Research - (2019) Volume 7, Issue 5
Post-orthodontic Pharyngeal Airway Changes Following First Premolar Extraction and Incisor Retraction in Bimaxillary Protrusion PatientsâÂÂA Retrospective Study
Alqahtani Nasser1*, Rana Alshammari2, Thikriat Al-Jewair3, Mohammad Aldosari1 and Albarakati Sahar1
*Correspondence: Alqahtani Nasser, Pediatric Dentistry and Orthodontics Department, College of Dentistry, Riyadh, Saudi Arabia, Email:
Abstract
Objectives: The goals of orthodontic treatment are not only limited to correcting malocclusion and facial appearance but also extend to achieving normal function of the stomatognathic system and airway patency. This study aimed to investigate postorthodontic pharyngeal airway changes after the extraction of the four first premolars with subsequent retraction of the incisor teeth in patients with bimaxillary protrusion.
Materials and methods: Pre- and post-treatment cephalometric radiographs of adult patients (age range 18-30 years) who underwent orthodontic therapy for class I bimaxillary protrusion from April to July 2018 were obtained. Fixed orthodontic therapy following first premolar extraction was the absolute inclusion criteria. Cephalometric measurements of dental (upper and lower incisor retraction and retroclination) and pharyngeal airway (tongue length and height, soft palate height, superior, middle and inferior airway spaces, vertical airway length) variables were identified. Collected data was analyzed with SPSS® software. Paired t-test, Pearson’s correlation and linear regression analysis were done with statistical significance set at 95% (p-value<0.05).
Results: A total of 46 patients (16 male and 30 female) were included in the study. Statistically significant difference was evident in the mean values of pre- and post-treatment pharyngeal airway variables like soft palate thickness (0.35 mm, p<0.001), superior airway space (0.69 mm, p<0.001), and middle airway space (0.66 mm, p<0.001). Based on linear regression, retroclination of the lower incisors by 1° could predict a 0.736 mm increase in tongue length, up to 12% of times. Similarly, a 0.043 mm decrease in middle airway space could be predicted up to 17% of times following lower incisor retraction by 1 mm.
Conclusion: First premolar extraction and orthodontic retraction of incisor teeth results in significant reduction of soft palate thickness and superior and middle airway spaces. Comprehensive pre- and post-orthodontic evaluation of the soft palate, tongue and pharynx should be mandated to avoid pharyngeal airway compromise.
Keywords
Bimaxillary protrusion, Pharyngeal airway space, Cephalometric analysis, Orthodontic therapy, Incisor retraction
Introduction
Bimaxillary protrusion (BMP) is a clinical condition classified by protrusive and proclined upper and lower incisors, and procumbent lips. The unaesthetic appearance caused by the presence of circumoral convexity, despite a straight facial profile and Class I molar relationship, often forms the rationale for orthodontic management. Recently, airway health has been asserted as a primary consideration before starting orthodontic treatment, especially when associated with premolar extractions [1]. The assessment of the upper airway is an important foundation because of its role in swallowing, respiration, pronunciation, and combined effects over malocclusion and the stability of orthodontic treatment outcomes [2].
Orthodontic treatment in BMP patients with a class I molar relationship, often involves extraction of all the first or second premolar teeth, followed by retraction of anterior teeth [3,4]. This not only results in soft tissue profile changes, but also contributes to changes in the upper airway space [5]. Post-orthodontic pharyngeal airway changes occur primarily as a result of retraction of the anterior teeth, which alters the arch dimension and in turn affects the tongue position [6]. These positional changes in the oral cavity influence the size and function of the pharyngeal airway space (PAS), thereby affecting breathing [7]. Moreover, orthodontic diagnosis and prognosis of BMP patients can be strongly influenced by the pre- and posttreatment tongue pressure [8]. Therefore, measurements of upper airway dimensions are considered a critical variable for evaluation of post-treatment soft tissue profile changes [9].
The various modalities used in airway assessment includes nasal endoscopy, rhinomanometry, acoustic rhinometry, cephalometric analysis, computed tomography, magnetic resonance imaging and cone-beam computed tomography(CBCT) [6]. Traditionally, for orthodontic patients, assessment of the upper airway alterations is done clinically supported with lateral cephalograms. Although, only limited information is obtained by the 2D reconstruction of the airway in comparison to a CBCT, it is greatly preferred as the latter is not part of the routine examination and poses greater risk of radiation exposure [6]. Although cephalometric measurements of the PAS are two-dimensional, these measurements have been proven to be a reliable diagnostic tool for assessing pharyngeal volumes [10]. Cephalometric measurements of the PAS as a part of post orthodontic analysis have been reported as early as 1988 by deBerry- Borowiecki et al. [11]. The analysis of PAS is reportedly performed at three different levels, based on their parallelism with a cephalometric reference line connecting point B (most concave point on mandibular symphysis) to gonion (Go) (most postero-inferior point on angle of mandible). The first level is the superior posterior airway space (SPAS) measuring the anteroposterior width of the airway posterior to the soft palate. The second level is the middle airway space (MAS), measured anteroposteriorly along the tip of the uvula and the lowest level is the inferior airway space (IAS), measured anteroposteriorly along the Go-B line Germec- Cakan et al. [8] concluded that extraction of four premolars and retraction of anterior teeth with maximum anchorage resulted in a reduction of the uvulo-glossopharyngeal dimensions [8]. Based on a similar study, Wang et al. [12] reported that the dimensions of the velopharynx and glossopharynx decreased following maximal retraction of anterior teeth [13]. Sharma et al. evaluated the upper airway dimensions in adolescent BMP patients treated with first premolar extraction, and reported that extraction of premolars had a detrimental narrowing effect on the oropharyngeal structures [9].
