Research - (2019) Volume 7, Issue 2
Prognostic Factors for the Development of Amputations in People with Type 2 Diabetes Mellitus
Víctor Horacio Orozco-Covarrubias1*, Carlos Enrique Cabrera-Pivaral1, María de los Ángeles Aguilera-Velasc1, Noé Alfaro-Alfaro1, Guillermo González-Gálvez2 and Blanca Leticia Sánchez-Michel3
*Correspondence: Víctor Horacio Orozco-Covarrubias, Centro Universitario de Ciencias de la Salud, Universidad de Guadalajara, Guadalajara, Mexico, Email:
Abstract
Introduction: The importance of this research lies in the determination of the prognostic factors that predict the clinical course of amputations in people with diabetes mellitus type 2 (DM2), the identification of these factors are of great interest for secondary and tertiary prevention of complications in DM2.
Objective: To determine the main prognostic factors for the development of amputations in people with DM2.
Material and Methods: A matched case-control study with a ratio of 1: 1 was carried out, with a total of 268 people diagnosed with DM2 included in the study, of whom 134 were cases (of DM2 with amputation) and 134 were controls (DM2 without amputation). The analysis of the relationship between risk factors and amputations was made through the measure of association Odds Ratio (OR) and developing a predictive model with the main prognostic factors for the development of amputations.
Results: It was demonstrated that HbA1c greater than 8% is the main prognostic factor for the development of the pathologies that lead to amputations, such as the presence of ulcers in lower limbs (OR of 2.8, p of 0.00), the presence of diabetic neuropathy (OR of 3.6, p of 0.01) and peripheral arterial disease (PAD) (OR of 2.5, p of 0.05).
Conclusion: The main prognostic factors identified for the development of amputations in people with DM2 are the increase in HbA1c greater than 8%, the history of ulcers, PAD and diabetic neuropathy. For the prevention of amputations and the main pathologies that lead to the development of these, metabolic control is essential through an adequate control of HbA1c levels.
Keywords
Diabetes mellitus type 2, Amputation, Diabetic foot, Risk factors
Introduction
The importance of this research lies in the determination of the prognostic factors that predict the clinical course of amputations in people with diabetes mellitus type 2 (DM2), the identification of these factors are of great interest for the secondary and tertiary prevention of complications in DM2.
At an international level, the prevalence of diabetic foot is between 8% and 13% of people with diabetes mellitus (DM) [1]. In Mexico, the prevalence of diabetic foot is increasing, as mentioned in the National Health and Nutrition Survey (ENSANUT 2016). In 2012, there was a prevalence of diabetic foot of 7.2%, which for the year 2016 increased to a 9.1% [2].
In the words of Eusko [3] the problem of diabetic foot as a complication of DM is one of the most dramatic, where approximately 20% of people who have a diabetic foot episode die before a year, it has been calculated that one of every five people with DM will present a picture of diabetic foot in the course of their life.
Amputations in the lower limbs are the main complication of diabetic foot, between 70 and 80% of amputations are preceded by a diabetic foot in people with DM [1]. The incidence of amputations in people with DM is between 2.5-6/1000 patients/year [4]. Every 30 seconds, somewhere in the world someone undergoes a total or partial amputation of a lower limb because of DM, considering itself as the first cause of non-traumatic amputation of the lower limbs [1]. Where after presenting a major amputation (supracondilea), the 3 year survival is 50% and at 5 years, only 40% of people will survive [5].
The complications of diabetic foot correspond mainly to the lack of prevention, this is often due to two factors, not having knowledge about preventive care or having knowledge, but not the proper practices of these, so not only it is important to know what should be done but also how to perform each care [6].
According to ENSANUT 2016, 46.4% of people with DM, do not take preventive measures to avoid or delay complications of the disease. The preventive measures implemented in a greater proportion by people with DM2 in the last year were: revision of feet (20.9%), measurement of cholesterol and triglycerides (15.2%), application of vaccines against influenza (15.1%), general urine test and microalbuminuria (14.2%) and ophthalmological review (13.1%), where only 9% of people received health education [2].
The assessment of the feet should be comprehensive since anatomical and functional alterations should be investigated during the early stages of the disease because they can have functional repercussions even in advanced stages of the disease [7].
As López et al. [8] mention the need to foresee and study diabetic foot disease is a major issue and represents a great medical challenge, reducing the condition of diabetic foot can be translated into positive results to improve the quality of life of people, in addition to the incidence in the socioeconomic aspect, due to the high prevalence of DM in the working population.
The purpose of this document was to determine the main prognostic factors for the development of amputations in people with type 2 diabetes mellitus.
