Research Article - (2022) Volume 10, Issue 10
Postoperative Complications of Surgery on the Thyroid Gland
Gopalsamy Santhanam Prabudoss*
*Correspondence: Dr. Gopalsamy Santhanam Prabudoss, Department of General Surgery, Sree Balaji Medical College and Hospital, Tamil Nadu, Chennai, India, Email:
Abstract
Thyroid cancer incidence is increasing, and with it, an increase in total thyroidectomy. There are limited studies comparing outcomes in total thyroidectomy performed in the inpatient versus outpatient setting. Major postoperative complications of thyroid surgeries include wound infection, hematoma/haemorrhage causing airway compromise, hypocalcaemia, recurrent or superior laryngeal nerve injury, and thyroid storm. In this study that was conducted in our hospital during the mentioned period, the clinical presentations, surgical procedures and post-operative complications were noted, analysed and compared with various standard studies. Thyroid disorders are common in females. No age group is exempted from thyroid disorders. However thyroid disorders are common in middle age group. Most common clinical presentation is asymptomatic solitary nodule of thyroid (40%). Incidence of malignancy is 10. Thyroid malignancy can present as enlarged neck nodes without thyromegaly. Post op IDL is useful to assess the vocal cord status especially in-patient who develop hoarseness/change in voice following surgery. Incidence of remnant laryngeal nerve paralysis following thyroid surgery found to be high in cases of thyroiditis 8 s malignancy
Keywords
Thyroid cancer, Thyromegaly, Laryngeal nerve paralysis, Thyroid surgery
Introduction
Disorders of the thyroid gland count as the second most common endocrine disorders trailing diabetes mellitus. Thyroid disorders warranting surgical intervention can be either benign tumours or malignant ones. Another reason for thyroid surgery is the swelling or enlargement of thyroid in the form of nodular or colloid goitre, when enlarged, causing difficulties in breathing, voice production, and swallowing. Total thyroidectomy has historically been performed as an inpatient surgery. Patients were admitted to hospital postoperatively due to the associated risk of life threatening complications including hypocalcaemia and airway obstruction, either due to bilateral Recurrent Laryngeal Nerve (RLN) injury or neck hematoma.
Major postoperative complications of thyroid surgeries include wound infection, hematoma/haemorrhage causing airway compromise, hypocalcaemia, recurrent or superior laryngeal nerve injury, and thyroid storm. Precise knowledge of the intricate anatomic details and meticulous surgical technique are prerequisite determinants for successful outcomes and to keep complications within acceptable limits. Postoperative HPT is a serious issue leading to prolonged hospital stay and increased expenditure. The aim of this present study involves the various surgical procedures and postoperative complications of surgery on the thyroid gland. To assess the different surgeries involving in thyroid gland. To study the technical details of procedure with morbid complications. To provides basic ideas for a safer surgery on the thyroid gland for the benefit of both the patient and the surgeon.
Materials and Methods
75 patients with thyroid swelling were studied prospectively between Jan 2002 to Jan 2004. All patients underwent thorough clinical examination in surgical clinic after registration. Patients who underwent surgery were included in this study. Patients were admitted at an appropriate period before surgery. Complete blood count, biochemical analysis chests X-ray, X-ray neck, thyroid function test were done for all cases. ECG was taken for persons above 40 years and with toxicity. Patients with toxic features were taken up for surgery only after control of hyper thyroid status. All patients were subjected to IDL by ENT dept. Most patients were subjected to FNAC and only in selective cases USG neck, CT (neck thorax was taken) patients were taken up for surgery in euthyroid status on day of surgery. All patients vocal cord movements was noted during extubation. Those patients who developed hoarseness of voice underwent postoperative IDL examination on 5/7th post-operative day by ENT department. Patients were followed up for 30-60 days. Intra op, immediate and late complications of surgical procedure was studied and analysed.
Exclusion criteria: Patients who required conservative treatment or who required medical management were excluded.
Results and Discussion
The following criteria are analysed and the data observed as below (Tables 1-7 and Figures 1-7).
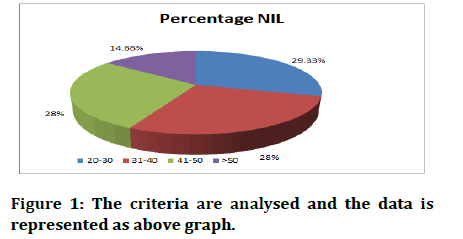
Figure 1: The criteria are analysed and the data is represented as above graph.