While orthodontic treatment is focused towards altering the dentoskeletal framework, it may produce desirable or undesirable changes in the external or integumental contours of the face [4]. According to ethnic variations, the soft tissue response to orthodontic treatment may vary in thickness, tone, and length [8]. The above factors help predict future stability and patient satisfaction, especially in clinical scenarios involving orthodontic retraction following extraction of teeth [4,8]. Studies have evaluated the soft tissue response and upper airway changes in BMP patients treated orthodontically with the extraction of upper and lower premolars, in several ethnic groups [4,12,14-17]. However, there are not many studies reporting the same in a middle-eastern population. Furthermore, the effect of incisor retraction on the pharyngeal airway dimensions has not been reported widely. Therefore, the aim of the present retrospective study was to investigate post-orthodontic pharyngeal airway changes in patients with bimaxillary protrusion who were treated by extraction of the four first premolars followed by retraction of the incisors.
Materials and Methods
Following ethical approval from the Institutional Review Board (CDRC Approval No. FR-0439 / IRB. No. E-18-3029), cephalometric radiographs of adult BMP patients who underwent orthodontic retraction of anterior teeth following extraction of all first premolars were included. The sampling frame included all patients reporting to a dental center between April 2017 and July 2018, and fulfilling the following inclusion criteria:
• Harmonious facial profile with an ANB (A point–Nasion–B point) angle of 3° ± 2.3 and an SN-MP (Sella-Nasion to Mandibular plane) angle of 32° ± 5.
• Class I molar relationship with an interincisal angle of 110.4° ± 6, overjet of 3 ± 1 mm, and overbite of 1.4 ± 1 mm [18].
• Treated using fixed orthodontic appliance and availability of pre and post-treatment cephalometric radiographs of adequate diagnostic quality.
• Absence of functional appliance therapy or orthognathic surgical procedures as a part of treatment.
• Absence of congenitally missing teeth (excluding third molars).
No medical history of pharyngeal pathology and/ or nasal obstruction, snoring, obstructive sleep apnea, adenoidectomy, or tonsillectomy.
Based on evidence from previously published data [15-17], and assuming a statistical power of 80% with 95% confidence level, the sample size was estimated to be 42 patients (EPI Info 7-StatCalc, CDC, Atlanta, USA). Patient records identified using the inclusion criteria were assigned unique reference numbers by a blinded operator and were randomly included to the study using an online random number generator (RANDOM.ORG, Dublin, Ireland). Pre and post treatment digital cephalometric radiographs of the study patients were collected for analysis. All the radiographs were obtained using a Planmeca Proline XC CEPH Digital X-Ray Unit (Planmeca OY, Helsinki, Finland) set at 80 kV with total filtration 2.5 mm Al and 1500 VA 50 Hz. Bias arising as a result of differing treatment methodologies was avoided by selecting records of patients treated by a single orthodontist with fixed edgewise (0.018” slot) mechanotherapy using maximum anchorage (Nance appliance) in the upper arch.
Analysis of the digital cephalometric radiographs was done using Dolphin Imaging® Software, Version 10.0 (Dolphin Imaging and Management Solutions, Chatsworth, California, USA). The magnification probability was eliminated through calibration of the actual length of the ruler on the head positioner with simultaneous identification of the two ends of the rulers and the anatomical landmarks (Figure 1 and Figure 2). To assure examiner reliability, samples of 10 randomly selected cephalometric radiographs were traced and measured by the same investigator, who would eventually trace all the radiographs. Identification of the cephalometric landmarks and measurement of the variables were carried out in two different sessions separated by a period of two weeks. In order to ascertain the test-retest reliability, the mean values of the variables obtained during the two sessions were compared using paired t-tests. Furthermore, Pearson’s correlation was done to evaluate the relationship between the first and second readings and negligible error was assumed for a minimum correlation coefficient (Pearson’s r) of 0.75.
