Case Report - (2022) Volume 10, Issue 12
Plummer Vinson Syndrome-A Case Report
Mohan Kumar J* and MK Rajasekar
*Correspondence: Dr. Mohan Kumar J, Department of ENT, Sree Balaji Medical College and Hospital, Chrompet, Chennai, India, Email:
Abstract
Plummer Vinson Syndrome (PVS) is a rare entity characterized by upper oesophageal webs and iron deficiency anaemia. Plummer Vinson Syndrome (PVS) also named as Patterson brown kelly syndrome is a combined presentation of three things dysphagia, iron deficiency anaemia and oesophageal webs, seen more often in middle aged females. We report a case of 65 years old female presented with chief complaints of dysphagia for more than 2 years, more for solid diet than liquid diet and also with complaints of dyspnoea on exertion and weight loss. On routine blood investigations she was found to be severe anaemic. Upper GI endoscopy revealed oesophageal web. Dilatation of oesophageal web was done, anaemia was corrected. Patient is on regular follow up with marked improvement in terms of weight gain and increased functional capacity.
marsbahis marsbahis mobilbahis 1xbet onwin betist piabella casino holiganbet holiganbet holiganbet mostbet mariobet meritking meritking meritking betnano casinoplus casinoplus betriyal casinoplus
Keywords
Plummer vinson syndrome, Palpitation, Predispose, Myoglobin, Upper oesophageal carcinoma
Introduction
Plummer Vinson Syndrome (PVS) also known as Paterson brown Kelly syndrome is an association of iron deficiency anaemia with koilonychias, angular stomatitis, glossitis and atrophy of oesophageal mucosa in the post cricoid region, which forms and obstructing web [1]. First described in 1912 by Henry Stanley Plummer, this disease is more prevalent among middle aged females [2]. The disease usually presents either with symptoms of anaemia fatigue, shortness of breath, palpitations and progressive dysphagia. His diagnosis of PVS relies on thorough history taking, general clinical examination, haematological investigation and radiological examination. On gross pathology, oesophageal web and oesophageal strictures are characteristic findings of PVS. On microscopic histopathological analysis, PVS presents with epithelial atrophy, chronic sub-mucosal inflammation and epithelial atypia or dysplasia in advanced cases [3,4]. Chronic irritation of the oesophagus may predispose to an increased risk of developing oesophageal webs or strictures. Common complications of PVS include hypo pharyngeal cancer, oesophageal cancer and oral cancer [5].
Case Presentation
A 65-year-old female presented to our hospital with complaints of difficulty to swallow solid food since the past two years, dyspnoea on exertion, episodes of palpitations and distinct weight loss. As per patient, symptoms progressed gradually to present level when she was able to take only soft diet and liquids and it takes her more time to finish the meal. Dysphagia was with solid foods only. The patient had also noticed her gradual weight loss and muscle wasting over the past two years. On examination height 165 cm, weight 45 kg and body mass index of 16.5 kg/m2. Patient had pallor with ridging of nails (Figure 1) and a bald tongue with tremor. On blood investigations haemoglobin of 8.1 g/dl, MCV 61.3, MCH 16.7. On peripheral smear it was microcytic hypochromic anaemia. Serum iron was low at 10 μg/dl, serum ferritin 3.8 and total iron binding capacity of 332 μg/dl and transferrin saturation of 8.6%. All other blood investigations found to be normal. On barium swallow examination persistent filling defect was noted at mid oesophagus (Figure 2). On upper Gastrointestinal (GI) endoscopy showed a narrowing in the upper oesophagus confirmed to be an oesophageal web (Figure 3). No other abnormality was seen. In this patient diagnostic endoscopy was performed with 5.5 mm scope that revealed narrow oesophageal lumen just below crico pharynx and scope could not pass beyond that. Hence a guide wire passed into the stomach. Savoury Gillard dilator set was used and dilated up to 11 sizes. Check endoscopy revealed dilated stricture area with no undue bleeding and other structures appeared normal and patient was treated with iron sucrose therapy for iron deficiency anaemia. Post dilatation patient improved symptomatically and discharged with regular follow up.
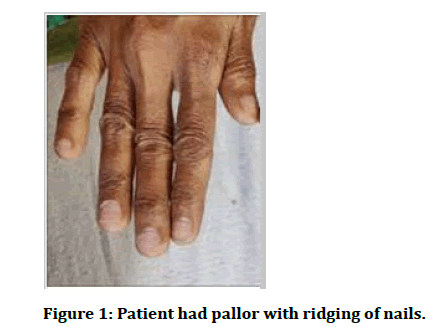
Figure 1: Patient had pallor with ridging of nails.
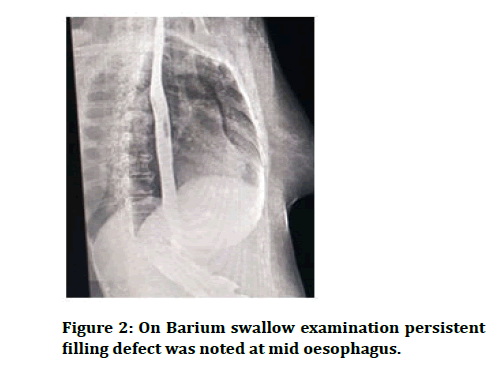
Figure 2: On Barium swallow examination persistent filling defect was noted at mid oesophagus.