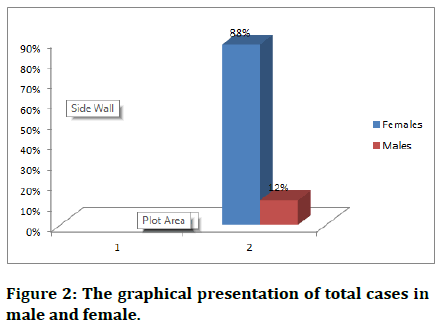
Figure 2: The graphical presentation of total cases in male and female.
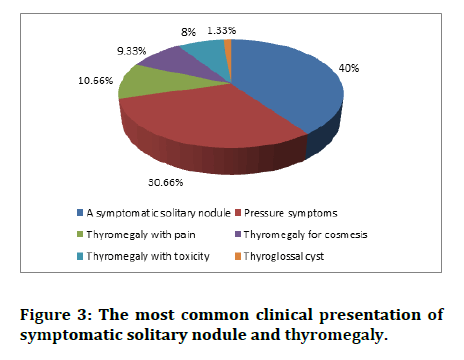
Figure 3: The most common clinical presentation of symptomatic solitary nodule and thyromegaly.
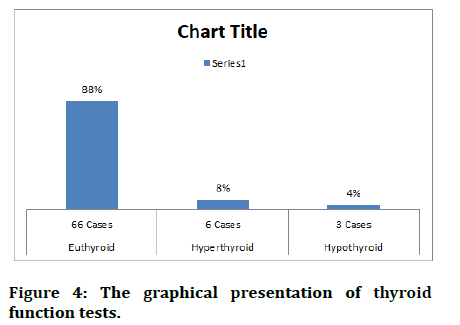
Figure 4: The graphical presentation of thyroid function tests.
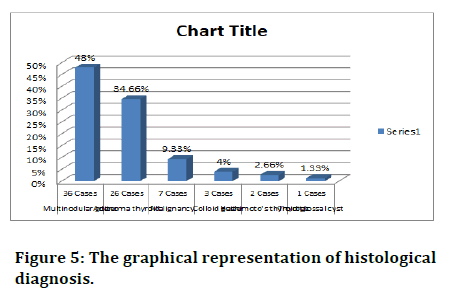
Figure 5: The graphical representation of histological diagnosis.
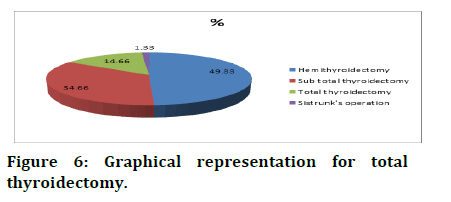
Figure 6: Graphical representation for total thyroidectomy.
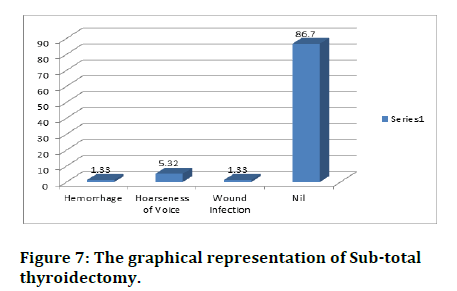
Figure 7: The graphical representation of Sub-total thyroidectomy.
| Age in years | No. | Percentage |
|---|---|---|
| 0-20 | NIL | NIL |
| 20-30 | 22 cases | 29.33% |
| 31-40 | 21 cases | 28% |
| 41-50 | 21 cases | 28% |
| >50 | 11 cases | 14.66% |
| Sex | ||
| Females | 66 Cases | 88% |
| Males | 9 Cases | 12% |
Table 1: Total no of cases (n)=75.
| Symptoms | ||
|---|---|---|
| Symptomatic thyromegaly | 44 Cases | 58.66% |
| A symptomatic thyromegaly | 31 Cases | 11.33% |
| Clinical Presentation | ||
| A symptomatic solitary nodule | 30 Cases | 40% |
| Pressure symptoms | 23 Cases | 30.66% |
| Thyromegaly with pain | 8 Cases | 10.66% |
| Thyromegaly for cosmesis | 7 Cases | 9.33% |
| Thyromegaly with toxicity | 6 Cases | 8% |
| Thyroglossal cyst | 1 Cases | 1.33% |
| Thyroid function test | ||
| Euthyroid | 66 Cases | 88% |
| Hyperthyroid | 6 Cases | 8% |
| Hypothyroid | 3 Cases | 4% |
Table 2: The clinical examination was studied and analysed.
