Research - (2022) Volume 10, Issue 1
Prevalence and Complications of Inflammatory Bowel Disease among Saudi Population: A Cross-Sectional Study
Masoud Ahmad Al-Ghamdi1, Manal Abdulaziz Murad2, Reem Mohammed Alshiakh3, Hoda Jehad Abousada4*, Mohammed Bandar Alharbi5, Rawiah Abubkr Almehdhar5, Turki Saad Aljuhani5, Abdullah Mohammed H Alsobyei5, Abdulrahman Hussain Alharbi6, Ghanem Ahmed AL Ghanem6, Saud Ali Alharbi6, Abdulaziz Shelash Alonezi6, Rashed Saleh A Alghamdi6, Razan Talal Almowllad7 and Fatimah Mohammed Alfaqih7
*Correspondence: Hoda Jehad Abousada, Department of Obestetric and Gynecology, KAMC, Jeddah, KSA, Email:
Abstract
Background: Inflammatory bowel disease (IBD) comprises a group of diseases that affect the digestive system and, due to wave-like inflammation, lead to long-term complaints in the gastrointestinal tract, such as diarrhoea with blood or mucus in the stool, abdominal pain and symptoms from other organ systems. This inflammation is due to an excessive reaction of the immune system to the body's own germs or cells that are normally in the intestine. The trigger for this reaction remains unclear, despite intensive research, and is most likely multifactorial. So far there is no definitive therapy. There are a number of drugs available that primarily suppress inflammation and prevent complications from developing. In severe cases, surgical interventions are also an option. The two basic diseases that together make up about 90% of inflammatory bowel disease cases are: Ulcerative colitis and Crohn's Disease. Methods: This was an analytical cross-sectional study to spot light on the prevalence and complications of IBD among Saudi Population. The study was carried out at universities, hospitals and malls in KSA. Data were collected from IBD patients and general population during a period from June to October 2021. Results: Among the 776 participants, 490 were females (63.1%) and the rest are males. Regarding the age group, most of the participants were from 18-24 years (n=247, 31.8%). From the participants, 138 were smoking; at the time of data collection, (17.8%) and 40 were ex-smokers (5.2%). About (n=84, 10.8%) from the participants were diagnosed with IBD; 31% of them have Crohn's disease, and 69% have Ulcerative colitis. The peak age group for Crohn’s disease was 35-44 years while for ulcerative colitis was 25-34. For symptoms of IBD, the change in appetite is more significant among females while mouth or stomach ulcers is more significant for older age groups; and weight loss is significant for both females and older age groups. Osteoporosis is more significant for females while perforation and B 12 malabsorption is more significant among older age groups. Conclusion: The prevalence of IBD among the selected group of patients was relatively low. It was noticed that the patients with Ulcerative colitis were younger than patients with Crohn's disease; with overall female predominance for both Ulcerative colitis and Crohn's disease. The selected patients were suffering from many symptoms; the most common symptoms were joint manifestations, eye manifestations, and abdominal pain.
Keywords
Crohn's disease, Inflammatory bowel disease, Diarrhoea, Ulcerative colitis, Malabsorption
Introduction
The term inflammatory bowel disease is used to combine Crohn's disease and ulcerative colitis. Common symptoms include diarrhoea, blood loss from the intestines, and abdominal pain. Usually, however, the two diseases can be differentiated. The clinical pictures run in batches. The cause is a "dysregulation" of the mucosal immune system [1]. This is now seen as an adequate response to bacterial invasion when the chemical mucosal barrier is defective. Inflammatory bowel diseases occur more frequently in industrialized countries with a high standard of living. There is a familial accumulation. Smoking plays a role (especially in Crohn's disease. The age profile is broad when ulcerative colitis is first diagnosed and peaks in the third to fourth decade of life. Crohn's disease is found primarily in 15 to 34 years old [2]. Women and men are affected in roughly equal proportions. There are many common characteristics and significant overlap between the two diseases, but also important differences. In around 10% of cases, however, despite extensive diagnostic measures, it is not possible to differentiate between the two. In these cases, one speaks of "colitis indeterminata" [3].