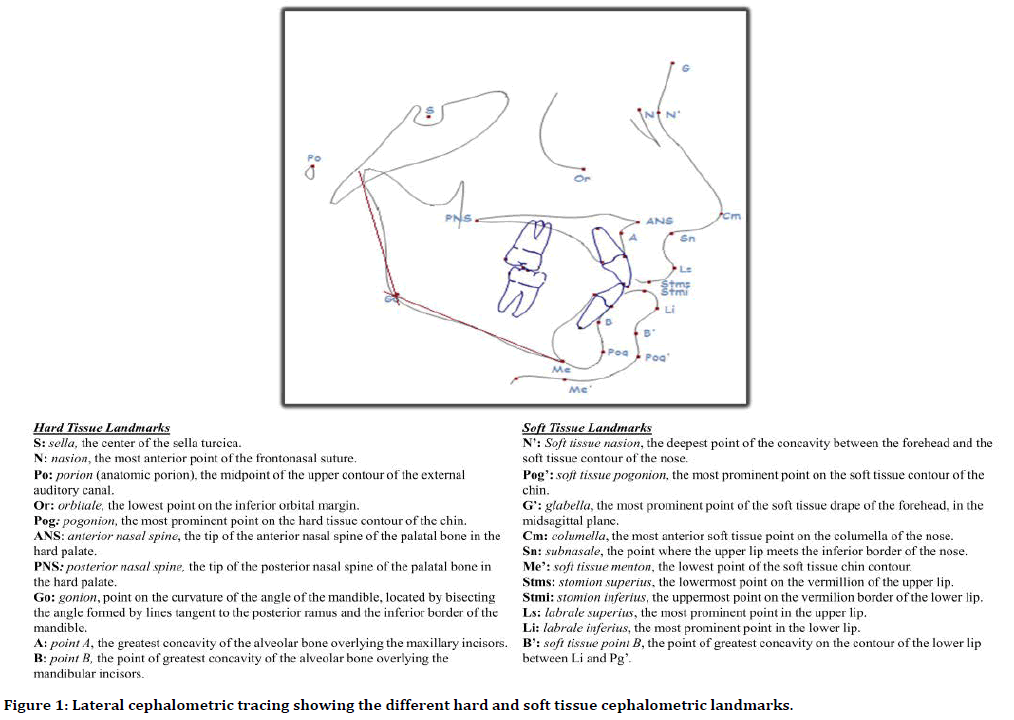
Figure 1. Lateral cephalometric tracing showing the different hard and soft tissue cephalometric landmarks.
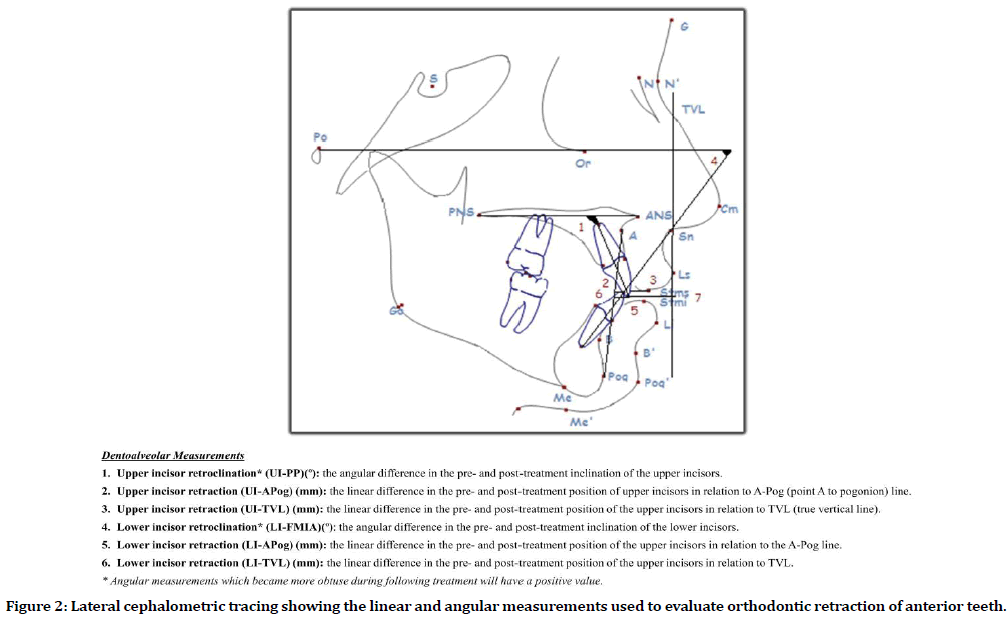
Figure 2. Lateral cephalometric tracing showing the linear and angular measurements used to evaluate orthodontic retraction of anterior teeth.
Pre- and post-treatment cephalometric data were analyzed using the SPSS PC+ version 21.0 for Windows, (IBM SPSS Statistics, Armonk, NY, USA). Descriptive statistics (mean and standard deviation) were calculated for all the quantitative outcome variables (dental and airway). The preand post-test mean values of the quantitative variables were compared using a student’s paired t-test, with the resulting difference being the variable of interest. To quantify the correlation between the difference in the pre- and posttreatment values of the variables, Pearson’s correlation was used. Linear regression analysis was used to identify the independent predictor variables (changes in dental measurements) for the dependent outcome variables (changes in pharyngeal airway measurements) of interest. The statistical significance of the results was fixed at a p-value <5% (α=0.05) and at 95% confidence interval.
Results
A total of 46 patient records (16 males and 30 females) fulfilling the inclusion criteria were identified and included in the study. Pretreatment and post-treatment cephalometric analysis was done based on standardized cephalometric hard-tissue and soft-tissue landmarks as described in Figure 1. Angular and linear measurements relating to incisor teeth retraction as a part of orthodontic treatment of BMP was recorded (Figure 2). Similarly, linear pharyngeal airway, soft palate and tongue measurements were obtained using the cephalometric analysis (Figure 3).