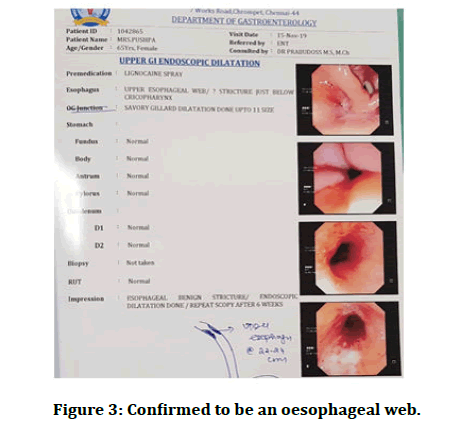
Figure 3: Confirmed to be an oesophageal web.
Discussion
PVS was highly suspected in this patient with iron deficiency anaemia and dysphagia; it was then confirmed after her barium swallow x-ray and UGI scope. The syndrome is a rare disorder characterized by a triad of iron deficiency anaemia, dysphagia and oesophageal webs [6]. The exact etiopathogenesis of PVS is unknown.
It is postulated that PVS results from iron deficiency [7]. Other possible factors include malnutrition, genetic predisposition and autoimmune disorders. In patients with iron deficiency, the iron dependent oxidative enzymes are unable to function at an optimum level and the dependent metabolic pathways such as oxidative phosphorylation are compromised. This promotes anaerobic metabolism leading to myasthenic changes in oesophageal muscles, which in turn forms oesophageal webs. The dysphagia is rarely due to oesophageal muscular disco-ordination [8,9]. Patients with iron deficiency have low levels of myoglobin which may affect the muscles of the tongue and lead to glossitis. Genes involved in the pathogenesis of iron deficiency anaemia associated with PVS include a mutation in the TMPRSS6 gene [10,11]. The TMPRSS6 gene encodes instructions for the protein hepcidin. Increased levels of hepcidin lead to decreased release of iron from ferritin and subsequently presents as iron deficiency anaemia. In case of significant oesophageal obstruction by multiple oesophageal webs or persistent dysphagia despite medical treatment, rupture and mechanical dilation of the web using an endoscope can be performed such as with our patient [12]
Conclusion
Since Plummer Vinson syndrome is a preventable cause of upper oesophageal carcinoma, prediction of dysphagia and questioning regarding dysphagia while taking history in patient presenting with iron deficiency is necessary and can prompt clinician for early intervention. Though literature projects Plummer Vinson syndrome as rare syndrome, seen in women with iron deficiency preceding dysphagia, in the present case patient had dysphagia for 1.5 years and was so trivial that only after iron deficiency anaemia symptoms prompted patient for visiting clinician. Hence in patients presenting with iron deficiency, taking history regarding any dysphagia can help clinicians to detect any cases of Plummer Vinson syndrome and thereby can initiate early interventions and regular surveillance.
References
- Malhotra P, Kochhar R, Varma N, et al. Paterson Kelly syndrome and celiac disease a rare combination. Indian J Gastroenterol 2000; 19:191-192.
- Verma S, Mukherjee S. Plummer Vinson Syndrome. Stat Pearls Publishing, 2019.
- Field Z, Russin M, Kropf J, et al. Plummer Vinson syndrome and heart failure: An unusual association in an African American woman. Am J Case Rep 2019; 20:1264-1267.
- Sanfrancesco J, Jones SJ, Hansel DE. Diagnostically challenging cases: What are atypia and dysplasia? Urol Clin North Am 2013; 40:281-293.
- Goel A, Bakshi AA, Soni N, et al. Iron deficiency anaemia and Plummer Vinson syndrome: Current insights. J Blood Med 2017; 8:175-184.
- Chung S, Roberts Thomson IC. Gastrointestinal: Upper oesophageal web. J Gastroenterol Hepatol 1999; 14:611.
- Mansell NJ, Jani P, Bailey CM. Plummer Vinson syndrome a rare presentation in a child. J Laryngol Otol 1999; 113:475-476.
- Huynh PT, de Lange EE, Shaffer HA Jr. Symptomatic webs of the upper oesophagus: Treatment with fluoroscopically guided balloon dilation. Radiol 1995; 196:789-792.
- Pinto J, de Jesus GN, Anselmo MP, et al. Iron refractory iron deficiency anaemia in dizygotic twins due to a novel TMPRSS6 gene mutation in addition to polymorphisms associated with high susceptibility to develop ferropenic anaemia. J Investig Med High Impact Case Rep 2017; 5:2324709617701776.
- Yaish HM, Farrell CP, Christensen RD, et al. Two novel mutations in TMPRSS6 associated with iron refractory iron deficiency anaemia in a mother and child. Blood Cells Mol Dis 2017; 65:38-40.
- Camaschella C, Silvestri L. Molecular mechanisms regulating hepcidin revealed by hepcidin disorders. Sci World J 2011; 11:1-10.
- Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anaemia. Am J Hematol 2016; 91:31-38.
Author Info
Mohan Kumar J* and MK Rajasekar
Department of ENT, Sree Balaji Medical College and Hospital, Chrompet, Chennai, IndiaCitation: Mohan Kumar J, MK Rajasekar, Plummer Vinson Syndrome-A Case Report, J Res Med Dent Sci, 2022, 10 (12): 038-040.
Received: 02-Sep-2022, Manuscript No. JRMDS-22-75753; , Pre QC No. JRMDS-22-75753(PQ); Editor assigned: 05-Sep-2022, Pre QC No. JRMDS-22-75753(PQ); Reviewed: 19-Sep-2022, QC No. JRMDS-22-75753; Revised: 21-Nov-2022, Manuscript No. JRMDS-22-75753(R); Published: 02-Dec-2022