An exact cause has not yet been identified. In part, it is an excessive activation of the immune system by the microorganisms that normally live in the intestine (the microbiome) and do not trigger an immune reaction in healthy people [4]. This activation leads to the collection of immune cells in the wall of the gastrointestinal tract and the excretion of messenger substances, which further intensify this reaction. The result is severe inflammation, which initially irritates the intestine with increased diarrhoea and over time can damage the intestinal wall and mucous membrane with bleeding, ulcers and scars or even rupture the wall. The course is almost always wavy, with relapses (acute deterioration) alternating with remissions (improvement of symptoms).
In addition, other organs and systems are sometimes affected by this immune activity. The skin, eyes and joints are most commonly affected. However, what triggers the initial activation of the immune system remains unclear [5]. It is most likely a combination of genetic predisposition, environmental factors (e.g., nutrients), and impaired interaction between the microbiome and immune cells.
With typical complaints and findings in the clinical examination, the suspicion of a chronic inflammatory bowel disease arises. Laboratory findings, such as increased markers of inflammation in the blood or in the stool, can support this assumption. For a definitive diagnosis, however, a direct assessment of the mucous membrane of the intestine and stomach with an endoscopy (colonoscopy or gastroscopy) and removal of tissue samples is necessary. Either imaging techniques (e.g. magnetic resonance imaging) or endoscopic methods (capsule endoscopy, double balloon enteroscopy) can be used to evaluate the small intestine in Crohn's disease [6].
On the basis of international guidelines and the needs of each patient, a personalized therapy plan is created and adjusted depending on the course of the disease. Except for the classification of drug therapy, we also carry out endoscopic therapies (e.g., expansion of constrictions) if necessary [7]. The patients who may need surgical therapy are cared for and treated by gastroenterologists as part of interdisciplinary team together with visceral surgery.
Literature Review
Crohn's disease is a chronic inflammatory bowel disease that can affect the entire gastrointestinal tract. This means that the inflammation and the associated symptoms can extend from the mouth to the rectum. In the event of an attack from Cohn's disease, several widely spaced segments of the gastrointestinal tract can become inflamed at the same time. Most often, however, the last part of the small intestine (terminal ileum) before the transition into the large intestine is affected [8]. Another important characteristic of Crohn's disease is that, unlike ulcerative colitis, the inflammation affects all layers of the wall. As a result, the inflammation can spread more quickly to adjacent structures and cause accumulations of pus (abscesses) or connections between the inflamed intestine and other organs (fistulas), e.g., the urinary bladder, the uterus or the skin, which complicate the course and the therapy [9].
The most common symptoms of Crohn's disease (as with ulcerative colitis) are an increased frequency of bowel movements (a few to several tens of times per day) with liquid stool and mostly blood and mucus. Along with the diarrhoea, there are usually cramp-like abdominal pain, which may be aggravated after eating and partially alleviated after a bowel movement. Due to the inflammatory condition, fever, mostly flare-ups, is also common. Crohn's disease can affect the small intestine and stomach, nausea or vomiting are sometimes also part of the clinical picture [10]. The combination of blood loss in the intestine and poor iron and vitamin absorption in the small intestine can lead to anemia with general tiredness and shortness of breath. In the medium or long term, there may also be deterioration in nutritional status and weight loss. In severe cases, the scarring of the intestinal wall can cause an intestinal obstruction (congestion of the intestinal contents) or an expansion of a loop of intestine, which in rare cases can lead to rupture of the intestinal wall and peritonitis. In Crohn's disease, as in ulcerative colitis, inflammation can occur in other parts of the body. These include painful reddening of the skin (erythema nodosum), purulent necrosis (pyoderma gangrenosum) or inflammation of the joints or eyes. These symptoms outside the intestine can sometimes occur years before, at the same time or after the symptoms of the gastrointestinal tract [11].
