Research - (2021) Volume 9, Issue 5
Prevalence of Causative Factors Involved in Hematemesis
Prakhar Nagar, P Vardaraju and K Kuberan*
*Correspondence: K Kuberan, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
The associated co-morbid illness plays a significant role in deciding the mortality. Oesophago-Gastro-Duodenoscopy was used as a diagnostic and therapeutic tool in the management of UGIB. The most common finding was Gastritis, followed by Erosive Gastritis. Thus, Peptic ulcer disease is the commonest cause of UGIB. The Rock all score was used to triage the non-variceal upper gastrointestinal bleed patients into low and high-risk strata, and it was proved that higher the Rock all score, higher will be the mortality. Radiological and surgical interventions should be considered in patients refractory to conservative management, depending upon the circumstances. Mortality rate in our institute is 4%, which is best explained by the availability of an Upper GI bleed center and strict adherence to formed protocols. To analyze the incidence and severity of presentation, predict the prognosis and mortality risk of Non variceal bleeding using Rock all scoring system, delineate the specific cause and bleeding site using OGD Scopy and management of Upper GI bleeding.
Keywords
Oesophago-gastro-duodenoscopy, GI bleed, Pepticulcer, Gastritis
Introduction
Upper Gastrointestinal bleeding is a common potentially life-threatening condition associated with high morbidity, mortality, and medical care costs. Clinically manifests as haematemesis and, or melena and rarely haematochezia with or without haemodynamic compromise.
Upper Gastrointestinal bleeding is defined as bleeding proximal to the ligament of Treitz. The incidence of UGI bleeding is approximately 100 cases per 100,000 population per year. Mortality rates from UGI bleeding are 6 – 10 % overall [1]. Accurate patient evaluation and appropriate early management is critical to decrease the morbidity and mortality. The foundation of diagnosis and management of patients with Upper GI Bleeding is Oesophago-Gastro-Duodenoscopy (OGD). Endoscopy has a sensitivity of 92% for identification of the site of (AUGIB), with a specificity that approaches 100%, especially if it is done within the first 24 hour of (AUGIB) [2]. Various scoring systems have been used in the prediction of risk in patients with Upper GI bleeding and early stratification in accordance with clinical symptoms.
Materials and Methods
Inclusion criteria
All patients with age groups 20 to 85 years admitted with Upper GI bleeding in Trauma ward.
Exclusion criteria
Children and patients with age groups below 20 years with Upper GI bleeding.
A Proforma will be made that includes detailed history, physical examination, basic investigations and other relevant investigations required. Clinical diagnosis will be made accordingly. Risk stratification will be done using Rock all risk scoring system. Triage, intensive monitoring and general supportive therapy done for the patients will be recorded. Endoscopic findings and various modalities of treatment are compared and analysed.
Results
Total number of cases–100.
Mean Age of presentation–45 years.
Male: Female ratio–89:11 (Figure 1).
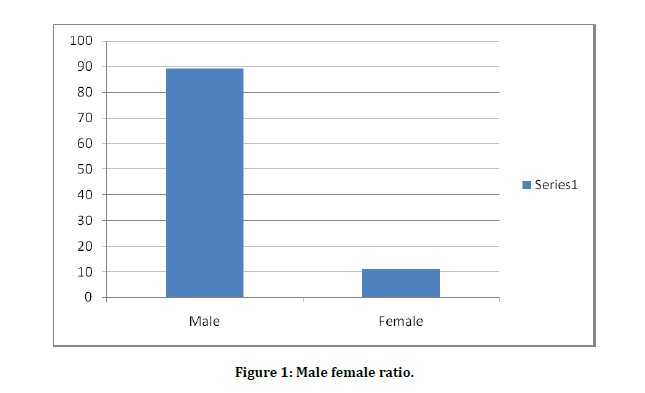
Figure 1: Male female ratio.
Further detailed results are explained in the form of Tables (Tables 1-5) and Figures (Figure 2-5).
