Research Article - (2025) Volume 13, Issue 3
Prediction of Intraoperative Difficulties in Patients Undergoing Laparoscopic Vertical Sleeve Gastrectomy
Anees Faisal Obaid1* and Hayder AL-Zobaidy2
*Correspondence: Anees Faisal Obaid, Department of Medical Science, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq, Email:
Abstract
Background: The laparoscopic vertical sleeve gastrectomy is a safe and effective treatment that may improve quality of life and reduce morbidity and mortality associated with morbid obesity.
Materials and methods: A cross sectional study was conducted in the third unit of the surgical department of Baghdad teaching hospital and a private hospital from (the 2nd of November 2019 to the 30th of January of 2020), a hundred patients who wished to do LVSG for their morbid obesity were involved in this study, four factors was measured for these patients including gender, BMI, WHR and liver span by ultrasound.
The duration of the surgery was calculated for each patient starting from the insertion of the first port till the firing of the last endo GIA cartridge.
Results: There were no significant differences in the mean duration of surgery in relation to BMI (p=0.178), also the mean operation time had no significant difference with different gender (p=0.244). The mean operation time in patients with liver span ≤ 16 cm was lower than the mean operation time in patients with liver span>16 cm groups (p=0.0001). Also, the mean operation time in patients with peripherally obese was lower than the mean operation time in patients with centrally obese (p=0.0001).
Conclusion: Factors such as liver size and central obesity might lead to difficulties during LVSG whereas factors such as gender and BMI show no possible relation to difficulty.
Keywords
Intraoperative, Laparoscopic, Sleeve gastrectomy, Difficulties
Introduction
Obesity is described as excessive fat accumulation that may harm health. Obesity and overweight are caused by an energy imbalance between intake and output [1]. Obesity is rising alarmingly in many regions of the globe. A third of the world's population is fat [2]. Epidemiologic research has linked high BMI to an increasing number of chronic illnesses, including cardiovascular disease, diabetes, chronic renal disease, several malignancies and musculoskeletal problems [3].
The BMI is the most often used indicator of body fat. Bodyweight in kilograms divided by body height in meters squared. Although the BMI does not directly measure body fat, it has been determined to be a reliable indication due to its strong correlation [3].
WHR was calculated by dividing WC (in cm) by hip circumference (cm). Hip circumference was taken at the maximum circumference of the buttocks, parallel to the floor [4]. Accurate liver measurement improves surgical planning. An enlarged liver is defined as one that measures above 16 cm in the mid clavicular line. In addition to laparoscopic adjustable gastric banding, Roux-en- Y gastric bypass, vertical sleeve gastrectomy and biliopancreatic diversion are viable treatments for obesity. Overweight and obese patients benefit from surgery, which reduces mortality and improves obesity related disorders [5].
Bariatric surgery led to effective weight reduction in severely obese people. Diabetes, hyperlipidaemia, hypertension and obstructive sleep apnea were completely resolved or improved [6].
Sleeve gastrectomy: As a stand-alone treatment, gastric sleeve resection was originally intended to be the first stage in the biliopancreatic diversion with a duodenal switch [7].
Sleeve Gastrectomy (SG) is a bariatric operation that restricts food intake. Laparoscopic surgery removes 34% of the stomach. Surgeons consider it a stand-alone surgery, the first component of a two part approach for super obese patients with high BMI. The SG has fewer difficulties than the gastric bypass and Biliopancreatic Diversion (BPD) and allows for considerable weight reduction. SGs may be changed to gastric bypasses or BPDs in individuals with high BMIs and insufficient weight reduction (after weight loss has occurred). If weight reduction was adequate, no more procedures would be required [8].
Weight loss causes by the sleeve: It is a physiological technique that cannot be classified as simply restrictive surgery because it produces significant changes in the production of hormones, particularly ghrelin, PYY and GLP-1 [9].
LSG's ability to cause weight reduction is thought to be attributable to two key processes. First, as a restrictive surgery, it restricts food intake and stomach distension. Second, hormonal pathways may be implicated. This is linked to lower circulating ghrelin levels after gastric fundus excision. Decreased ghrelin levels may also cause post meal satiety [10].
Expected weight loss: Weight loss following SG varies according to the population investigated. SG employed this surgery to downstage high risk medical patients. SG alone may help most people reduce 40-60% of their extra body weight in a year [11].
Complications of surgery: Complications of SG include bleeding, stenosis, portal thrombosis, and leak. The most feared consequence is an oesophagogastric staple line leak that is difficult to avoid [12].
Materials and Methods
The data collection was carried out at the 3rd surgical unit/department of surgery in Baghdad teaching hospital and a private hospital, between the (2nd of November 2019 to the 30th of January of 2020).
Study sample: A convenient sample of patients with morbid obesity who were submitted for LVSG as a definitive bariatric procedure.
Inclusion criteria:
• Body Mass Index (BMI)>40 kg/m2 or BMI 35-39.9
kg/m2 with a serious comorbid disease treatable by
weight loss.
• Minimum of 5 years of obesity.
• Failure of conservative treatment.