Selections of drugs that inhibit the activation of the immune system are available today. The choice of the right drug depends on the location of the inflammation in the gastrointestinal tract and the severity [12]. The main categories are as follows: 1: Aminosalicylic acid products (e.g., mesalazine): These drugs are less effective for Crohn's disease than for ulcerative colitis. They can be used for prevention both in relapse and in remission. They are available in the form of tablets, enema, or suppositories. They are hardly absorbed from the intestine into the circulation and therefore have few systemic side effects. 2: Corticosteroids: They can be given in tablet form or intravenously. The corticosteroids are powerful anti-inflammatory drugs, but are mainly used for a limited time during an episode because of their significant side effects. 3: Immune modulators: This is what drugs are called which suppress the immune system and thus also the inflammatory reaction in the intestine. The main drugs in this class are azathioprine and 6-mercaptopurine. Methotrexate is also used, although less often than the other two. 4: Biologicals: This category includes modified artificial antibodies that inhibit the action of molecules that are very important for the activation of the immune system. The drugs belonging to this are very potent and can also be effective in patients who do not respond to the other categories.
Surgical therapy is used in Crohn's disease primarily in the event of complications, with the aim of securing the intestinal passage (e.g., in the case of scarred constrictions), locally removing the abscesses and closing the fistulas, as well as an intestinal rupture to be avoided (with greatly enlarged intestinal loops) [13].
Patients with Crohn's disease are at a much higher risk of developing colon cancer as their disease progresses. For this reason, these patients, even if they do not have any subjective symptoms, must be included in a monitoring program and examined with regular colonoscopies. The intervals between the colonoscopies depend on the location of the inflammation, but in most cases, according to current guidelines, one colonoscopy is 8 years after the initial diagnosis and every 1 to 2 years thereafter [14].
On the other hand, Ulcerative colitis is a chronic inflammatory disease of the large intestine that usually runs in episodes. Most of the time, the inflammation starts in the rectum and can spread to the entire colon [15]. Inflammatory ulcers that bleed easily can be found in the superficial layer of the lining of the large intestine.
Regarding the differences between ulcerative colitis and Crohn's disease: First of all, in ulcerative colitis only the large intestine can be affected, in contrast to Crohn's disease, where the inflammation can spread throughout the digestive system. Second, the distribution of inflammation in ulcerative colitis is continuous. An infestation of different intestinal segments that are distant from one another is not the case here. In most cases, the inflammation begins in the rectum and can spread towards the appendix. Thirdly, ulcerative colitis does not affect all layers of the intestinal wall, only the mucous membrane (innermost layer) [16].
Similar to Crohn's disease, the symptoms of ulcerative colitis range from attacks of bloody and slimy diarrhoea with or without fever, abdominal cramps, anemia caused by the loss of blood, and complaints in other parts of the body (mainly skin, eyes and joints) [17]. It is seldom possible to distinguish between the two diseases only on the basis of the symptoms. Since the small intestine is not affected in ulcerative colitis, there is not so often a reduced absorption of nutrients. Connections between the intestine and other organs (urinary bladder, skin, uterus) as well as accumulations of pus next to the intestine are also much rarer here, because the inflammation does not affect the entire wall thickness, but only the mucous membrane.
The therapy for ulcerative colitis is based on the same drugs as for Crohn's disease. However, the different localization of the inflammation also has a major influence here [18]. Since the inflammation is only in the large intestine and is more superficial (mucous membrane), locally effective drugs (such as Aminosalicylic acid products and locally effective steroids) are of much greater importance and are the first choice for most patients. Similar to Crohn's disease, the corticosteroids are used briefly to control a relapse if the locally effective therapies are insufficient. The other immunomodulatory and biologics are used in patients who do not respond to local therapies.