Table 1: Clinical severity of upper gastrointestinal bleeding.
| Mild (<500 ml) | 58 |
| Moderate (500–1500 ml) | 36 |
| Severe (>1500 ml) | 6 |
Table 2: Clinical presentation.
| Hematemesis | 100% |
| Malena | 45% |
| Abdomen pain | 69% |
| Haematochezia | 12% |
| Heart burns | 32% |
| Jaundice | 4% |
| Previous Upper GIT surgery | 1% |
| Loss of weight and appetite | 5% |
| Foreign body ingestion | 2% |
Table 3: Co-morbidities.
| Hypertension | 12% |
| Diabetes | 11% |
| Coronary artery Disease | 19% |
| Chronic liver disease | 5% |
Table 4: Impact of Rock all score with mortality.
| Rockall score | Frequency | Percent |
|---|---|---|
| 0 | 2 | 2 |
| 1 | 22 | 22 |
| 2 | 32 | 32 |
| 3 | 27 | 27 |
| 4 | 8 | 8 |
| 5 | 5 | 5 |
| 6 | 4 | 4 |
| Total | 100 | 100 |
Table 5: Independent samples t-Test to compare mean age between survival and death in upper GI bleeding.
| Death | N | Mean | Std. Dev | t-Value | P-Value | |
|---|---|---|---|---|---|---|
| Age | No | 96 | 44.72 | 12.677 | 0.769 | 0.497 |
| Yes | 4 | 55 | 26.608 |
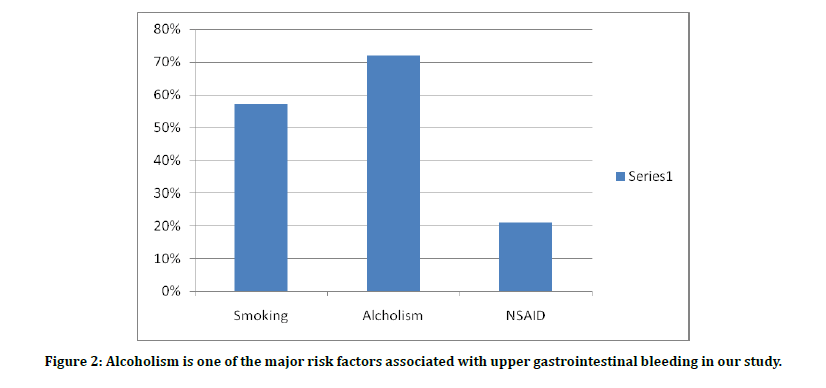
Figure 2: Alcoholism is one of the major risk factors associated with upper gastrointestinal bleeding in our study.
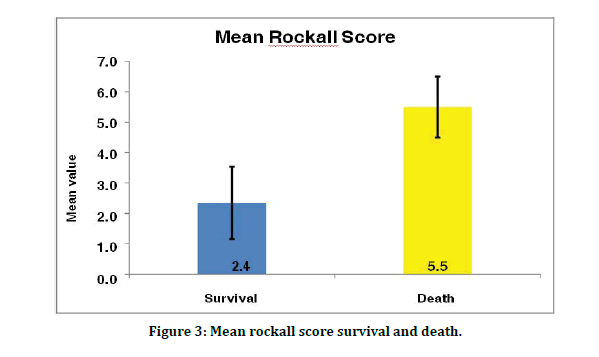
Figure 3: Mean rockall score survival and death.
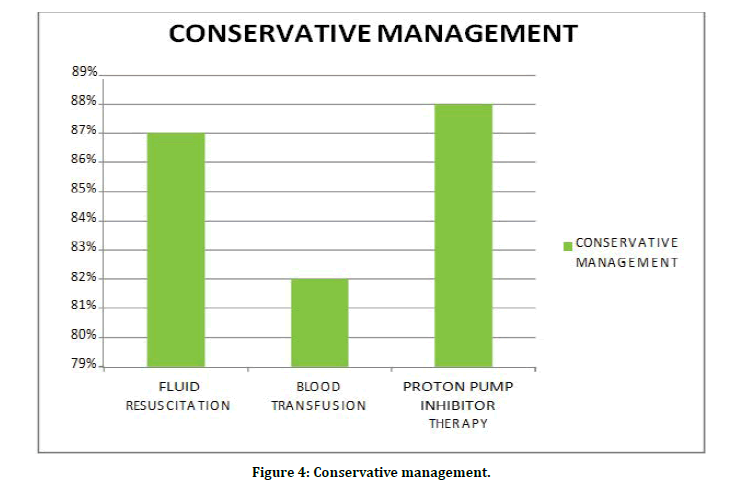
Figure 4: Conservative management.
