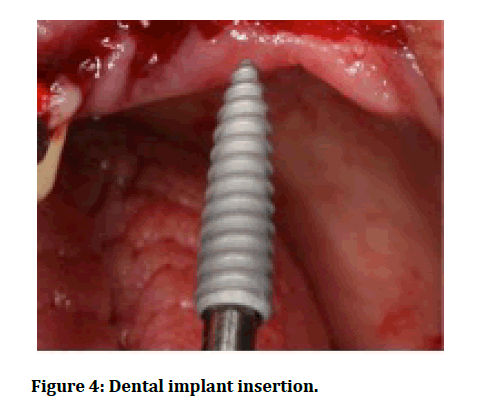
Figure 4: Dental implant insertion.
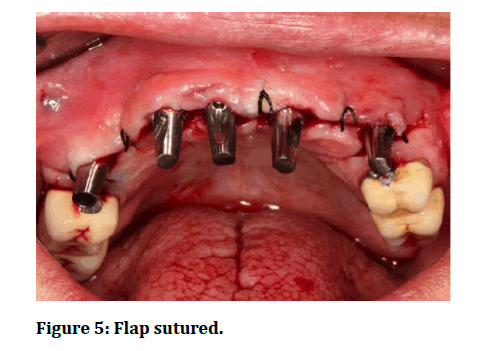
Figure 5: Flap sutured.
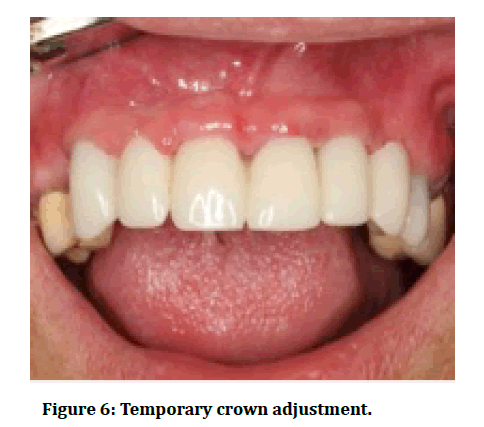
Figure 6: Temporary crown adjustment.
Follow-up evaluation and success criteria
All patients were clinically and radiographically examined immediately after surgery, 6 months and again at 12 months post-operatively. The participants were reviewed for: presence of peri-implant infection, postoperative persistent local pain, neuropathies or paraesthesia. In addition, the patients were evaluated for presence of clinically detectable mobility. Periotest M (Periotest® M, Medizintechnik Gulden, Bensheim, Germany) was used to test implant stability and osseointegration at 6 and 12months. PTMV range from (-8 to 0). Loose implants show high Periotest M values (PTMV), while Osseo integrated implants have low PTMV.
Radiographic evaluations
Standardized serial periapical radiographs using parallel technique, panoramic radiographs and CBCT were undertaken preoperative, immediately after operation (within the first 24 hours), 6 months and 12 months post-operatively to assess MBL around the placed implants.
Esthetics outcomes
Clinical digital intraoral images were captured by digital single-lens reflex camera systems (Nikon USA) throughout the study recall visits. For image standardization, the camera photographic settings of first visit for every subject were recorded and were identically repeated at subsequent visits. Two blinded calibrated clinicians evaluated and scored PES using the images throughout 1-year follow-up recall visits [9].
Sample size calculation
Using PASS software, sample size was calculated. Noninferiority margin record has been adjusted at 1, significance level at 0.05 and power (β) at 95%was established a priori. According to the preliminary data, sample size had to be 24 patients in each group. Considering around 20% dropout, 58 participants were recruited.
Statistical analysis
All variables mean values and standard deviation values were calculated for both groups. Statistical analysis was performed with IBM® SPSS® Statistics Version 26 for Windows.
Chi-square test was utilized for comparing categorical variables, whereas Mann Whitney test compared continuous variables. Paired sample t-tests were used to compare means with repeated measures within groups with continuous variables. The statistical significance level was adjusted at P ≤ 0.001.