Surgical therapy is used in case of complications. Surgery can remove severely dilated loops of intestine to avoid the risk of rupture. In ulcerative colitis, however, surgical therapy can be evaluated as a basic therapy in very severe cases (not responding to any other therapy). With the intention of curing the disease, the inflamed part or the whole of the large intestine can be removed (colectomy) [19]. However, the disease can sometimes become active again in the remaining parts.
Possible complications of ulcerative colitis are diverse and sometimes life-threatening. It can lead to heavy to massive bleeding, this occurs with increasing spread of ulcerative colitis. Another complication of a severe flareup is a toxic mega colon (that is, the transverse colon is enlarged by more than 5-6 cm), often accompanied by an ileus. The abdomen is then swollen and a perforation can follow [20]. The latter can also occur independently of a toxic mega colon. Scarred constrictions (strictures) rarely occur in ulcerative colitis, in contrast to Crohn's disease. Patients with long-standing and extensive ulcerative colitis have an increased risk of developing colon cancer; these tumors can also be concealed in the strictures mentioned.
Regarding the complications of Crohn's disease; they include: Bleeding (less common than ulcerative colitis), fissures, and fistulas (predominantly in the perianal region, >54%), abscesses, strictures and obstructions (most often located in the ileocecal region, that is, at the transition from the small to the large intestine.) and rarely also toxic mega colon, perforations, colon cancer and other tumorous neoplasms [14].
Methods
Study design
This was an analytical cross-sectional study to spot light on the prevalence and complications of IBD among Saudi Population.
Study setting
The study was carried out at universities, hospitals and malls in KSA. Data were collected from general population during a period from June to October 2021.
Sampling and sample
Participants were chosen via probability simple random sampling technique. Participants were selected from the general population and IBD patients. The final number of sample size was 500 participants. However, the study included 776 participants.
Inclusion criteria
General population, IBD patients.
Exclusion criteria
None.
Instruments
Data collection tool was self-designed and base on latest literature. It contained the following information: (1) Sociodemographic characteristics: age, gender, and (2) Disease related information: Smoking, DM, Symptoms and complications.
Statistical analysis
Data was entered and analyzed via SPSS version 23, descriptive statistics were performed and categorical data was displayed as frequencies and percentages while measures of patients with IBD and measures complications were used to summarize continuous variables.
Univariate and multivariate analysis was performed to investigate association between age, gender, and most common symptoms and complications. Statistical significance is set at a P value of 0.05 or less.
Permission and ethical considerations
Administrative approval will be sought from the unit of biomedical ethics research committee Ethical approval was sought from the ethical committee of the faculty of medicine, King Abdul-Aziz university. An informed consent was sought from the participants.
Results
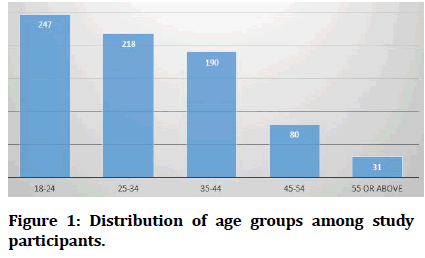
This study aimed to spot light on inflammatory bowel disease among Saudi population. The study included 776 participants. Among them, there were 490 female (63.1%) and the rest were males. The most prevalent age group among study participants was 18-24 years of age (n= 247, 31.8%). Figure 1 shows the distribution of age groups among study participants.
Figure 1: Distribution of age groups among study participants.