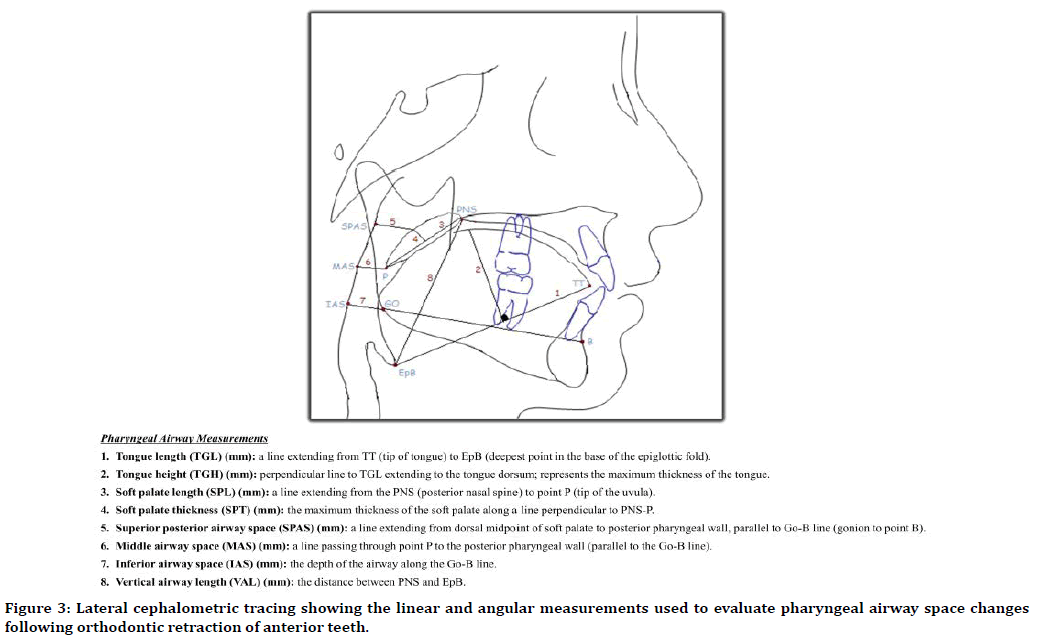
Figure 3. Lateral cephalometric tracing showing the linear and angular measurements used to evaluate pharyngeal airway space changes following orthodontic retraction of anterior teeth.
A statistically significant correlation was found between the test and retest values of all dental and airway variables (Table 1). The values for correlation coefficient (Pearson’s r) ranged from 0.834 to 0.988, and were considered reliable to highly reliable. Moreover, paired t-test of the test and re-test values for the variables indicated no statistically significant differences. The above results of reliability testing indicated intra-observer agreement and validity of the tool used to measure the dental and airway related cephalometric variables. Comparison of the mean difference of pre- and post-treatment cephalometric variables between the male and female patient records, revealed no statistically significant differences (Table 2). Therefore, the combined data obtained from the records of all 46 patients included in the study were used for further statistical comparisons.
| Cephalometric Measurements | Correlation coefficient (r) | p-value |
|---|---|---|
| Dental variables | ||
| Upper incisor retroclination (UI-PP)(º) | 0.914 | <0.001 |
| Upper incisor retraction (UI-APog’) (mm) | 0.969 | <0.001 |
| Upper incisor retraction (UI-TVL) (mm) | 0.941 | <0.001 |
| Lower incisor retroclination (LI-FMIA)(º) | 0.911 | <0.001 |
| Lower incisor retraction (LI-APog’) (mm) | 0.988 | <0.001 |
| Lower incisor retraction (LI-TVL) (mm) | 0.913 | <0.001 |
| Airway variables | ||
| Tongue length (TGL) (mm) | 0.939 | <0.001 |
| Tongue height (TGH) (mm) | 0.985 | <0.001 |
| Soft palate length (SPL) (mm) | 0.976 | <0.001 |
| Soft palate thickness (SPT) (mm) | 0.871 | 0.001 |
| Superior airway space (SPAS) (mm) | 0.834 | 0.003 |
| Middle airway space (MAS) (mm) | 0.985 | <0.001 |
| Inferior airway space (IAS) (mm) | 0.957 | <0.001 |
| Vertical airway length (VAL) (mm) | 0.979 | <0.001 |
Table 1: Reliability test for the cephalometric measurements using correlation between the test and retest values, and their significance (n=10).