Results
The population characteristics of this study are summarized in Table 1 and the candidate’s flow diagram is presented in Figure 1. A total of 50 patients (25 each group with total 114 dental implants) completed the 12 months follow-up. The clinical and radiographic parameters at baseline immediately after implant placement, 6 months and 12 months are summarized in Tables 2 and 3.
Table 1: Demographic data.
| Variable | Control group | Study group | |
|---|---|---|---|
| Age (years) | |||
| Mean ± SD | 42.28 ± 9.62 | 41.38 ± 8.73 | |
| Median (range) | 40 | 39 | |
| Gender (n[%]) | |||
| Male | 13 (52%) | 14 (56%) | |
| Female | 12 (48%) | 11 (44%) | |
SD: Standard deviation.
Table 2: Mean ± SD values of clinical and radiographic parameters of both groups at baseline and 6 months postoperatively.
| Control Group | Study Group | |||
|---|---|---|---|---|
| Parameter | Mean ± SD | P | Mean ± SD | P |
| periotest M value | ||||
| Baseline | -0.53 | <0.001* | -0.55 | <0.001* |
| 6 months | -2 | -3.38 | ||
| periotest M value | ||||
| 6 months | -2 | >0.001 | -3.38 | >0.001 |
| 12 months | -2 | (NS) | -3.38 | (NS) |
| MBL | ||||
| Baseline | 17.96 ± 1.69 | <0.001* | 18.63 ± 2.34 | >0.001 |
| 6 months | 16.76 ± 1.66 | 18.27 ± 2.34 | (NS) | |
| MBL | ||||
| 6 months | 16.76 ± 1.66 | >0.001 | 18.27 ± 2.34 | >0.001 |
| 12 months | 16.75 ± 1.66 | (NS) | 18.25 ± 2.34 | (NS) |
| PES | ||||
| Baseline | 7.20 ± 0.77 | <0.001* | 6.93 ± 0.59 | <0.001* |
| 6 months | 8.67 ± 0.72 | 9.47 ± 0.83 | ||
| PES | ||||
| 6 months | 8.67 ± 0.72 | >0.001 | 9.47 ± 0.83 | >0.001 |
| 12 months | 9.07 ± 0.79 | (NS) | 9.93 ± 0.70 | (NS) |
MBL: Marginal Bone Level
PES: Pink Esthetic Score
*: Statistical significant difference
NS: Not statistically significantly different
SD: Standard deviation
Table 3: Mean changes in the clinical and radiographic parameters over 12-months period among both groups.
| Parameter | Control Group Mean ± SD | Study Group Mean ± SD | P |
|---|---|---|---|
| periotest M value gain 0-6 | 2.04 ± 0.74 | 3.18 ± 0.47 | <0.001* |
| periotest M value Reduction 6-12 | 0.00 ± 0.00 | 0.00 ± 0.00 | >0.001 (NS) |
| MBL Reduction 0-6 | 1.19 ± 0.30 | 0.36 ± 0.38 | <0.001* |
| MBL increase 6-12 | 0.18 ± 0.01 | 0.15 ± 0.01 | >0.001 (NS) |
| PES Reduction 0-6 | 1.47 ± 0.51 | 2.53 ± 0.91 | <0.001* |
| PES increase 6-12 | 0.40 ± 0.63 | 0.47 ± 0.51 | >0.001 (NS) |
MBL: Marginal Bone Level
PES: Pink Esthetic Score
*: Statistical significant difference
NS: Not statistically significantly different
SD: Standard deviation
Wound healing of both groups was uneventful in all patients, no signs of local persistent pain, tenderness, neuropathies, and paraesthesia or wound dehiscence were observed throughout the evaluation period. Twenty-three patients presented with mild pain and mild local swelling immediately after surgery, which gradually subsided within 4 days postoperatively. The implants survival rates were 100% with no mobility all over the recall visits.
Considerable significant statistical reduction of the Periotest M values from -0.68 ± 0.15, -0.69 ± 0.13 at base line to -2.73 ± 0.73, -3.87 ± 0.49 at 6 months was noticed in control and study groups respectively.