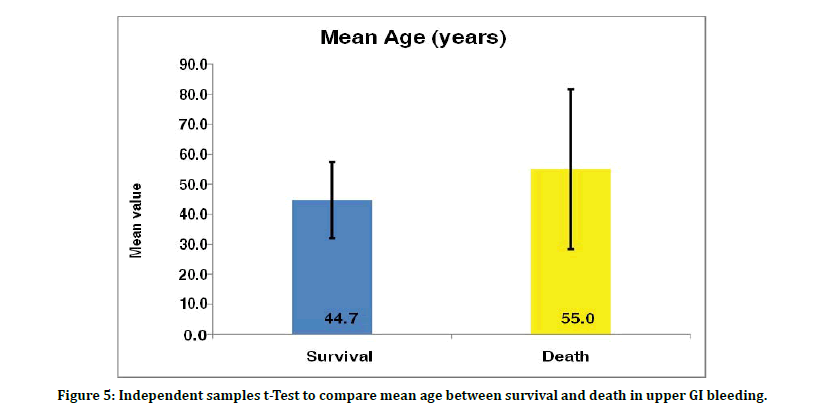
Figure 5: Independent samples t-Test to compare mean age between survival and death in upper GI bleeding.
Initial fluid resuscitation with crystalloids and colloids were given in 87% of patients, 82% of patients were given blood transfusion and 88% of patients were managed with proton pump inhibitor therapy (Figure 4).
Discussion
Upper Gastrointestinal bleeding is one of the most common emergencies in the surgical department that carries 6 to 10 % mortality worldwide [1]. Our study was a prospective clinical study on evaluation and management of Upper gastrointestinal bleeding in patients admitted in our institute (sree balaji medical college) in one year. We excluded children and patients under the age of 20 years from this study. We assessed the clinical presentation, co-morbidities, associated risk factors, OGD findings (within 24 hours of presentation), need of initial resuscitation, blood transfusion and intervention procedures like therapeutic endoscopy, radiological intervention, or emergency laparotomy.
A total of 100 cases were taken up for the study. In these patients, the mean age of presentation was 45 years with a standard deviation of 13. Minimum and maximum age of presentation in the final study was 20 and 79 years respectively with sex distribution predominantly seen among males (89% ) than females (11% ). The maximum number of age group is between 31 – 40 years as shown in the Figure 2.
The severity of bleeding was classified into mild, moderate, and severe depending upon the quantity of blood loss. Majority of patients ( 58% ) were presented with mild hematemesis (<500 ml ), 36% 0f patients presented with moderate hematemesis ( 500 – 1500 ml ) and only 6% presented with severe hematemesis (>1500 ml ) as shown in Table 1. We had 58 patients in mild, 36 patients in moderate and 6 patients in severe form of which 4 patients were died in spite of resuscitative measures.
All our patients admitted with haemetemis had Abdomen pain in 69 of them. About 45 patients had malena, 12 patients were presented with haematochezia and 32 patients had history of heart burns. History of anorexia and weight loss were observed in 5 patients while jaundice were noted in 4 patients as shown in Table 2 and Figure 3.
The mortality rate was 4% in our study with mean age of survival and mortality being 44 and 55 year, respectively. Thus, elderly people withstand less well to UGIB than younger patients. The major contributing factor that leads to death was blood loss, which inturn leading to hypovolemic shock.
The incidence of risk factors like Smoking, Alcoholism and NSAIDs drug intake were considered in our study and the impact with mortality have also been been compared. Smoking is seen in 57 % of patients while the incidence of alcohol was seen with 72 %. Around 21 % of patients were having NSAIDs intake. Most of thepatients took NSAIDS for arthritis and myalgia. Thus, it can be clearly delineated from the Chart.4 that alcoholism i s one of the major risk factors causing Upper GI bleeding and almost, always associated with Peptic ulcer disease. Mortality rate also stands high in patients with alcoholism (75% ) than the other two risk factors (50%) as shown in Figure 5. The associated co-morbid illness in our study were Hypertension (12%), Diabetes (11%), Coronary Artery Disease (19%) and Chronic liver disease ( 5% ) as noted in Table.3. One of our patients died had associated history of old coronary artery disease and another patient had chronic liver disease leading to portal hypertension. Thus, it can be stated that, associated co-morbid factors had a strong link with mortality.