Materials and Methods
A matched case-control study with a ratio of 1:1 was carried out, with a total of 268 people diagnosed with DM2 included in the study, of whom 134 were cases (of DM2 with amputation) and 134 were controls (from DM2 without amputation).
The cases against the controls were compared, making a pairing by sex and age in five-year periods, with hospital controls being one for each case.
The study was conducted in Mexico, in a second level hospital, in 2017, a review of the electronic and physical files of the internal medicine, chest and cardiovascular, endocrinology and orthopedic services was performed. The information was collected in a period of 10 years prior to the presence of amputation.
Stratified random probabilistic sampling was performed according to the different strata with simple affixation.
For the calculation of sample sizes, the following elements were considered:
1. The variables of interest, amputations in qualitative scale.
2. The sample size is calculated with the objective of estimating the population odds ratio.
3. A proportion of expected exposures in controls (group B) of 0.1000.
4. An expected minimum odds ratio of 3.0000.
5. A confidence of 95% (Z1-α/2=1.960).
6. A power of 80% (Z1-β=-0.842).
7. A ratio of 1.0 element in the sample of controls (B) for each element in the sample of cases (A).
Using the formula by Fleiss et al. (Equation 1 and Equation 2) [9]:
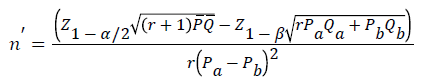
Where,
Z1-α/2='alpha error' that is accepted, expressed in Z value considering a normal distribution of two tails=1.960;
Z1-β='beta error' that is accepted, expressed in Z value considering a normal distribution of a tail=-0.842;
r=quotient of dividing the control number (group B) between the number of cases (group A)=1.00;
Pb=proportion of subjects exposed in the controls (group B)=0.1000;
Qb=1-Pb;
φ=odds ratio to be identified as significant=3.00;
Pa=proportion of subjects exposed in cases (group A)=(φ*Pb)/((1-Pb)+φ*Pb)=0.2500;
Qa=1-Pa;
P=(Pb*r+Pa)/(1+r)=0.1750;
Q=1-P,
We found that for controls (group B) n=112.5, and for cases (group A) n=112.5.
The inclusion criteria were: people with type 2 diabetes mellitus of 10 years of evolution or more, metabolic decontrol with glycosylated hemoglobin (HbA1c) values of 7% to 16% (in case of not having HbA1c, they were included in the study to determine the lack of performance of the test), with or without a history of pelvic member ulcers, presenting ulcers with or without infection, which may or may not include variables of hypertension, smoking, obesity, dyslipidemia, distal diabetic sensory neuropathy, ischemic or disease processes peripheral arterial for cases with pelvic limb amputation and for controls witho ut pelvic limb amputation.
The analysis of the relationship between risk factors and amputations was made through the measure of association Odds Ratio (OR) and developing a predictive model with the main prognostic factors for the development of amputations, to predict the probability that there is an amputation with respect to the independent variables as risk factors; the main independent variables were taken into account: the years of evolution with DM2, the history of ulcers, peripheral arterial disease (PAD), diabetic neuropathy (DN), the increase in HbA1c and, were related to the dependent variable amputation. Free and informed consent was obtained, tacitly on the part of the participants, based on article 6 of the Universal Declaration of Human Rights and articles 21, 22 and 24 of the Regulation of the General Law of Health in the Matter of Research for Health. The Research and Ethics Committee of the second level Hospital approved the research. The Jalisco Secretary of Health, granting the state registration No. 0165/17 HCJIM/2017 requested a state registry.
Results
Study was done on 268 people (134 cases and 134 controls). With respect to the socio-demographic characteristics presented in this research, age and gender between cases and controls there is no statistical difference, since the groups were homogenized. It was identified that the groups of schooling that had the highest prevalence for the development of amputations were the incomplete primary with 25% and the primary with 40%, thus presenting a higher number of cases with amputations compared to the secondary groups with 15%, high school with 7% and undergraduate with only 2%; thus establishing an inverse correlation between the lower schooling and the increase in amputations. In the study, those presented in Table 1 were determined as the main risk factors for amputations.
| Variables | Cases | Controls | OR | CI 95% | Value of square chi from Mantel-Haenszel | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Ulcers history | Si | 132 | 98 | 44 | 33 | 135 | 31.9-571 | 0 |
| No | 2 | 2 | 90 | 67 | ||||
| Fisher exact test | CI 95%= 33.2-153.7 | p= 0.00 | ||||||
| PAD | Si | 55 | 41 | 9 | 7 | 9.6 | 4.5-20.5 | 0 |
| No | 79 | 59 | 124 | 93 | ||||
| DN | Si | 48 | 36 | 10 | 8 | 6.9 | 3.3-14.4 | 0 |
| No | 86 | 64 | 124 | 92 | ||||
| HbA1c | >8% | 71 | 53 | 55 | 41 | 2.6 | 1.3-5.2 | 0.01 |
| 7 a 7.9% | 16 | 12 | 32 | 24 | ||||
Table 1: Association of the main risk factors with the presence of amputations
In relation to the increase in HbA1c as a prognostic factor for the development of the main pathologies that lead to amputations, the risks of an increase in HbA1c for the development of ulcers, PAD and diabetic neuropathy in people with DM2 were determined.