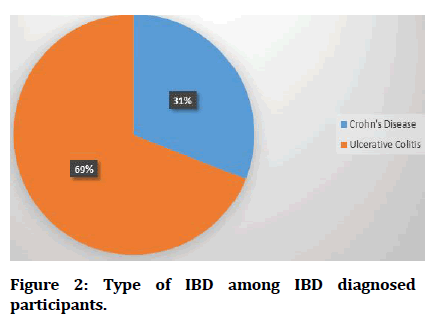
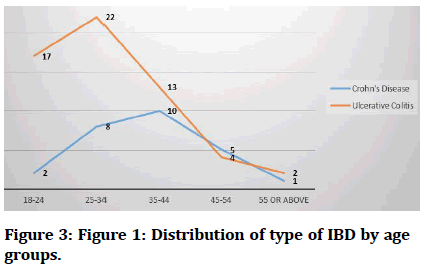
On asking participants about their smoking status, there were 138 participants who are currently smoking (17.8%) and 40 participants who were ex-smokers (5.2%). There were very little proportion of participants had diabetes mellitus (n=61, 7.9%). This was the same for the proportion of participants who are being diagnosed having inflammatory bowel disease (n= 84, 10.8%). On further asking these patients about which IBD they have, their responses are presented in Figure 2. The distribution of IBD disease by gender is presented in Table 1. The peak age group for Crohn’s disease was 35-44 years while for ulcerative colitis was 25-34. Figure 3 shows the distribution of IBD by age groups. Symptoms of inflammatory bowel disease varied among participants. They presented with some painful symptoms and others. Table 2 demonstrates the frequency of symptoms of participants.
Figure 2: Type of IBD among IBD diagnosed participants.
Figure 3:Distribution of type of IBD by age groups.
| IBD | Male | Female |
| Crohn’s disease | 12 | 14 |
| Ulcerative colitis | 18 | 40 |
Table 1: Distribution of IBD according to gender.
| Symptom or sign | Frequency | Percent | P value for gender | P value for age groups |
|---|---|---|---|---|
| Abdominal pain | 44 | 5.7 | - | - |
| Change in menstrual cycle | 2 | 0.3 | - | - |
| Fatigue | 10 | 1.3 | - | - |
| Change in appetite | 7 | 0.9 | 0.03 | - |
| Mouth or stomach ulcers | 5 | 0.6 | - | 0.01 |
| Diarrhea | 2 | 0.3 | - | - |
| Rectal bleeding | 4 | 0.5 | - | - |
| Weight loss | 5 | 0.6 | 0.001 | 0 |
| Fistula | 12 | 1.5 | - | - |
| Eye symptoms | 45 | 5.8 | - | - |
| Joint manifestations | 55 | 7.1 | - | - |
| Osteoporosis | 10 | 1.3 | 0 | - |
| Perforation | 5 | 0.6 | - | 0.001 |
| B 12 Malabsorption | 18 | 2.3 | - | 0.001 |
| Toxic mega colon | 6 | 0.8 | - | - |
| Colon cancer | 1 | 0.1 | - | - |
Table 2: Signs and symptoms of participants with statistically significant relationships.
It is noticed from the previous table that change in appetite is more significant among females while mouth or stomach ulcers are more significant for older age groups. Furthermore, weight loss is significant for both females and older age groups. Osteoporosis is more significant for females while perforation and B 12 malabsorption is more significant among older age groups. Ultimately, participants were asked if they had malnutrition or anemia. Their answers are drawn on 5 points Likert scale as presented in the following Table 3. Majority of participants didn’t answer the questions.
| Variable | Always | Often | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| Malnutrition | 6 | 15 | 33 | 21 | 9 |
| Anemia | 6 | 17 | 19 | 15 | 27 |
Table 3: Participant's perception of having anemia and malnutrition.
Discussion
Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory diseases affecting the gastrointestinal tract and are collectively known as inflammatory bowel diseases (IBDs) [21]. UC generally affects the large intestine and rectum, whereas CD can target any part of the gut [22]. Historical data have shown that the younger demographic is more susceptible to IBD, causing a significant alteration in their quality of life, alongside debilitating morbidity and exacerbations.
The etiology of IBD is not well-established; however, contemporary hypotheses implicate an interaction of environmental and immunoregulatory factors in genetically vulnerable individuals [23].