| Multinodular goiter | 36 Cases | 48% |
| Adenoma thyroid | 26 Cases | 34.66% |
| Malignancy | 7 Cases | 9.33% |
| Colloid goiter | 3 Cases | 4% |
| Hashimoto's thyroiditis | 2 Cases | 2.66% |
| Thyroglossal cyst | 1 Cases | 1.33% |
Table 3: Histological diagnosis.
| Procedure | No. of Cases | % |
|---|---|---|
| Hemithyroidectomy | 37 | 49.33 |
| Subtotal thyroidectomy | 26 | 34.66 |
| Total thyroidectomy | 11 | 14.66 |
| Sistrunk's operation | 1 | 1.33 |
Table 4: Procedure done.
| Complications | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 4 | 1.33 | 1.33 | 6.65 | 4 | 1.33 | 2.66 | 6.66 | 6.66 | 2.66 | 62.72 |
| Hemi Thyroidectomy | ||||||||||
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 1.33% | 1.33 | 1.33 | - | - | - | 1.33 | - | - | - | 94.68 |
| Sub-total thyroidectomy | ||||||||||
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 1.33% | - | 1.33 | 1.33 | - | - | - | 5.33 | - | - | 90.69 |
| Total thyroidectomy | ||||||||||
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 1.33 | - | - | 5.32 | - | - | 1.33 | - | - | - | 86.7 |
Table 5: Intra, immediate and late complications of surgical procedure was studied and analysed.
| Sub-total thyroidectomy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 1.33% | - | 1.33 | 1.33 | - | - | - | 5.33 | - | - | 90.69 |
| Total thyroidectomy | ||||||||||
| Hemorrhage | Sinus formation | Preop Vocal Cord Palsy | Hoarseness of Voice | Unilateral Vocal Cord Palsy | Bilateral Vocal Cord Palsy | Wound Infection | Hypo Calcemia | Perioral Tingling and Numbness | Hypo Thyroidism | Nil |
| 1.33 | - | - | 5.32 | - | - | 1.33 | - | - | - | 86.7 |
Table 6: Total thyroidectomy has historically been performed and analysed.
| Edema of arytenoids | 5 Cases (6.66%) |
| Unilateral vocal cord palsy | 3 Cases (4%) |
| Right Hemi thyroidectomy side | 1 Case (1.33%) |
| Left side | 1 case (1.33%) |
| Bilateral | 1 case (1.33%) |
Table 7: Post-operative indirect laryngoscopy.
Details for total thyroidectomy
• Total thyroidectomy alone-8 cases
• Median sternotomy for retrosternal goiter-1 case
• Completion thyroidectomy for malignancy-1 case
• Radial next-dissection with total thyroidectomy for malignancy of thyroid-1 Case.
Pre-operative indirect laryngoscopy
Left side vocal cord movement found to be restricted in a case of multi nodular goiter with retrosternal extension (1.33%). All the other 74 cases IDL revealed normal study (98.66%)
Vocal cord movement on extubation
Vocal cords found to be not moving during excavation in 2 cases (2.55%) others than a case pre-operative left side restricted vocal cord movement (1.33%). All the other 72 cases vocal cords were moving during extubation (96%).
Post-operative indirect laryngoscopy
Post op indirect laryngoscopewas done in 5th or 7th post op day, only in patients who developed hoarseness or change in voice.
Those patients who had edema of arytenoids recovered within 7-14 days after surgery with conservative treatment.
One patient who had bilateral vocal cord paralysis developed stridor and underwent emergency tracheostomy (1.33%) and the patient was diagnosed histopathologically as a case of papillary carcinoma of thyroid that underwent total thyroidectomy.
Unilateral vocal cord palsy was reported in 4 cases, in post op IDL, out of these 4 cases (5.33) one case (1.33%) had pre op change in voice with restricted left side VOCAL CORD movement for retrosternal goiter underwent total thyroidectomy. Two cases (2.66%) diagnosed as thyroiditis of which, 1 case underwent hemithyroidectomy and other case underwent total thyroidectomy.