| Cephalometric Measurements | Mean difference in pre- and post-treatment values | ||
|---|---|---|---|
| Male (n=16) | Female (n=30) | p-value | |
| Dental variables | |||
| Upper incisor retroclination (UI-PP)(º) | 9.89 | 9.12 | 0.184 |
| Upper incisor retraction (UI-APog’) (mm) | 4.13 | 4.09 | 0.967 |
| Upper incisor retraction (UI-TVL) (mm) | 3.93 | 3.72 | 0.783 |
| Lower incisor retroclination (LI-FMIA)(º) | -10.09 | -9.44 | 0.555 |
| Lower incisor retraction (LI-APog’) (mm) | 9.85 | 9.26 | 0.755 |
| Lower incisor retraction (LI-TVL) (mm) | 3.75 | 3.51 | 0.639 |
| Airway variables | |||
| Tongue length (TGL) (mm) | 0.77 | 1.2 | 0.368 |
| Tongue height (TGH) (mm) | -0.71 | -0.15 | 0.172 |
| Soft palate length (SPL) (mm) | 0.25 | 0 | 0.642 |
| Soft palate thickness (SPT) (mm) | 0.35 | 0.35 | 1 |
| Superior airway space (SPAS) (mm) | 0.7 | 0.69 | 0.955 |
| Middle airway space (MAS) (mm) | 0.52 | 0.74 | 0.245 |
| Inferior airway space (IAS) (mm) | -0.27 | -0.33 | 0.901 |
| Vertical airway length (VAL) (mm) | -0.57 | -0.4 | 0.79 |
Table 2: Comparison of mean difference in pre and post treatment cephalometric variables between male and female study population.
Comparing the mean pre- and post-treatment dental cephalometric variables, a highly significant mean difference (p ≤ 0.001) was observed for all the measured parameters. This was indicative of successful anterior teeth (upper and lower incisors) retraction and retroclination associated with orthodontic correction of BMP (Table 3). This was associated with a decrease in tongue length (TGL), soft palate length (SPL) and thickness (SPT), superior airway space (SPAS) and middle airway space (MAS). On the contrary, an increase in tongue height (TGH), inferior airway space (IAS) and vertical airway length (VAL) was observed. Nevertheless, the above changes in airway measurements were statistically significant (p<0.001) only for SPT, SPAS and MAS, with a mean reduction of 0.35 mm, 0.69 mm and 0.66 mm respectively (Table 3).
| Cephalometric Measurements | Mean pre-treatment value (± S.D.) | Mean post-treatment value (± S.D.) | Mean difference | p-value | 95% | C.I. |
|---|---|---|---|---|---|---|
| Dental variables | ||||||
| Upper incisor retroclination (UI-PP)(º) | 122.4 ± 4.7 | 109.6 ± 5.1 | 9.6 | <0.001* | 4.5 | 14.7 |
| Upper incisor retraction (UI-APog’) (mm) | 36.1 ± 2.9 | 26.9 ± 3.6 | 4.1 | <0.001* | 0.5 | 7.7 |
| Upper incisor retraction (UI-TVL) (mm) | 3.58 ± 2.1 | 0.83 ± 2.3 | 3.8 | <0.001* | 2.3 | 4.19 |
| Lower incisor retroclination (LI-FMIA)(º) | 48.9 ± 3.0 | 58.6 ± 3.3 | -9.65 | <0.001* | -10.7 | -8.6 |
| Lower incisor retraction (LI-APog’) (mm) | 35.7 ± 5.0 | 26.3 ± 5.8 | 4.1 | 0.001* | -1.7 | 9.9 |
| Lower incisor retraction (LI-TVL) (mm) | -0.61 ± 2.8 | -3.24 ± 2.2 | 3.6 | <0.001* | 0.8 | 6.42 |
| Airway variables | ||||||
| Tongue length (TGL) (mm) | 75.8 ± 10.4 | 75.3 ± 8.6 | 0.5 | 0.62 | -1.6 | 2.6 |
| Tongue height (TGH) (mm) | 34.7 ± 2.3 | 34.8 ± 2.7 | -0.15 | 0.61 | -0.75 | 0.45 |
| Soft palate length (SPL) (mm) | 35.9 ± 4.7 | 35.8 ± 4.9 | 0.3 | 0.73 | -0.42 | 0.59 |
| Soft palate thickness (SPT) (mm) | 9.9 ± 1.6 | 9.6 ± 1.6 | 0.35 | <0.001* | 0.21 | 0.48 |
| Superior airway space (SPAS) (mm) | 13.2 ± 1.7 | 12.5 ± 1.8 | 0.69 | <0.001* | 0.43 | -0.96 |
| Middle airway space (MAS) (mm) | 11.6 ± 1.5 | 10.9 ± 1.5 | 0.66 | <0.001* | 0.48 | 0.85 |
| Inferior airway space (IAS) (mm) | 12.6 ± 7.6 | 12.9 ± 7.9 | -0.31 | 0.19 | -0.77 | 0.15 |
| Vertical airway length (VAL) (mm) | 59.7 ± 4.2 | 60.1 ± 3.7 | -0.45 | 0.11 | -1 | 0.11 |
Table 3: Comparison between the mean values of pre- and post-treatment cephalometric dental and airway variables, and their significance. (n=46).