There are six studies reported the incidence and/or prevalence of IBD in the aforementioned countries. In the study reported by Al-Shamali et al. [24], a retrospective review of all patients presented with a confirmed diagnosis of UC in Kuwait City, a total of 346 patients were identified. The authors reported that the local incidence of UC was 2.8 per 100,000 persons per year. Another study from Kuwait reported that the incidence of pediatric IBD was 2.6 per 100,000 persons per year [25].
Al-Ghamdi et al. [26] retrieved the data of all confirmed cases with CD in a tertiary center in Riyadh, KSA, and estimated that the incidence of CD increased from 0.32 per 100,000 persons per year between 1983 and 1993 to 1.66 per 100,000 persons per year between 1994 and 2004 with a combined mean annual incidence of 0.94 per 100,000 persons per year over these 20 years. In another retrospective study from Bahrain, it was found that the average number of CD cases increased from 0.4 between the years 1984 and 2001 to 4 cases per year between 2002 and 2014. For UC, the average number of cases between 1984 and 2001 was 2, while this increased to 8 for the years 2002–2014. Overall, the prevalence of IBD was found to be 26.25 per 100,000 persons [27].
In the prospective study of IBD patients in Oman, it was reported that the incidence of UC was 1.35 per 100,000 persons per year [28]. Abdul-Baki et al. [29] collected data of IBD patients in Beirut and reported a mean annual incidence of 4.1 per 100,000 people for UC, 1.4 per 100,000 people for CD, and a total annual incidence of IBD of 5.5 per 100,000 people per year.
The mean age at diagnosis ranged from 24.13 to 43.6 years in adult cases and from 4.5 to 16 years in pediatric cases. In most of the included studies, the majority of patients were males (average 41–59%). The majority of patients in the included studies had no previous history of smoking. While the prevalence of family history ranged from 1.5 to 26.1%. Only 1 study from Saudi Arabia reported the consanguinity rate, which was 32.6%. Studies reported that hematochezia, diarrhoea, urgency, and tenesmus were the main presenting features of the patients. Concerning the time to diagnosis, studies in Saudi population reported that the average time to diagnosis was nearly 6 months in >90% of the patients with UC; while the study from Oman demonstrated that the average time to diagnosis was 13.2 months. The most common site of colon involvement among the included studies was the left colon. Concerning disease severity and extent, ulcerative proctitis accounted for 6.9–27.3% of the cases, while pan colitis accounted for 10–45% of the cases. The proportion of patients with pan colitis was notably higher among patients from Kuwait, Lebanon, and Saudi Arabia. The majority of patients had mild/ moderate severity of the disease. The protocol of IBD diagnosis was consistent across the included studies and composed mainly of endoscopy and biopsy. The extent of colon involvement was variable across the included studies [30-33].
The gender preponderance (higher number of males) observed among the IBD patients from Arab countries contrasts with studies of the adult IBD population, where there are a slightly greater proportion of females with IBD in studies from Iran [34] and Sri Lanka [35], while studies in Japan [36], Korea [37], and other Asian countries [38] have shown a similar incidence in males and females.
Conclusion
The prevalence of IBD among the selected group of patients was relatively low. It was noticed that the patients with Ulcerative colitis were younger than patients with Crohn's disease; with overall female predominance for both Ulcerative colitis and Crohn's disease. The selected patients were suffering from many symptoms; the most common symptoms were joint manifestations, eye manifestations, and abdominal pain.
References
- Bianco AM, Girardelli M, Tommasini A. Genetics of inflammatory bowel disease from multifactorial to monogenic forms. World J Gastroenterol 2015; 21:12296–310.
- Wallace KL, Zheng LB, Kanazawa Y, et al. Immunopathology of inflammatory bowel disease. World J Gastroenterol 2014; 20:6–21.
- http://accesspharmacy.mhmedical.com/content.aspx?aid=1120811070
- McDowell C, Farooq U, Haseeb M. Inflammatory bowel disease. In Treasure Island (FL) 2021.
- Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life 2019; 12:113–22.
- Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterol 2007; 133:1670–89.