• Acceptable operative risk on preoperative assessment.
Exclusion criteria: Patients with previous bariatric surgery and patients with previous upper abdominal surgery.
Surgical technique: The patient lies supine, with the surgeon standing on the patient's right side. A 5 mm port is inserted in the epigastric region just below the xiphoid process, followed by a 10 mm port above and to the left of the optical port, and a 12 mm port at the right mid clavicular line. Insufflation CO2 pressure was 10-15 mmHg.
Mobilization of the larger omentum from the greater curvature of the stomach to the left crus using a 5 mm Maryland jaw ligature.
Using a 60 mm Endo GIA device (gastrointestinal anastomosis) stapler, a sleeve is formed beginning 5 cm from the pylorus up to the angle of his.
The specimen was withdrawn using the 10 mm port, and no over stitching over the stapler line was done.
The 10 mm corrugated drain is introduced below the stapler line, deflating the peritoneal cavity and closing the ports.
Statistical analysis: Data were analyzed using a statistical package for the social sciences (SPSS version 23) computer software program.
Descriptive statistics are presented as frequency tables. Chi-square fisher exact test was used to find an association between two categorical variables with a significant level of ≤ 0.05.
Results
A total of 100 patients with morbid obesity were enrolled in this study, all patients underwent sleeve surgery. The mean age of patients was 32.7 years ranging between 17-63 years. Females represent 61% of patients and 39% of patients were male (Table 1).
| Variable | Percentage | |
|---|---|---|
| Age | Less than 30 years | 43% |
| Between 30-39 years | 34% | |
| More than and equal to 40 years | 23% | |
| Gender | Female | 61% |
| Male | 39% | |
Table 1: Age and gender distribution of studied patients.
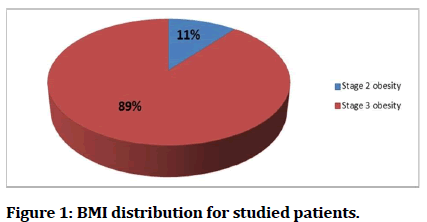
The mean Body Mass Index (BMI) was 46.7 Kg/m2, the percentage of patients with class II obesity (BMI between 35-39.9 Kg/m2) was 11% and the percentage of patients with class III obesity (BMI ≥ 40 Kg/m2) was 89% (Figure 1).
Figure 1: BMI distribution for studied patients.
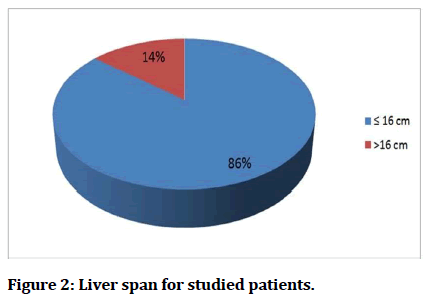
Regarding the liver span, the mean liver span was 15.5 cm, ranging between 14.4 cm to 18 cm and the percentage of patients below or equal to 16 cm was 86% while only 14% of patients had a liver span more than 16 cm (Figure 2).
Figure 2: Figure 1: Liver span for studied patients.
Regarding fat distribution pattern, 78% of patients were peripherally obese while 22% of patients were centrally obese (Table 2).
| Fat distribution pattern | Percentage |
|---|---|
| Peripherally obese | 78% |
| Centrally obese | 22% |
Table 2: Fat distribution pattern for studied patients.
The mean operation time had no significant difference with different age groups and different gender (p=0.124, 0.244 respectively) (Table 3).
| Variable | Mean operation time (± SD) | P value | |
|---|---|---|---|
| Age | <30 years | 748.5 (± 173) sec | 0.124* |
| 30-39 years | 688.3 (± 97) sec | ||
| ≥ 40 years | 764 (± 180) sec | ||
| Gender | Female | 746 (± 164) sec | 0.244** |
| Male | 709 (± 139) sec | ||
| *ANOVA test, **student T test, significant ≤ 0.05. | |||
Table 3: Relation of operation time with different age and gender groups.
Although the mean operation time for patients with stage 2 obesity was shorter than for those with stage 3, the mean duration did not vary between the two groups (p=0.178). The mean surgery time was shorter in patients with a liver spread of 16 cm or less than the mean operation time in patients with a liver span of 16 cm or more (p=0.0001). Also, the mean operation time for patients with peripheral obesity was shorter than for patients with central obesity and the difference was statistically significant (p=0.0001) (Table 4).
| Variables | Mean operation time (± SD) | P value | |
|---|---|---|---|
| Stage of obesity | Stage 2 | 673.1 (± 37) sec | 0.178** |
| Stage 3 | 739 (± 162) sec | ||
| Liver span | ≤ 16 cm | 681.6 (± 95) sec | 0.0001** |
| >16 cm | 1039.6 (± 75) sec | ||
| Fat distribution pattern | Peripherally obese | 658.3 (± 38) sec | 0.0001** |
| Centrally obese | 992 (± 132) sec | ||
| **Student T test, significant ≤0.05. | |||
Discussion
The relationship of variables to surgery length offered us a hint regarding their probable rule as a predictor of surgery difficulties. The patients in this research varied in age from 17 to 63 years, with a mean age of 32.7 years, and a 61 percent female preponderance.