One case (1.33%) diagnosed as adenoma thyroid underwent Hemi thyroidectomy, had unilateral Vocal Cord paralysis. Surprisingly BL Vocal Cord palsy was missed on extubation, as was another patient with unilateral (R) side paralysis. It is understandable that edema of the arytenoids taken time to occur and hence not picked up on extubation.
Complications
Seroma: One case was reported in our study which is on par with other studies. This is the most common complication, which is due to sub cutaneous collection. It can be let out by aspiration and antibiotics to prevent further infection.
Haemorrhage: Three cases (4%) developed these complications. Out of the 3 cases, 2 patients (2.66%) had intra operative (Primary) Haemorrhage. One of the cases diagnosed to have huge MULTI NODULAR GOITER with inflammatory changes and other patient had retrosternal goitre. One patient (1.44%) had reactionary haemorrhage during immediate post op period and haemorrhage was controlled by re-exploration.
Infection: Two cases developed this complication. One patient was operated for Multi nodular goitre Subtotal thyroidectomy; other case was diagnosed as colloid goitre underwent Subtotal thyroidectomy. Both of these were treated with antibiotics.
Hoarseness of voice: Ten cases including transient hoarseness (5 cases), unilateral 4 cases including 1 case that had preoperative hoarseness, with restricted (L) side Vocal cord movement and one case of bilateral Vocal cord paralysis. Post op IDL was done for those patients who had Haemorrhage or change in voice in 5/7th Post- Operative Day. All the 10 cases were followed up for 4-6 weeks and were given speech therapy.
All the given cases (6.66%) that had edema of arytenoids and Haemorrhage recovered within 7-14 days. 4 patients including 1 case of pre-operative vocal cord palsy found to have unilateral Vocal cord paralysis and hoarseness of voice even after 6 wks.
Stridor: Two cases (2.66%) developed this complication. Both the patients were diagnosed as malignancy of thyroid and underwent total thyroidectomy later they developed stridor and underwent emergency tracheostomy and patients were shifted to ICU. Direct laryngoscopy was performed for both cases, one case found to have bilateral Vocal cord paralysis, another case diagnosed as tracheomalacia, a good premonitory is required to diagnose. It is easy to diagnose unilateral palsy rather than bilateral palsy on extubation.
Hypocalcaemia: Five cases (6.66%) developed this complication. All the patients underwent total thyroidectomy. Patients developed perioral tingling and numbness during 2 to 3 post-operative day. Trousseau's sign 86 chvostek's sign was demonstrated in few cases. Serum estimation of serum calcium was performed. Patients were with vitamin D 8s calcium supplements.
Hypothyroidism: Two cases (2.66%) developed this complication. Both cases underwent Subtotal thyroidectomy, which were not given replacement dose of thyroxin developed this complication. Out of 26 cases that underwent Subtotal thyroidectomy, 2 Patients developed hypothyroidism. Clinically; patients were normal whose serum thyroxin found to be low and TSH found to be high (Greater than 20 lu per ml) patients were treated with replacement dose of eltroxin.
Difficult intubation: 1 patient (1.33%) developed this complication that had Multi nodular goitre with toxic features. Patient was intubated with help of fibre optic bronchoscope.
Tracheomalacia: 1 patient (1.33%) developed this complication. Patient developed respiratory distress and stridor during immediate post op period, patient was intubated and ICU care was given. This patient required tracheostomy.
Mortality following thyroid surgery-NIL. We have compared our observation with the studies conducted on thyroid gland by Prof. Vittal, et al., Prof. N. Ananthakrishnan, et al., Prof. Prudencio S, Prof. Samson, et al., Christian Prof. A Seiler, et al., Prof. Giovanni Stuniolo, et al., Prof. Veena G, et al., Prof. Chandrasekar et al.
In our study thyroid disorders were more or less equally distributed between 2-4th decade of life which correlates with western and Indian studies. No age group is exempted from thyroid disease however thyromegaly requiring surgery in less than 20 years is rare. The maximum aged person in our study is 65 years 85 minimum aged patients is 21 years, with a mean age of 43 years, when compared with sansar, et al. (33 years), vital, et al. (34.08 years).The mean age in our study is slightly higher than the comparative studies.