Pearson’s correlation between dental and airway variables revealed significant negative correlation between lower incisor (LI) retroclination and TGL (r=-0.736), and positive correlation between LI retraction and MAS (r=0.043) (Table 4). Within the airway variables, significant positive correlation was observed between TGL and MAS, TGH and SPAS, and TGH and VAL (Table 4). Linear regression analysis, with the dental variables as independent predictors and airway variables as the dependent outcomes (Table 5), indicated statistically significant changes in TGL and MAS, associated with changes in LI retroclination and retraction respectively (Table 6). Retroclination of the lower incisors by 1° could predict a 0.736 mm increase in TGL, up to 12% of times. Similarly, a 0.043 mm decrease in MAS could be predicted up to 17% of times following lower incisor retraction by 1 mm (Table 6).
| Cephalometric measurements | Dental variables | Airway variables | |||||
|---|---|---|---|---|---|---|---|
| Lower incisor retroclination | Lower incisor retraction | Tongue length | Tongue height | Superior airway space | Middle airway space | Vertical airway length | |
| Lower incisor retroclination (LI-FMIA)(º) | - | -0.736 | |||||
| Lower incisor retraction (LI-APog’) (mm) | - | 0.043 | |||||
| Tongue length (TGL) (mm) | -0.736 | - | 0.293 | ||||
| Tongue height (TGH) (mm) | - | 0.415 | 0.464 | ||||
| Superior airway space (SPAS) (mm) | 0.415 | - | |||||
| Middle airway space (MAS) (mm) | 0.043 | 0.293 | - | ||||
| Vertical airway length (VAL) (mm) | 0.464 | - | |||||
Table 4: Statistically significant (p<0.05) correlation (Pearson’s r) between the mean pre- and post-treatment difference among the different cephalometric dental and airway variables. (n=46).
| Independent (Dental) variables | Dependent (Airway) variables |
|---|---|
| Upper incisor retroclination (UI-PP)(º) | Tongue length (TGL) (mm) |
| Upper incisor retraction (UI-APog’) (mm) | Tongue height (TGH) (mm) |
| Upper incisor retraction (UI-TVL) (mm) | Soft palate length (SPL) (mm) |
| Lower incisor retroclination (LI-FMIA)(º) | Soft palate thickness (SPT) (mm) |
| Lower incisor retraction (LI-APog’) (mm) | Superior airway space (SPAS) (mm) |
| Lower incisor retraction (LI-TVL) (mm) | Middle airway space (MAS) (mm) |
| Inferior airway space (IAS) (mm) | |
| Vertical airway length (VAL) (mm) |
Table 5: Dependent and independent variables used in multiple regression. (n=46).
| Change in independent (dental) variables | Change in dependent (airway) variables | r | p-value | r2 |
|---|---|---|---|---|
| Lower incisor retroclination (LI-FMIA)(º) | Tongue length (TGL) (mm) | -0.736 | 0.038 | 12% |
| Lower incisor retraction (LI-APog’) (mm) | Middle airway space (MAS) (mm) | 0.043 | 0.007 | 17% |
Table 6: Statistically significant (p<0.05) Predictors (changes in dental variables) influencing pharyngeal airway changes based on multiple regression. (n=46).
Discussion
Factors that can modify the posture or the position of the tongue and soft palate, such as mode of breathing, body mass index, age, gender, tongue hypertrophy, or ethnicity, may increase or decrease the airway dimensions [19]. This change in airway dimensions can degrade quality of life or lead to a life-threatening condition, such as obstructive sleep apnea [20]. The results of this study showed a significant decrease in soft palate thickness by a mean of 0.35 mm, which could have been due to backward displacement of the tongue and its corresponding pressure on the soft palate. While there were no significant changes observed in TGL, TGH, IAS and VAL measurements, the superior and middle airway spaces decreased in anteroposterior length by 0.69 mm and 0.66 mm respectively (Table 3). This indicates a reduction in nasopharyngeal and palatopharyngeal dimensions following incisor retraction for BMP correction.
Reduction in upper pharyngeal airway cephalometric measurements have been reported following rapid maxillary expansion [21], facemask therapy for maxilla-mandibular skeletal protraction [22], and orthognathic surgery for maxilla-mandibular skeletal prognathism [23,24]. In terms of reduction in airway space following premolar extraction, there have been contradicting reports especially among adolescent orthodontic patients. While Sharma et al. [9] reported reduction in PAS following first premolar extraction and anterior teeth retraction, Valiathan et al. [25] reported no significant airway changes in the long term. According to them this was attributable to the continued mandibular growth in adolescent age group [25]. The present study included only adult BMP patients treated orthodontically. Nevertheless, the results indicate a definite reduction in at least the superior and middle airway spaces following first premolar extraction and anterior teeth retraction. Moreover, these findings are in coherence with that reported in an earlier study involving class II BMP patients. This study by Kikuchi et al. [26] reported that, BMP patients treated by premolar extraction were found to have PAS reduction. On the contrary patients treated using Herbst functional appliance, in the same study, had a marginal increase in PAS in the latter [26].