OGD is very useful to delineate the site of bleeding and to facilitate targeted therapy. It defines the low risk and high-risk strata and helps to identify the appropriate candidates for a period of hospital stay or intervention procedures if neded. Risk – stratification scores that incorporate endoscopic data, such as the complete Rock all score, propose that such scores are superior to clinically based scores because they define a greater proportion of all patients at low risk for adverse outcomes related to acute upper gastrointestinal bleeding. The pattern of Upper GI bleeding in our study was shown in Table.4. The commonest OGD finding in our study was Gastritis (25%), followed by Erosive gastritis (13%). Thus, around 38% of the patients had gastric inflammation or erosions, of which 32 patients were alcoholics. The second commonest cause was found to be Oesophagitis (9%), followed by Duodenitis (8%) and Mallory weiss tear (5%). There was not able to identify any lesion in about 4% of the individuals. More than a single site lesion like Gastritis + Duodenitis, Oesophagitis + Gastritis can be seen in 3 and 2 % of patients respectively while Gastric and Duodenal ulcers were seen in 2 and 4% respectively. Stigmata of recent haemorrhage (SRH) were found in 5 patients with UGIB. Malignancies were noted in 4 patients of UGIB.
In our study, stomal ulcer bleeding was seen only in 1 patient. A foreign body, needle was the cause of hematemesis in one patient. Variceal bleeding from Oesophageal and fundal varices constitutes 4% of UGIB in our study. According to the study by other researchers the most common endoscopic findings were Gastric ulcer (23.1) and oesophageal varices (23.1), followed by Duodenal ulcer (13.9), Mallory weiss tear (10.2), Gastritis (4.7), Duodenitis (3.7) and Oesophagitis (3.7). According to the study 24% had Duodenal ulcer, 24.4% had Gastritis/ Erosions, 22.3 % Gastric ulcer, 11.3 %. Oesophageal varices, 8.2% Mallory weiss tear, 7.3% Oesophagitis, 6.8% Duodenitis, 2.8% Neoplasms, 1.9% Stomal ulcer.
Based on the clinical variables like age, the pre sence of shock and the presence of co-morbid illness, the clinical Rockall score was calculated for each patient with non-variceal bleeding. The original rockall scoring was calculated by totaling the clinical and endoscopic scoring systems. It clearly showed that majority of the patients (32) were with the score of 2. Only 5 and 4 patients had the score of 5 and 6 respectively with mortality rate being 4% among them. Thus, it concludes that, higher the rockall score, higher the mortality with significant P value of < 0.001 as shown in the Table.6. The mean Rockall score was 2.4 and 5.5 among the survival and death respectively as shown in the Chart.7. Thus in our study we could stratify patients with a total rockall score of 4 and below as low risk strata and with a score of 5 and above as high risk strata. Rockall scoring has been validated in multiple patient populations across a range of health sittings. It appears to be a valid predictive index that relies on clinical and endoscopic data for assessing the risk of subsequent recurrent bleeding and mortality in patients with acute UGIH.
Patients presented with Upper GI bleeding in emergency ward was prioritized to start initial resuscitation according to the clinical presentation. Peripheral line or Central venous line, Ryles tube insertion and Foley’s catheterization would be started with intense monitoring of vital signs and urine output. Endotracheal intubation should be attempted in necessary conditions.
Initial fluid resuscitation should be given with crystalloids like Ringer lactate or Normal saline of about 500 ml within the first 30 minutes, followed by colloids like haemacel to maintain the intravascular volume. Compatible cross matched blood transfusion should be started as soon as possible to counteract the blood loss due to hematemesis. Fresh frozen plasma or Platelet’s transfusion can also be given depending upon multiple factors, including bleeding severity, bleeding rate, presence of other coagulopathies, and presence of qualitative platelet defects, such as those induced by NSAIDs. Cardiorespiratory support, and treatment of significant comorbid diseases, such as sepsis or coronary artery disease must be given importance to prevent morbidity. Patients usually receive supplemental oxygen by face mask or nasal prongs to counteract the loss of oxygen carrying capacity from blood loss.
In patients suggestive of Non variceal bleeding, high-dose Proton pump inhibitor therapy i.e, initial intravenous bolus of Pantoprazole 80 mg followed by continuous infusion (Pantoprazole 8 mg/hr) for up to 72 h should be given. This therapy ideally be given prior endoscopy. In our study, 87% of patients were managed with initial fluid resuscitation with crystalloids and colloids, blood transfusion was given in 82% of individuals and 88% of patients had given proton pump inhibitor therapy.