Female-male ratio in our study is 7.4% correlates with the study by Samson, et al. (9:1) 8 and Giovanni stuniolo, et al. (6:1) but female-male ratio in our study found to be slightly higher than other Indian studies concluded by Vittal, et al. (4.6:1) and Chandrasekar, et al. (4.25:1) [2].
41.33% of our patients were a symptomatic including 9.33% of patients with malignancy correlates with the western study conducted by Samsan, et al. (47%) asymptomatic solitary nodule was found to be most common, clinical presentation.
30.66% of our patients presented with pressure symptoms including 6.66% of patients with retrosternal extension which is comparable with 38% in Samson et al study and 23.1% in Anathakrishnan, et al. study.
Toxic manifestations were seen among 8% of our patients which well correlates with Ananthakrishnan, et al. (7.9%) and Samson, et al. (7%) studies [1].
Multi Nodular Goiter found to be common histological diagnosis (48%) in our study. This is comparable with the study conducted by christian A seiler, et al. and Ananthakrishnanital (36.6%) [1,3].
Secondary intrathoracic goiter in our study is 5.3% in contrast with 24% in Giovanni Sturucola, et al. study. Primary intrathoracic goiter in seen is one of our patients (1.33%) in constrast to 11.5% in Giovanni sturniolo, et al. study [4].
The incidence of retrosternal goiter found to be higher in western studus when compared with Indian studies.
34.66% of patients were histologically diagnosed as adenonra which correlates with veena G, et al. (5.4%) But in christian A swiler, et al. study adenomas were only 9%. In our study 20 patients out of 26 cases with adenoma were clinically asymptomatic (76.9%).
Colloid goiter was found in 4% of our cases. But in Veena G, et al. study it was 11% and 1.2% in Anatha Krishnan, et al. study 2.66% of one patients were diagnosed as Hashimotos thyroiditis which correlates with the study by Ananthakrishnan, et al. (3.6%) and 6% by Bhanusali, et al. (9) and 2% in Christian, et al. study. But in other Indian studies conducted by Vittal etal (20%) and Veena G, et al. (14.8%) Kapoor, et al. 13.9%. The Incidence of Hashimoto thyroiditisis found to be higher in our study [1,3].
Malignancy were seen in 9.33% of our patients which correlates with the study of Vittal, et al. (12.6%), Veena G, et al. (5.26%) Christian A Seiler, et al. (13%) [3]. In our study Malignancy were seen in less than 10% of patients however incidence of Malignancy found to be more or less equal in Indian and western studies. All of our patients found to have papillary carcinoma with correlates with Veena G, et al. study which revealed 90% of malignancy was papillary. According to Vittal, et al. (57.3%) S.K. Salker, et al. (56%) the incidence of papillary carcinoma found to be less than our study.
Hemi thyroidectomy was done in 49.33% of cases of which is comparable with the study by Veena G, et al. (51.6%) in contrary to Samson, et al. (18.7%). Hemi thyroidectomy is commonest surgery done compared to other surgeries [5-7].
34.66% of patients underwent sub total thyroidectomy which correlates with Veena G, et al. study (22%) but western study by Samson, et al. shown sub total thyroidectomy is commonest surgery (81.3%) when compared to other surgeries. 14.66% of our patients under went total thyroidectomy but in Veena A, et al. it was only 4.2%.
Completion thyroidectomy was done after HP confirmation of Malignancy in one case (1.33%), which is comparable with the study of Giovanni sturniola, et al. (6.2%).
Near total thyroidectomy was done along with neck node block dissection for an occult thyroid carcinoma with secondary’s neck in 1 case (1.33%) which correlates with study by ananthakrishnan, (0.6%) et al. [1,8].
4% of our patients had primary and reactionary Haemorrhage but in Veena, et al. study, Haemorrhage was seen in only 0.5% of cases. Haemorrhage is fatal complication following thyroid surgery which should be controlled during surgery and drain should be placed. This high incidence could be because of surgeons at various levels performing thyroid surgery [9,10].
In our study 1 patient (Multi Nodular Goitre with retrosternal extension) had asymptomatic Vocal Cord paralysis (1.33%) preoperatively, which correlates with the study conducted by veena G, et al. (1.4%) and Giovanni sturniolo, et al. (0.6%). So it is important to do pre op IDL for all patients undergoing thyroid surgery to rule out pre-existing asymptomatic Vocal Cord paralysis and its medico legal aspect. However in our study malignancy of thyroid has no pre-operative IDL changes.