In addition, the present study showed that there was a 12% chance of predicting change in tongue length by observing the angular change in degree of lower incisor retroclination. Similarly, the linear change in lower incisor retraction had a 17% chance of predicting changes in the MAS, corresponding to the palatopharyngeal airway. Wang et al. [12] reported that reduction in PAS and change in tongue measurements are due to changes in hyoid position following lower incisor retraction. They reported a mean reduction of superior, middle and inferior airway space by 0.56 mm, 0.85 mm and 1.63 mm respectively, following orthodontic retraction of lower incisors [12]. Similarly, Tong et al. [27] reported reduction in the superior, middle and inferior airway space dimensions ranging from 21% to 38%, following lower incisor retraction. The above reductions reported in SPAS and MAS are similar to that of the present study. However, there was an increase in IAS by 0.31 mm, which though not statistically significant, could be attributed only to the differences in the ethnicity of the study populations. In a study conducted among middle-eastern subjects, Al Maaitah et al. [14] reported a reduction in tongue space and soft palate thickness, following premolar extraction and orthodontic treatment. The above observation is significant considering the fact that it was similar to findings in the present study, which was also based on records obtained from middle-eastern subjects. Based on a study in Indian population, Bhatia et al. [19] reported significant reduction in PAS ranging from 16% to 22%, along with a 11% change in hyoid position following orthodontic treatment of Class I BMP. On the contrary, Nuvusetty et al. [4] reported no significant changes in PAS measurements following orthodontic treatment of Indian class I BMP patients.
Similar to the results of the current study, majority of the afore-mentioned studies indicated a reduction in PAS following premolar extraction and/or lower incisor retraction, without any change in the VAL. Nevertheless, ethnic differences among patients might affect the severity of reduction in PAS [28]. Moreover, differences in the facial pattern have also been proposed to affect PAS reduction following orthodontic retraction of anterior teeth [29]. Wherein, brachyfacial individuals with class I malocclusion are considered to be least affected in comparison to mesofacial and dolichofacial patterns [29].
One of the major limitations of the present study was the ethnicity of the study population, which was mainly from middle-eastern descent [18], there are no studies exclusively evaluating their pharyngeal airway anatomy and its response to orthodontic therapy. Nevertheless, the findings of the present study are coherent with several previous studies, as mentioned earlier, evaluating PAS changes following orthodontic treatment of BMP. Further, the craniocervical inclination primarily influenced by extension and flexion of the patient head has an evident effect over PAS established by 2D cephalometric evaluations. However, the intricate variations in the craniocervical “pitch” during the treatment sessions can be better assessed only by 3D (CBCT) examinations [30]. Interestingly, the lateral cephalograms can be utilized for understanding the effects on nasopharyngeal spaces in patients over 15 years of age due to the stability of the craniofacial complex achieved at this age [31].
In addition to evaluating the effect of first premolar extraction and anterior teeth retraction, the present study also analyzed a linear regression model to predict PAS changes following lower incisor retraction and retroclination. Since lower incisor retraction and retroclination are the corner stone of orthodontic therapy in BMP patients [4,12,14,15,17], it is imperative for clinicians to know the effects of these therapies on the pharyngeal airway. The knowledge about this would be critical especially while managing class I BMP patients with preexisting pharyngeal airway compromise such as obstructive sleep apnea, dolichocephalic facial pattern and obesity [29,32].
Conclusion
Based on this study, a statistically significant reduction in soft palate thickness (0.35 mm), superior (0.69 mm), and middle (0.66 mm) airway spaces is evident following first premolar extraction and orthodontic retraction of anterior teeth among class I BMP patients. Furthermore, regression analysis showed that, for every 1° of lower incisor retroclination, a 0.73 mm change in tongue length was evidenced. The results of the present study need to be considered in light of the population studied, the difference in number of male to female samples and the twodimensional imaging technique used for analysis of PAS. Further studies utilizing advanced threedimensional modalities that could accurately assess the changes in different levels of the pharynx in a similar population would be promising. In addition to comprehensive pretreatment evaluation of the soft palate and tongue, the use of skeletal anchorage without premolar extractions may be considered in BMP patients, owing to their significant effects on the airway.
Conflict of Interest
All the authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Acknowledgment
The authors extend their appreciation to the Deanship of Scientific Research at King Saud University for funding this work through Research Group no. RG-1439-54.
References
- Kannan A, Sathyanarayana HP, Padmanabhan S. Effect of functional appliances on the airway dimensions in patients with skeletal class II malocclusion: A systematic review. J Orthod Sci 2017; 6:54-64.
- Park JE, Bae SH, Choi YJ, et al. The structural changes of pharyngeal airway contributing to snoring after orthognathic surgery in skeletal class III patients. Maxillofac Plast Reconstr Surg 2017; 39:22-26.
- Shokri A, Miresmaeili A, Ahmadi A, et al. Comparison of pharyngeal airway volume in different skeletal facial patterns using cone beam computed tomography. J Clin Exp Dent 2018; 10:1017-1028.
- Nuvusetty B, Peddu R, Prakash A, et al. Assessment of changes in pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary dentoalveolar protrusion. J Indian Orthod Soc 2016; 50:215-218.
- Zheng DH, Wang XX, Ma D, et al. Upper airway asymmetry in skeletal class III malocclusions with mandibular deviation. Sci Rep 2017; 7:1-14.
- Rojas E, Corvalan R, Messen E, et al. Upper airway assessment in orthodontics: A review. Odontoestomatologia 2017; 19:1-19.
- Maurya MRK, Kumar CP, Sharma LCM, et al. Cephalometric appraisal of the effects of orthodontic treatment on total airway dimensions in adolescents. J Oral Biol Craniofac Res 2019; 9:51-56.