The mean MBL values immediately after implant placement were found to be 17.96 ± 1.69 mm for the control group and 18.63 ± 2.39 mm for the study group. 6 months postoperatively, statistical significant loss of MBL was noticed in the control group [16.76 ± 1.66mm] and non-significant loss was observed in the study group [18.27 ± 2.34mm]. Moreover, 12 months values of MBL were non-significantly reduced to 16.75 ± 1.66mm and 18.25 ± 2.34mm for the control and study groups respectively when compared to 6 months means.
Regarding the mean values of the PES, the recordings of the control and study groups respectively were significantly improved from 7.20 ± 0.77, 6.93 ± 0.59 at base line to 8.67 ± 0.72, 9.47 ± 0.83 after 6 months and were improved to 9.07 ± 0.79, 9.93 ± 0.70 at 12 months but without significant difference than 6 months records.
Discussion
The main present study purpose was to compare PFS versus PFM dental implants regarding implant mobility, MBL as well as soft tissue condition.
Regarding the timing of implant placement, all implants in both groups of the present study were placed immediately after tooth extraction. Soft and hard tissue preservation is the rationale for immediately placed implants in fresh extraction sockets [10]. As said, in the study of Menchini-Fabris and co-workers, immediate implant placement showed lower MBL loss compared with delayed implant placement after 3-years [11]. Moreover, other studies confirmed that immediate implant placement not only preserve the preexisting soft and hard tissues architecture, but also reduce the surgical procedures, decrease the overall treatment timing and increase the patient satisfaction [12-14].
In this study, the implants were placed 1 to 2 mm below bone crest for both PFS and PFM groups. Valles and colleagues systematic review showed that subcrestal placement of PFS implants demonstrated less MBL changes when compared to equicrestal implant placement [15]. Furthermore, Subcrestal implant placement in esthetics areas was found to decrease the risk of implant or abutment metal collar exposure and to obtain a restoration with an ideal emergence profile [15]. On the other hand, a review of Suaárez-Loópez Del Amo confirmed that placing implants supracrestally had demonstrated many beneficial effects as reducing marginal bone resorption and formation thicker periimplant soft tissue [16].
In this study, immediate provisional restorations have been applied to the two treatment groups. The beneficial role of immediate provisionalization have been reported by Saito et al by providing a platform for early healing of peri-implant soft tissue and preservation of MBL [17]. This is in accordance with other studies, which noted that immediate provisional restorations reduce periimplant bone loss and improve peri-implant soft tissue condition required for bone preservation and establishment of biologic width [16,18,19].
Results of this study, using PFS implants with immediate placement of implant and immediate provisional prosthesis was accompanied with a significantly higher stability of alveolar ridge dimension and peri-implant soft tissue scores than using PFM implants after 12 months follow up period.
The PFM implants group in this study showed significant higher MBL loss in the first year 6 months than PFS implants, the measured data of PFM group were even close to the data reported in literatures [20,21]. Traditionally, MBL loss 1 year after loading had found to be 1.0 – 1.2 mm and in the following years 0.2 mm loss due to physiological bone remodeling process. On contrary, recent literatures have demonstrated less MBL loss than previously reported values [22-28].
Regarding PFS implants in the present study, showed a significant much lesser resorption of MBL in the first 6 months, but from 6-12 months were comparable with loss values in the control group and previously mentioned literatures for the same time interval. Parallel to the recorded results here, a previous review of DI Girolamo et al. had pointed out that PFS implant group showed less resorption of MBL than PFM implant group by reducing the abutment diameter 0.45 mm than the implant diameter [29]. Similar with present study result, Enkling and colleagues reported that PFS implants showed a very limited MBL alteration [30]. Moreover, Wagemberg and Forum in a prospective study evaluated MBL around PFS implants for 11-14 years, the results showed minimal MBL loss confirming that PFS was effective approach for MBL preservation [31].
The minimal MBL resorption around implants with PFS is primarily related to reestablishment of the biologic width resulted from implant-abutment horizontal mismatch [32]. A human histologic study confirmed that PFS implants maintained the level of crestal bone around implants [33]. In addition, minimal MBL resorption associated with PFS implants could be attributed to force dissipation to internal implant abutment junction than to external junction, thus this improves occlusal loads distribution on the restoration surface along the implant axis [34,35]. Also, the implant-abutment microgap play an important role in peri-implant MBL remodeling, as PFM implants are associated with bacterial colonization in the implant sulcus, with subsequent penetration of bacteria and its products within this microgap That may cause initiation and progression of inflammatory process close to crestal bone, resulting in MBL loss. Whereas in PFS implants inward moving of the implant abutment junction that brings out bacteria more internally away from the crestal alveolar bone [36-38].