- Taylor S, Lobo AJ. Diagnosis and treatment of inflammatory bowel disease. Practitioner 2016; 260:19–23.
- Feuerstein JD, Cheifetz AS. Crohn disease: Epidemiology, diagnosis, and management. Mayo Clin Proc 2017; 92:1088–103.
- Ha F, Khalil H. Crohn’s disease: A clinical update. Therap Adv Gastroenterol 2015; 8:352–9.
- Perler BK, Ungaro R, Baird G, et al. Presenting symptoms in inflammatory bowel disease: Descriptive analysis of a community-based inception cohort. BMC Gastroenterol 2019; 19:47.
- Nóbrega VG, Silva IN de N, Brito BS, et al. The onset of clinical manifestations in inflammatory bowel disease patients. Arq Gastroenterol 2018; 55:290–295.
- Wilkins T, Jarvis K, Patel J. Diagnosis and management of crohn’s disease. Am Fam Physician 2011; 84:1365–75.
- Shaffer VO, Wexner SD. Surgical management of Crohn’s disease. Langenbeck’s Arch Surg 2013; 398:13–27.
- Hsu YC, Wu TC, Lo YC, et al. Gastrointestinal complications and extraintestinal manifestations of inflammatory bowel disease in Taiwan: A population-based study. J Chin Med Assoc 2017; 80:56–62.
- Gajendran M, Loganathan P, Jimenez G, et al. A comprehensive review and update on ulcerative colitis. Dis Mon 2019; 65:100851.
- Roushan N, Ebrahimi Daryani N, Azizi Z, et al. Differentiation of Crohn’s disease and ulcerative colitis using intestinal wall thickness of the colon: A diagnostic accuracy study of endoscopic ultrasonography. Med J Islam Repub Iran 2019; 33:57.
- Ungaro R, Mehandru S, Allen PB, et al. Ulcerative colitis. Lancet 2017; 389:1756–70.
- Xu CT, Meng SY, Pan BR. Drug therapy for ulcerative colitis. World J Gastroenterol 2004; 10:2311–2317.
- Kayal M, Shah S. Ulcerative colitis: Current and emerging treatment strategies. J Clin Med 2019; 9.
- Manser CN, Borovicka J, Seibold F, et al. Risk factors for complications in patients with ulcerative colitis. United Eur Gastroenterol J 2016; 4:281–7.
- Esmat S, El Nady M, Elfekki M, et al. Epidemiological and clinical characteristics of inflammatory bowel diseases in Cairo, Egypt. World J Gastroenterol 2014; 20:814–21.
- Mosli M, Alzahrani A, Showlag S, et al. A cross-sectional survey of multi-generation inflammatory bowel disease consanguinity and its relationship with disease onset. Saudi J Gastroenterol 2017; 23:337–40.
- Siddique I, Alazmi W, Al-Ali J, et al. Clinical epidemiology of Crohn’s disease in Arabs based on the montreal classification. Inflamm Bowel Dis 2012; 18:1689–97.
- Al-Shamali MA, Kalaoui M, Patty I, et al. Ulcerative colitis in Kuwait: A review of 90 cases. Digestion 2003; 67:218–24.
- Al-Qabandi WA, Buhamrah EK, Hamadi KA, et al. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol 2011; 17:323–7.
- Al-Ghamdi AS, Al-Mofleh IA, Al-Rashed RS, et al. Epidemiology and outcome of crohn’s disease in a teaching hospital in Riyadh. World J Gastroenterol 2004; 10:1341–4.
- Abdulla M, Al Saeed M, Fardan RH, et al. Inflammatory bowel disease in Bahrain: Single-center experience. Clin Exp Gastroenterol 2017; 10:133–45.
- Radhakrishnan S, Zubaidi G, Daniel M, et al. Ulcerative colitis in Oman. A prospective study of the incidence and disease pattern from 1987 to 1994. Digestion 1997; 58:266–70.