Early OGD will significantly improves the clinical outcome in special circumstances requiring urgent endoscopic hemostasis, such as severe, ongoing hemorrhage or esophageal variceal hemorrhage. Bleeding form vaices is mainly because of dysfunction of liver and bleeding varices which are refractive to the treatment. The selection of therapy for bleeding esophageal varices remains controversial. Of all the modes of treatment, in recent years attention was focused on the relative merits of portosystemic shunting, devascularization of esophagus on one hand and the endoscopic procedures to control the bleeding from esophageal varices on the other hand.
The use of endoscopy therapeutically, minimizes the blood transfusion requirements and reduces the length of stay in intensive care set up. Injection therapy can be done over the bleeding site using normal saline or diluted epinephrine. The use of Cautery devices like heater probes, neodymium yttrium aluminum garnet lasers, argon plasma coagulation, and electrocautery probes were used to coagulate blood vessels (coaptation). Clips and band ligation devices were also deployed over the bleeding site to control it. In our study. therapeutic interventions were needed in 2 patients whose OGD findings showed Gastric polyp and Foreign body. Endoscopic polypectomy and Endoscopic foreign body (needle) extraction were done in the above said cases.
Endoscopic variceal band ligation (EVL) was done in a patient who had presented with Upper GI bleeding and OGD showing Grade III oesophageal varices. The results from 6 randomized control trials showed that, Endoscopic variceal ligation is superior to Endoscopic sclerotherapy (EST) and a meta-analysis has confirmed the superiority of EVL over EST. It was stated that, Endoscopic variceal ligation should be repeated every 2 to 4 weeks to eradicate the varices. Concomitant Beta-blocker therapy should also be considered for effective treatment.
Radiological intervention was required for 2 cases in our study. Angiography along with transcatheter embolization proved to be valuable as a non-operative option for selected patients with non-variceal upper gastrointestinal bleeding. Micro coils like, fibred platinum coils of size ranging from 2–10 mm in diameter are used. These coils decrease the perfusion pressure thus allowing the bleeding vessel to get thrombose, once deployed in a distal artery. Coil embolization of Gastro duodenal artery was done, and the patient was improved symptomatically.
In our study, Laparotomy was done for 4 cases. The operations for bleeding duodenal ulcer are oversewing of the ulcer with or without vagotomy and drainage procedures. Oversewing alone is associated with higher ulcer recurrence but have lower mortality rate. Emergency laparotomy was done for a case of Refractory haemetemis with pharmacological and endoscopic management. OGD finding was duodenal bulb ulcer with visible spurting vessel. Endoscopic banding was failed due to continuous bleeding. Laparotomy was done, under running sutures made over the spurting vessel followed by truncal vagotomy and pyloroplasty.
For other three patients with carcinoma stomach, fluid resuscitation and blood transfusion were given initially to stabilize the patient and thorough evaluation was made with investigations. Surgical resection of the growth with adequate margins is the only curative treatment for carcinoma stomach. R0 resection is the goal of surgical treatment. The standard surgery for stomach growth is, Radical subtotal gastrectomy, Billroth II gastrojejunostomy with Roux en Y anastomosis. The operative mortality for this procedure is around 2 to 4 %. Depending upon the per operative findings, procedure can be modified. Palliative procedures like anterior gastrojejunostomy or Feeding jejunostomy can be undertaken in case of locally advanced or metastased gastric carcinoma.
In our study, Elective laparotomy was made and one patient with antro pyloric growth underwent subtotal gastrectomy, roux-en-Y anastomosis with D2 resection. Another patient with carcinoma stomach with transverse mesocolon infiltration was managed with palliative anterior gastro jejunostomy, while the elderly patient with advanced carcinoma stomach with peritoneal and liver secondaries underwent feeding jejunostomy. From the Table.7 and Chart.10, it can be stated that, the mean age of survival among the individuals with upper gastrointestinal bleeding was 44 years and the mortality was seen among the patients with group of around 55 years [3-18].
Conclusion
More than half of the patients presented to the emergency ward with mild hematemesis whereas mortality was found to be in individuals with severe hematemesis. Among the risk factors studied, alcoholism appears to be a major risk factor almost always associated with peptic ulcer disease and 3/4 increased risk for mortality.