Changes in the peri-implant esthetics soft tissue condition were analysed in terms of PES values for PFS and PFM designs of implant in this study. PES outcomes for one-year demonstrated that both geometries of implant-abutment interface yielded dramatic improvement in the first 12 months following implant placement and immediate temporization, with the most statistically significant scores improvement observed during the first 6 months. At 6 months recall visit, the PES outcomes reported in this study demonstrated that PFS implant-abutment interface design yielded superior mucosal esthetics when compared to PFM interface, whereas at 12 months both groups demonstrated similar stability with asymptotic insignificant changes of mean PES scores when compared to 6 months values.
The present study PES mucosal outcomes correlate with other researchers’ findings that showed a dynamic periimplant mucosal plasticity and maturation through the first 6 months following implant loading, followed by peri-implant mucosal maturation in the next 6 months which lead to soft tissue stability. [39-41]. The esthetic outcomes of the present study are in agreement with the results of Cheng et al study who confirmed that PFS implants showed significant improvement of periimplant mucosa esthetics due to reduction of periimplant tissue inflammatory status [42]. Also the study of Lowy et al and Lago et al. noted that PFS implants demonstrated significant reduction of facial recession, and significant improvement of papilla fill when compared to PFM implants [43,44].
The PES outcomes of the present study are not in consistent with the results of Luongo and coworkers who assessed the peri-implant soft tissue around PFS implants, they concluded that peri-implant PES showed undetectable differences when compared to PFM implants [45].
Related to these study findings, the PES improvement in PFS implants could be explained by the absolute biologic sealing capability of implant- abutment interfaces that decreases saliva and bacteria penetrating of this connection and per implant sulcus [46].
Conclusion
Within the current study limitations, PFS implants design seems to represent better conditions of peri-implant hard and soft tissues and cause less MBL loss. Further studies with more participants and longer evaluation period would be necessary to validate the present study.
Data Availability Statement
Data available on request from the authors.
Funding Statement
No funding.
Conflict of Interest
No conflicts.
Acknowledgement
None.
References
- Hämmerle CHF, Tarnow D. The etiology of hard and soft-tissue deficiencies at dental implants: A narrative review. J Periodontol 2018; 89:S291-S303.
- D'Avenia F, Del Fabbro M, Karanxha L, et al. Hard and soft tissue changes in the rehabilitation of the anterior maxilla with triangular shape neck implants: A retrospective clinical study with a one-year follow up. J Biol Regul Homeost Agents 2019; 33:13-21.
- Elamrousy WA, Nassar M, Ragheb AM, et al. Radiographic bone changes around immediately placed immediately restored dental implants in periodontally compromised sites. Dentistry 2013; 3:1-5.
- Wahengbam P, Fatima D, Sehrawat M, et al. A review on loading protocols in implants. IP Ann Prosthodont Restor Dent 2021; 7:37-40.
- Mijiritsky E, Ben Zaken H, Shacham M, et al. Variety of surgical guides and protocols for bone reduction prior to implant placement: A narrative review. Int J Environ Res Public Health 2021; 18:2341.
- Ríos-Santos JV, Menjívar-Galán AM, Herrero-Climent M, et al. Unravelling the effect of macro and microscopic design of dental implants on osseointegration: a randomised clinical study in minipigs. J Mater Sci Mater Med 2018; 29:99.
- Linkevicius T, Puisys A, Steigmann M, et al. Influence of vertical soft tissue thickness on crestal bone changes around implants with platform switching: A comparative clinical study. Clin Implant Dent Relat Res 2015; 17:1228-36.
- Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent 2006; 26:9-17.
- Belser UC, Grütter L, Vailati F, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol 2009; 80:140-51.
- Schropp L, Isidor F. Timing of implant placement relative to tooth extraction. J. Oral Rehabil 2008; 35:33–43.