- Abdul-Baki H, ElHajj I, El-Zahabi LMN, et al. Clinical epidemiology of inflammatory bowel disease in Lebanon. Inflamm Bowel Dis 2007; 13:475–80.
- Sharara AI, Al Awadhi S, Alharbi O, et al. Epidemiology, disease burden, and treatment challenges of ulcerative colitis in Africa and the Middle East. Expert Rev Gastroenterol Hepatol 2018; 12:883–97.
- Aljebreen AM, Alharbi OR, Azzam NA, et al. Clinical epidemiology and phenotypic characteristics of Crohn’s disease in the central region of Saudi Arabia. Saudi J Gastroenterol 2014; 20:162–169.
- El Mouzan M, Al-Mofarreh M, Assiri A, et al. Consanguinity and inflammatory bowel diseases: Is there a relation?. J Pediatr Gastroenterol Nutr 2013; 56:182–5.
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000; 283:2008–12.
- Safarpour AR, Hosseini SV, Mehrabani D. Epidemiology of inflammatory bowel diseases in iran and Asia: A mini review. Iran J Med Sci 2013; 38:140–9.
- Subasinghe D, Nawarathna NMM, Samarasekera DN. Disease characteristics of inflammatory bowel disease (IBD): Findings from a tertiary care centre in South Asia. J Gastrointest Surg Off J Soc Surg Aliment Tract 2011; 15:1562–7.
- Yoshida Y, Murata Y. Inflammatory bowel disease in Japan: Studies of epidemiology and etiopathogenesis. Med Clin North Am 1990; 74:67–90.
- Yang SK, Hong WS, Min YI, et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong District, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol 2000; 15:1037–42.
- Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology 2013; 145:158-165.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at , Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Masoud Ahmad Al-Ghamdi1, Manal Abdulaziz Murad2, Reem Mohammed Alshiakh3, Hoda Jehad Abousada4*, Mohammed Bandar Alharbi5, Rawiah Abubkr Almehdhar5, Turki Saad Aljuhani5, Abdullah Mohammed H Alsobyei5, Abdulrahman Hussain Alharbi6, Ghanem Ahmed AL Ghanem6, Saud Ali Alharbi6, Abdulaziz Shelash Alonezi6, Rashed Saleh A Alghamdi6, Razan Talal Almowllad7 and Fatimah Mohammed Alfaqih7
1Department of General, Laproscopic and Colorectal Surgery, King Fahad general hospital, Jeddah, KSA2Department of Family Medicine, KAU, Jeddah, KSA
3Department of General Surgery, MOH, Jeddah, KSA
4Department of Obestetric and Gynecology, KAMC, Jeddah, KSA
5General Practitioner, MOH, KSA
6Medical Intern, KSA
7Medical Student, KSA
Citation: Masoud Ahmad Al-Ghamdi, Manal Abdulaziz Murad, Reem Mohammed Alshiakh, Hoda Jehad Abousada, Mohammed Bandar Alharbi, Rawiah Abubkr Almehdhar, Turki Saad Aljuhani, Abdullah Mohammed H Alsobyei, Abdulrahman Hussain Alharbi, Ghanem Ahmed AL Ghanem, Saud Ali Alharbi, Abdulaziz Shelash Alonezi, Rashed Saleh A Alghamdi, Razan Talal Almowllad, Fatimah Mohammed Alfaqih, Prevalence and Complications of Inflammatory Bowel Disease among Saudi Population: A Cross-Sectional Study, J Res Med Dent Sci, 2022, 10(1): 258-264
Received: 10-Dec-2021, Manuscript No. JRMDS-21-49229; , Pre QC No. JRMDS-21-49229 (PQ); Editor assigned: 13-Dec-2021, Pre QC No. JRMDS-21-49229 (PQ); Reviewed: 27-Dec-2021, QC No. JRMDS-21-49229; Revised: 30-Dec-2021, Manuscript No. JRMDS-21-49229 (R); Published: 06-Jan-2022