The associated co-morbid illness plays a significant role in deciding the mortality. Oesophago-Gastro-Duodenoscopy was used as a diagnostic and therapeutic tool in the management of UGIB. The most common finding was Gastritis, followed by Erosive Gastritis. Thus, Peptic ulcer disease is the commonest cause of UGIB.
The Rock all score was used to triage the nonvariceal upper gastrointestinal bleed patients into low and high-risk strata and it was proved that higher the Rock all score, higher will be the mortality. Radiological and surgical interventions should be considered in patients refractory to conservative management, depending upon the circumstances. Mortality rate in our institute is 4%, which is best explained by the availability of an Upper GI bleed centre and strict adherence to formed protocols.
Funding
No funding sources.
Ethical Approval
The study was approved by the institutional ethics committee.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding: A meta-analysis. AnnIntern Med 1995; 123:280–287.
- Savides TJ, Jensen DM, Cohen J, et al. Severe upper gastrointestinal tumor bleeding: endoscopic findings, treatment, and outcome. Endoscopy 1996; 28:244-248.
- Norton ID, Petersen BT, Sorbi D, et al. Management and long-term prognosis of Dieulafoy lesion. Gastrointest Endosc 1999; 50:762-767.
- Marwick T, Kerlin P. Angiodysplasia of the upper gastrointestinal tract: clinical spectrum in 41cases. J Clin Gastroenterol 1986; 8:404–407.
- Gostout CJ, Viggiano TR, Ahlquis DA, et al. The clinical and endoscopic spectrum of the Watermelon stomach. J Clin Gastroenterol 1992; 15:256–263.
- Lemos DW, Raffetto JD, Moore TC, et al. Primary aortoduodenal fistula: a case report and review of the literature. J Vasc Surg 2003; 37:686-689.
- Cheng CL, Lee CS, Liu NJ, et al. Overlooked lesions at emergency endoscopy for acute non variceal upper gastrointestinal bleeding. Endoscopy 2002; 34:527–530.
- Rockall TA, Logan RF, Devlin HB, et al. Selection of patients for early discharge or outpatient care after acute upper gastrointestinal haemorrhage. National Audit of Acute Upper Gastrointestinal Haemorrhage. Lancet 1996; 347:1138–1140.
- Forest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet 1974; 2:394-397.
- Chey WD, Wong BCY. Practice parameters committee of the american college of gastroenterology: American college of gastroenterology guideline on the management of helicobacter pylori infection. Am J Gastroenterol 2007; 102:1808.
- Rafique MZ, Ul Haq T, Ud Din GN, et al. Transcatheter embolization of acute nonvariceal gastrointestinal hemorrhage. J Coll Physicians Surg Pak 2005; 15: 81-84.
- Abraldes JG, Bosch J. Somatostatin and analogues in portal hypertension. Hepatology 2002; 35:1305–1312.
- Sanyal AJ, Freedman AM, Luketic VA, et al. Transjugular intrahepatic portosystemic shunts for patients with active variceal hemorrhage unresponsive to sclerotherapy. Gastroenterology 1996; 111:138–146
- de la Fuente SG, Khuri SF, Schifftner T, et al. Comparative analysis of vagotomy and drainage versus vagotomy and resection procedures for bleeding peptic ulcer disease: Results of 907 patients from the department of veterans affairs national surgical quality improvement program database. J Am Coll Surg 2006; 202:78-86.
- Sarfeh IJ, Rypins EB. Partial versus total portacaval shunt in alcoholic cirrhosis: Results of a prospective, randomized clinical trial. Ann Surg 1994; 219:353–361.
- Silverstein FE, Gilbert DA, Tedesco FJ, et al. The national ASGE survey on upper gastrointestinal bleeding: Study design and baseline data. Gastrointest Endosc 1981; 27:73–79 .
- Cho CS, Brennan MF. Gastric adenocarcinoma, in Cameron JL (Ed): Current Surgical Therapy , 9th Edn. Philadelphia: Mosby, 2008.
- Fullarton GM, Birnie GG, MacDonald A, e t al. Controlled trial of heater probe treatment in bleeding ulcer patients. Br J Surg 1989; 76:541–544.
Author Info
Prakhar Nagar, P Vardaraju and K Kuberan*
Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Prakhar Nagar, P Vardaraju, K Kuberan, Prevalence of Causative Factors Involved in Hematemesis, J Res Med Dent Sci, 2021, 9 (5):124-131.
Received: 20-Mar-2021 Accepted: 19-May-2021 Published: 31-May-2021