- Menchini-Fabris GB, Toti P, Crespi G, et al. Effect of different timings of implant insertion on the bone remodeling volume around patients' maxillary single implants: A 2-3 years follow-up. Int J Environ Res Public Health 2020; 17:6790.
- Bruschi E, Manicone PF, De Angelis P, et al. Comparison of marginal bone loss around axial and tilted implants: A retrospective CBCT analysis of up to 24 months. Int J Periodontics Restor Dent 2019; 39:675–684.
- Quaranta A, Perrotti V, Putignano A, et al. Anatomical remodeling of buccal bone plate in 35 premaxillary post-extraction immediately restored single TPS implants: 10-year radiographic investigation. Implant Dent 2016; 25:186–192.
- Barone A, Rispoli L, Vozza I, wt al. Immediate restoration of single implants placed immediately after tooth extraction. J Periodontol 2006; 77:1914–1920.
- Valles C, Rodríguez-Ciurana X, Clementini M, et al. In- fluence of subcrestal implant placement compared with equicrestal position on the peri-implant hard and soft tissues around platform-switched implants: A systematic review and meta-analysis. Clin Oral Investig 2018; 22:555–570.
- Suárez-López Del Amo F, Lin GH, Monje A, et al. Influence of soft tissue thickness on peri-implant marginal bone loss: A systematic review and meta-analysis. J Periodontol 2016; 87:690–699.
- Saito H, Chu SJ, Reynolds MA, et al. Provisional restorations used in immediate implant placement provide a platform to promote peri-implant soft tissue healing: A pilot study. Int J Periodont Restorative Dent 2016; 36:47–52.
- Galindo-Moreno P, León-Cano A, Ortega-Oller I, et al. Prosthetic abut- ment height is a key factor in peri-implant marginal bone loss. J Dent Res 2014; 93:80–85.
- Vervaeke S, Dierens M, Besseler J, et al. The influence of initial soft tissue thickness on peri‐implant bone remodeling. Clin Implant Dent Related Res 2014; 16:238-47.
- Goiato MC, Pellizzer EP, da Silva EV, et al. Is the internal connection more efficient than external connection in mechanical, biological, and esthetical point of views? A systematic review. Oral Maxillofac Surg 2015; 19:229–242.
- Lombardi T, Berton F, Salgarello S, et al. Factors influencing early marginal bone loss around dental implants positioned subcrestally: A multicenter prospective clinical study. J Clin Med 2019; 8:1168–1181.
- Pan YH, Lin HK, Lin JC, et al. Evaluation of the peri-implant bone level around platform-switched dental implants: a retrospective 3-year radiographic study. Int J Environ Res Public Health 2019; 16:2570–2582.
- Rana V, Dhakne VM, Jadhawar S, et al. Bone level measurements around platform switched and platform matched implants: A comparative study. Niger J Surg 2019; 25:9–13.
- Schwarz F, Alcoforado G, Nelson K, et al. Impact of implant-abutment connection, positioning of the machined collar/microgap, and platform switching on crestal bone level changes. Camlog foundation consensus report. Clin Oral Implants Res 2014; 25:1301–1303.
- Wallace SS. Significance of the ‘biologic width’ with respect to root-form implants. Dent Implantol Update 1994; 5:25–29.
- Hermann JS, Buser D, Schenk RK, et al. Crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged and submerged implants in the canine mandible. J Periodontol 2000; 71:1412–1424.
- Gupta S, Sabharwal R, Nazeer J, et al. Platform switching technique and crestal bone loss around the dental implants: A systematic review. Ann Afr Med 2019; 18:1–6.
- Spinato S, Galindo-Moreno P, Bernardello F, et al. Minimum abutment height to eliminate bone loss: influence of implant neck design and platform switching. Int J Oral Maxillofac Implants 2018; 33:405–411.
- DI Girolamo M, Calcaterra R, DI Gianfilippo R, et al. Bone level changes around platform switching and platform matching implants: A systematic review with meta-analysis. Oral Implantol 2016; 9:1–10.
- Enkling N, Jöhren P, Klimberg T, et al. Open or submerged healing of implants with platform switching: A randomized, controlled clinical trial. J Clin Periodontol 2011; 38:374-84.