Transient hoarseness of voice was seen in 6.65% of patients; when compared to sanesan, et al. (3.2%) Hamad W, et al. (3.5), Veena G, et al. Surada, et al. (3.7%) studies. Temporary hoarseness found to be slightly higher in our study. All these patients were treated conservatively and became normal before discharge [11-13].
Unilateral vocal cord palsy was seen in 4% of patients which found to be slightly higher when compared to other studies like Veena G, et al. (.5%), Giovanni sturniolo, et al. (1.2%) [4]. because surgery in our study was done by various surgeons with varying experiences. So the incidence of unilateral vocal cord palsy in our study is slightly higher than other studies. 2 out of 3 patients developed unilateral vocal cord paralysis were histologically diagnosed as thyroiditis. So the incidence of recurrent laryngeal nerve palsy following thyroiditis is high. If a reasonable pre op diagnosis is established by antibody studies, surgery should not be undertaken unless absolute mandatory [14-20].
B/L vocal cord paralysis was noticed in 1.33% of patients comparable with 1.04% in Giovanni, et al. study. This patient was diagnosed as papillary carcinoma thyroid that underwent Total Thyroidectomy. This patient developed stridor 85 dyspnoea 6-8 hrs. after surgery underwent emergency tracheostomy. Direct laryngoscopy revealed B/L vocal cord paralysis. 2.66% of our patients had will infection post op which corresponds to the study by vital, et al. (2.5%). But in Sarkar, et al. study infection was found to be 10%.
Hypocalcaemia was seen in 6.66% of our cases which correlates with 7.2% in sarker, et al. study. But in western studies. Hypocalcaemia was seen in 2.4% of cases [21-30].
5 Patients (6.66%) who underwent total thyroidectomy developed perioral tingling 85 numbness on 48-72 hrs following surgery. Serum calcium was found to be less than normal value and patients were treated with calcium supplements.
Hypothyroidism was noticed in 2.66% of our patients which is comparable with 1.3% in vittal, et al. study. Both the patients underwent sub-total thyroidectomy and not supplemented with thyroxine. In hemi thyroidectomy the other lobe will be normal too and in Total Thyroidectomy replacement dose of eltroxin will be given so the chance of developing Hypothyroidism is high in sub-total thyroidectomy [31,32].
Conclusion
Thyroid surgery has undergone metamorphosis in hands of experimental innovative and courageous surgeons. So as we went through the hardships, the complications are bound to occur. It is only a good surgical mind that identifies and rectifies complications as they emerge early leaving less morbidity to our patients.
Some of the suggestions are put forward for the future young, budding, enthusiastic surgeons to bear in mind before they venture into this ocean, which appears calm.
Reference
- Ananthakrishnan N, Rao KM, Narasimhan R, et al. The single thyroid nodule-a south Indian profile of 503 patients with special reference to incidence of malignancy. Ind J Surg 1993; 55:487-492.
- Chandrasekar A, Raghunatha Rao. Goitres and thyroid cal in guntus, south Indian Surgical clinic. 98:265.
- Christian AS, Hans E, Coagner. Thy' GISI in an endemic region world. J Sci 1996; 20:593¬597.
- Sturniolo G, D'Alia C, Tonante A, et al. The recurrent laryngeal nerve related to thyroid surgery. Am J Surg 1999; 177:485-488.
- Ahkar FS. Thyroid imaging and function studies. Clin Nucl Med 1981; 15:106-131.
- Batin GR. Anatomy thyroid, thymus and parathyroids. Lee Mcgregor's Synopsis of Surgical Anatomy; 12th Edition 2018 By GAG Decker, DJ du Plessis. KM Verghese and Company. 1986; 198-207.
- Beaugie JM. Principles of thyroid surgery. Pitman Medical 1975.
- Melanie L Lyden, MD, MHPE. Surgical anatomy of thyroid gland. Mastery of Surgery. Little Brown and Company. 2022; 159-167.
- Block MA, Horn RC, Brush BE. The place of total thyroidectomy in surgery for thyroid carcinoma. Arch Surg 1960; 81:236-243.
- Brieger GH. Develoment of surgery. Textbook of Surgery. 13th edition Sabiston DC Jr. (ed). WE Saunders Company. 1986; 2-5.
- Chatterjee BP. Surgical diagnosis and methods of examination. New Central Book Agency. 1984; 158.