- Germec-Cakan D, Taner T, Akan S. Uvulo-glossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. Eur J Orthod 2011; 33:515-520.
- Sharma K, Shrivastav S, Sharma N, et al. Effects of first premolar extraction on airway dimensions in young adolescents: A retrospective cephalometric appraisal. Contemp Clin Dent 2014; 5:190-194.
- Entrenas I, González-Chamorro E, Álvarez-Abad C, et al. Evaluation of changes in the upper airway after twin block treatment in patients with Class II malocclusion. Clin Exp Dent Res 2019; 5:259-68.
- deBerry-Borowiecki B, Kukwa A, Blanks RH. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope 1988; 98:226-34.
- Wang Q, Jia P, Anderson NK, et al. Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary protrusion. Angle Orthod 2012; 82:115-21.
- Hori K, Taniguchi H, Hayashi H, et al. Role of tongue pressure production in oropharyngeal swallow biomechanics. Physiol Rep 2013; 1:167.
- Al Maaitah E, El Said N, Abu Alhaija ES. First premolar extraction effects on upper airway dimension in bimaxillary proclination patients. Angle Orthod 2012; 82:853-859.
- Solem RC, Marasco R, Guiterrez-Pulido L, et al. Three-dimensional soft-tissue and hard-tissue changes in the treatment of bimaxillary protrusion. Am J Orthod Dent Orthop 2013; 144:218-228.
- Trisnawaty N, Ioi H, Kitahara T, et al. Effects of extraction of four premolars on vermilion height and lip area in patients with bimaxillary protrusion. Eur J Orthod 2013; 35:521-528.
- Yasutomi H, Ioi H, Nakata S, et al. Effects of retraction of anterior teeth on horizontal and vertical lip positions in Japanese adults with the bimaxillary dentoalveolar protrusion. Orthod Waves 2006; 65:141-147.
- Aldrees AM, Shamlan MA. Morphological features of bimaxillary protrusion in Saudis. Saudi Med J 2010; 31:512-519.
- Bhatia S, Jayan B, Chopra SS. Effect of retraction of anterior teeth on pharyngeal airway and hyoid bone position in Class I bimaxillary dentoalveolar protrusion. Medl J Armed Forces India 2016; 72:17-23.
- Jacobs JD. Vertical lip changes from maxillary incisor retraction. Am Orthod 1978; 74:396-404.
- Aloufi F, Preston CB, Zawawi KH. Changes in the upper and lower pharyngeal airway spaces associated with rapid maxillary expansion. ISRN Dent 2012; 2012:290964.
- Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod 2008; 78:209-214.
- Turnbull NR, Battagel JM. The effects of orthognathic surgery on pharyngeal airway dimensions and quality of sleep. J Orthod 2000; 27:235-247.
- Maetevorakul S, Viteporn S. Factors influencing soft tissue profile changes following orthodontic treatment in patients with class II division 1 malocclusion. Progress Orthod 2016; 17:13.
- Valiathan M, El H, Hans MG, et al. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod 2010; 80:1068-1074.
- Kikuchi M. Orthodontic treatment in children to prevent sleep-disordered breathing in adulthood. Sleep Breath 2005; 9:146-158.
- Tong H, Chen D, Xu L, et al. The effect of premolar extractions on tooth size discrepancies. Angle Orthod 2004; 74:508-511.
- Coşkun I, Kaya B. Cone beam computed tomography in orthodontics. Turk J Orthod 2018; 31:55-61.
- Flores-Blancas AP, Carruitero MJ, Flores-Mir C. Comparison of airway dimensions in skeletal Class I malocclusion subjects with different vertical facial patterns. Dental Press J Orthod 2017; 22:35-42.
- Obelenis Ryan DP, Bianchi J, Ignácio J, et al. Cone-beam computed tomography airway measurements: Can we trust them? Am Orthod Dento Ortho 2019; 156:53-60.
- Feng X, Li G, Qu Z, et al. Comparative analysis of upper airway volume with lateral cephalograms and cone-beam computed tomography. Am J Orthod Dento Orthop 2015; 147:197-204.
- Togeiro SM, Chaves CM, Palombini L, et al. Evaluation of the upper airway in obstructive sleep apnoea. Indian J Med Res 2010; 131:230-5.
Author Info
Alqahtani Nasser1*, Rana Alshammari2, Thikriat Al-Jewair3, Mohammad Aldosari1 and Albarakati Sahar1
1Pediatric Dentistry and Orthodontics Department, College of Dentistry, Riyadh, Saudi Arabia2Preventive Dentistry Department, College of Dentistry, University of Hail, Hail, Saudi Arabia
3Department of Orthodontics and Dentofacial Orthopedics, University of Missouri, Kansas City, USA
Citation: Alqahtani Nasser, Rana Alshammari, Thikriat Al-Jewair, Mohammad Aldosari, Albarakati Sahar, Post-orthodontic Pharyngeal Airway Changes Following First Premolar Extraction and Incisor Retraction in Bimaxillary Protrusion Patients–A Retrospective Study, J Res Med Dent Sci, 2019, 7(5):29-37
Received: 29-Aug-2019 Accepted: 16-Sep-2019