- Wagenberg B, Froum SJ. Prospective study of 94 platform-switched implants observed from 1992 to 2006. Int J Periodontics Restorative Dent 2010; 30:9-17.
- arronato D, Santoro G, Canullo L, et al. Establishment of the epithelial attachment and connective tissue adaptation to implants installed under the concept of “platform switching”: A histologic study in minipigs. Clin Oral Implants Res 2012; 23:90–94.
- Nevins M, Camelo M, Koo S, et al. Human histologic assessment of a platform-switched osseointegrated dental implant. Int J Periodontics Restorative Dent 2014; 34:s71–s73.
- Taheri M, Akbari S, Shamshiri AR, et al. Marginal bone loss around bone-level and tissue-level implants: A systematic review and meta-analysis. Ann Anat 2020; 231:151525.
- Klein M, Tarnow D, Lehrfield L. Marginal bone changes on ultraclean, micro-threaded platform-switched implants following restoration: 1 to 4 year data. Compend Contin Educ Dent 2020; 41:e7-e18.
- Amid R, Ardakani MRT, Tohidi R, et al. Bacterial microleakage at the implant-healing abutment interface in two different implant designs: Platform switching versus platform matching. J Long Term Eff Med Implants 2021; 31:33-42.
- Ellakany P, Mahrous AA, Al Eraky DM, et al. Evaluation of bacterial leakage in platform-switching dental implant with morse taper connection under thermocycling and loading effects: In vitro study. Int J Oral Maxillofac Implants 2021; 36:68-74.
- Cheng GL, Leblebicioglu B, Li J, et al. Soft tissue healing around platform-switching and platform-matching single implants: A randomized clinical trial. J Periodontol 2020; 91:1609-1620.
- Arora H, Khzam N, Roberts D, et al. Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2-5 year follow up. Clin Implant Dent Relat Res 2017; 19:694–702.
- Gjelvold B, Kisch J, Chrcanovic BR, et al. Clinical and radiographic outcome following immediate loading and delayed loading of single-tooth implants: Randomized clinical trial. Clin Implant Dent Relat Res 2017; 19:549–558.
- Sukekava F, Pannuti CM, Lima LA, et al. Dynamics of soft tissue healing at implants and teeth: A study in a dog model. Clin Oral Implants Res 2016; 27:545–552.
- Cheng GL, Leblebicioglu B, Li J, et al. Soft tissue healing around platform-switching and platform-matching single implants: A randomized clinical trial. J Periodontol 2020; 91:1609-1620.
- Lowy J, Kwon HS, Patel A, et al. The effect of platform-switching plus laser grooving on peri-implant hard and soft tissue level: A randomized, controlled, blinded clinical trial. Int J Periodontics Restorative Dent 2019; 39:669-674.
- Lago L, da Silva L, Gude F, et al. Bone and soft tissue response in bone-level implants restored with platform switching: A 5 year clinical prospective study. Int J Oral Maxillofac Implants 2017; 32:919-926.
- Luongo G, Simion M, Ferrantino L, et al. A prospective longitudinal clinical trial evaluating the preservation of the peri-implant hard and soft tissues. Int J Periodont Restorative Dent 2021; 41:e11-e17.
- Tokgöz SE, Bilhan H. The influence of the implant-abutment complex on marginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont 2021; 13:46-54.
Author Info
Amr Zahran1, Ahmed Mortada2, Maha Bahammam3 and Walid Elamrousy4*
1Department of Periodontology and Oral implantology, Egypt Cairo University, Egypt2Department of Periodontology and Oral implantology, Assiut University, Egypt
3Department of Periodontology, King Abdulaziz University, Jeddah, Saudi Arabia
4Department of Periodontology and Oral Medicine, Kafrelsheikh University, Egypt
Citation: Amr Zahran, Ahmed Mortada, Maha Bahammam, Walid Elamrousy,Peri-Implant Soft and Hard Tissues Evaluation around Immediately Placed New Implant Design: Randomised Clinical Study, J Res Med Dent Sci, 2021, 9(7): 263-270
Received: 22-Jun-2021 Accepted: 22-Jul-2021