Similar findings were obtained by Stroh C, Weiner R, et al. in Germany 2014, in which no gender specific variations were detected in terms of access method, and clinically irrelevant was the greater operation time for male patients [13].
Although 89 percent of patients had stage 3 obesity (BMI 40 Kg/m2), the remaining 11% had stage 2 obesity (BMI 35-39.9 Kg/m2), the difference in mean surgery length was not statistically significant (p=0.178), indicating that BMI had no influence on surgery duration or intraoperative difficulties.
In this research, the Waist to Hip Ratio (WHR) revealed that 22% of patients were centrally obese whereas 78% were peripherally obese.
This was mostly due to difficulty in port insertion especially the introduction of the optical port, as well as large and vascular omentum that was rather bothersome to handle.
By ultrasonography, only 14% of patients had a liver spread of more than 16 cm, while the remaining 85% had a liver span within the typical range.
The operation took longer in individuals with a liver size of 16 cm or more than in those with an average liver size, indicating that the former group had greater difficulties.
The additional time in patients with big livers was attributable to problems retracting the liver during mobilization of the stomach and construction of the stomach sleeve. The ports, omentum, spleen, liver, and staple line did not bleed.
Conclusion
There were no significant differences in the mean duration of surgery in relation to BMI (p=0.178), also the mean operation time had no significant difference with different gender (p=0.244). The mean operation time in patients with liver span ≤ 16 cm was lower than the mean operation time in patients with liver span>16 cm groups (p=0.0001). Also, the mean operation time in patients with peripherally obese was lower than the mean operation time in patients with centrally obese (p=0.0001). Several factors might affect the difficulty of sleeve gastrectomy including the liver size and fat distribution pattern, these factors should be evaluated and whenever possible corrected prior to surgery.
References
- World Health Organization (WHO). Obesity and overweight. Fact sheet No. 311. Updated March 2013.
- Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab 2015; 66:7-12.
[Crossref] [Google Scholar] [PubMed]
- Afshin A, Forouzanfar MH, Reitsma MB, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017; 377:13-27.
[Crossref] [Google Scholar] [PubMed]
- Ahmad N, Adam SI, Nawi AM, et al. Abdominal obesity indicators: Waist circumference or waist to hip ratio in Malaysian adults population. Int J Prev Med 2016; 7.
[Crossref] [Google Scholar] [PubMed]
- Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003-2012. JAMA Surg 2014; 149:275-287.
[Crossref] [Google Scholar] [PubMed]
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: A systematic review and meta-analysis. JAMA 2004; 292:1724-1737.
[Crossref] [Google Scholar] [PubMed]
- Felberbauer FX, Langer F, Shakeri Manesch S, et al. Laparoscopic sleeve gastrectomy as an isolated bariatric procedure: Intermediate term results from a large series in three austrian centers. Obesity Surg 2008; 7:814-818.
- Karmali, Shahzeer, et al. "Laparoscopic sleeve gastrectomy: An innovative new tool in the battle against the obesity epidemic in Canada Can J Surg 2010; 53:126-132.
[Google Scholar] [PubMed]
- Nassar R. Laparoscopic sleeve gastrectomy. Revista Colombiana de Gastroenterologia 2011; 26:265-268.
- Gill RS, Lai M, Birch DW, et al. Sleeve gastrectomy: Procedure, outcomes and complications. Curr Obes Reports 2012; 1:75-79.
- Arias E, Martinez PR, Li VK, et al. Mid-term follow up after sleeve gastrectomy as a final approach for morbid obesity. Obes Surg 2009; 19:544-548.
[Crossref] [Google Scholar] [PubMed]
- Iannelli A, Treacy P, Sebastianelli L, et al. Perioperative complications of sleeve gastrectomy: Review of the literature. J Minim Access Surg 2019; 15:1-7.
[Crossref] [Google Scholar] [PubMed]
- Stroh C, Weiner R, Wolff S, et al. Are there gender specific aspects in obesity and metabolic surgery? Data analysis from the german bariatric surgery registry. Viszeralmedizin. 2014; 30:125-132.
Author Info
Anees Faisal Obaid1* and Hayder AL-Zobaidy2
1Department of Medical Science, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq2Department of Surgery, College of Medicine, Baghdad University, Baghdad, Iraq
Citation: Anees Faisal Obaid, Hayder AL-Zobaidy, Prediction of Intraoperative Difficulties in Patients Undergoing Laparoscopic Vertical Sleeve Gastrectomy, J Res Med Dent Sci, 2022, 11 (06): 011-014.
Received: 05-May-2022, Manuscript No. JRMDS-22-62940; , Pre QC No. JRMDS-22-62940; Editor assigned: 09-May-2022, Pre QC No. JRMDS-22-62940; Reviewed: 24-May-2022, QC No. JRMDS-22-62940; Revised: 29-May-2023, Manuscript No. JRMDS-22-62940; Published: 07-Jun-2023