- Chaurasia BD. "Human anatomy Regional and applied". Voll 9th reprint New Delhi: CBS Publishers. 1990; 99.
- Chooison NW, Harness JX. Complications of total thyroidectomy for carcinoma. Surg Gyn obst 1970; 131:861-868.
- Clark, Orlo H, "Total thyroidectomy and lymphnode dissection for cancer of the thyroid". Chapter-24 in Mastery of Surgery-2 Edition Lloyd M Nyhus and Robert J. Baker, Boston, Little, Brown and Company. 1992; 204.
- Clarke RL. Ibanz ML. Kihit EC. What constitute adequate operation for carcinoma of thyroid. Irch Surg 1966; 92:23.
- Colcock BP. King ML Mortality and morbidity of thyroid surgery. Surg Gyn Obit 1962; 114:131-136.
- Cole WH "Carcinoma of the thyroid gland". Surg Gynaecol Obset. 1949; 88:349-352.
- Copenhaver WM, Douglas EK, Wood RL. "The thyroid gland" Chapter-21 in Bailey Text book of Histology, 7th Edn, Baltimore Williams and Wilkins company. 1978; 708-716.
- Das S. "The thyroid and parathyroids" in A concise textbook of surgery 1st edition Dr. S. Das Publisher. 1994; 655.
- Dobyns BM. Extended total thyroidecotmy with modified radical neck dissection for carcinoma. Mastery of Surgery. Nyhus LM. Baker RJ leds. Little Brown Company. 179-187.
- Dudley N. "The thyroid" Chapter-11.1 in Oxford Text book of surgery. Peter J. Morris and Ronald A malt, Oxford: Oxford University Press. 1994; 731-754.
- Ellelstyn CB. Total thyrodectomy and subtotal thyroidectomy. Mastery of Surgery. Nyhus LM. Baker RJ iedsl. Little Brown Company. 168-178.
- Foster RS Jr. Morbidity and mortality after thyroidectomy. Surg Gyn Obst 1978; 146:423-429.
- Franker DL, Monica S, Virginia L. "Thyroid tumours" Section-2 Chapter-37. In "Cancer: Principles and practice of Oncology" 5th Edition. Devita, Vincent T jr, Samuel Hellman, Steven a Rosenberg. Philadelphia, Lippincot Raven Publishers. 1629-1648.
- Ganong WF. Chapter-18: "The thyroid gland" in Review of Medical physiology 18th edition Connecticut: Prentice-Hall publishers. 1995; 297-307.
- Gharib H, Goellner JR. Fine needle aspiration biopsy of thyroid: A appraisal. Ann Intern Med 1993; 118:282-289.
- Gilliam FL. Warwick R. Eds: Gray's-anatomy. 36th edition, Churchill Livingstone. 1980; 1449.
- Harding Rain KJ, Manny CY. Bailey and Love. short practice of sorjery. 2ULh ed. English Language Book Society. 1988; 660.
- Harrison T. Historical aspects and anatomy of thyroid gland. Text Uook of Surgery, 13th edition SabisLon DC Jr. led). US Saunders Company. 1986; 579-580.
- Hollinshed WH. Anatomy for surgeons. Harper and Row 1982; 2:517-531.
[Indexed]
- Johnstone J, Mann R, Rintoul RF. Forquharsonl Textbook of Operative Surgery. Rintoul Rr 7th edition 1986 reprinting. 1992; 256-262.
- Liardin J. Carciloma of thyroid gland. Surg Gyn Obst 1971; 132:450.
Author Info
Gopalsamy Santhanam Prabudoss*
Department of General Surgery, Sree Balaji Medical College and Hospital, Tamil Nadu, Chennai, IndiaCitation: Gopalsamy Santhanam Prabudoss, Postoperative Complications of Surgery on the Thyroid Gland, J Res Med Dent Sci, 2022, 10 (10): 122-129.
Received: 29-Jul-2022, Manuscript No. JRMDS-22-57367; , Pre QC No. JRMDS-22-57367(PQ); Editor assigned: 01-Aug-2022, Pre QC No. JRMDS-22-57367(PQ); Reviewed: 16-Aug-2022, QC No. JRMDS-22-57367; Revised: 30-Sep-2022, Manuscript No. JRMDS-22-57367(R); Published: 10-Oct-2022