Regarding the association of the presence of ulcers with the increase in HbA1c, it was identified in the study that with an increase in HbA1c greater than 8% there was an association with an OR of 2.8 and being significant with a p of 0.00 with which the null hypothesis is rejected, where 75% of the people who presented an elevated HbA1c ended up developing an ulcer. In relation to the association of the presence of diabetic neuropathy with the increase in HbA1c, it was identified that there was an association with an OR of 3.6 and being significant with a p of 0.01, as for the people who did not present the factor of HbA1c risk greater than 8% the 90% of them did not have a diabetic neuropathy. In relation to the association of the presence of PAD with the increase of HbA1c, it was identified that there was an association with an OR of 2.5, being that of the people who did not present the risk factor of HbA1c greater than 8% the 88% of them did not present a PAD (Table 2).
| HbA1c | Ulcers | Without ulcers | Total | OR | CI 95% | Value of p | |||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Greater than 8% | 94 | 75.2 | 31 | 24.8 | 125 | 72.3 | 2.8 | 1.4-5.6 | 0 |
| 7 a 7.9% | 25 | 52.1 | 23 | 47.9 | 48 | 27.8 | |||
| Total | 119 | 68.8 | 54 | 31.2 | 173 | 100 | |||
| Neuropathy | Without neuropathy | ||||||||
| Greater than 8% | 37 | 29.6 | 88 | 70.4 | 125 | 72.3 | 3.6 | 1.3-9.9 | 0.01 |
| 7 a 7.9% | 5 | 10.4 | 43 | 89.6 | 48 | 27.8 | |||
| Total | 42 | 24.3 | 131 | 75.7 | 173 | 100 | |||
| PAD | Without PAD | ||||||||
| Greater than 8% | 33 | 26.4 | 92 | 73.6 | 125 | 72.3 | 2.5 | 1-6.5 | 0.05 |
| 7 a 7.9% | 6 | 12.5 | 42 | 87.5 | 48 | 27.8 | |||
| Total | 39 | 22.5 | 134 | 77.5 | 173 | 100 | |||
Table 2: Association of elevated HbA1c with the development of the main pathologies that lead to amputations
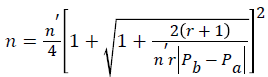
The association of PAD and diabetic neuropathy with the development of ulcers in people with DM2 was determined in the study. In relation to the association of the presence of ulcers with PAD as a risk factor, an association was identified with an OR of 15.7 and being significant with a p of 0.00, which rejects the null hypothesis, being that of people who presented a PAD, 95% of them ended up suffering ulceration. Regarding the association of ulcers with the DN as a risk factor, an association with an OR of 6 was identified and being significant with a p of 0.00, being that of the people who presented diabetic neuropathy 90% of them ended up suffering an ulceration (Table 3). A predictive model was developed with the main prognostic factors for the development of amputations, starting with metabolic decontrol, which leads to other complications until it ends in a greater number of amputations (Figure 1). In relation to the classification of ulcers according to the University of Texas and how they relate to amputations, it was observed that of 71 people who presented an "IID" classification (corresponding to a tendon or capsule wound with infection and ischemia), 53 people ended up presenting an amputation. In addition, with respect to the classification that was presented more in the study that was the classification "IIID" (corresponding to a penetrating wound to bone or joint with infection and ischemia), 97 cases were presented of which 88 ended up presenting an amputation (Figures 2 and 3).
| PAD | Ulcers | Without ulcers | Total | OR | CI 95% | Value of p | |||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Yes | 61 | 95.3 | 3 | 4.7 | 64 | 23.9 | 15.7 | 4.8-51.8 | 0 |
| Not | 115 | 56.4 | 89 | 43.6 | 204 | 76.1 | |||
| Total | 176 | 65.7 | 92 | 34.3 | 268 | 100 | |||
| Neuropathy | |||||||||
| Yes | 52 | 89.7 | 6 | 10.3 | 58 | 21.6 | 6 | 2.5-14.6 | 0 |
| Not | 124 | 59.1 | 86 | 40.9 | 216 | 78.4 | |||
| Total | 176 | 65.7 | 92 | 34.3 | 268 | 100 | |||
Table 3: Association of PAD and diabetic neuropathy with the development of ulcers in people with DM2
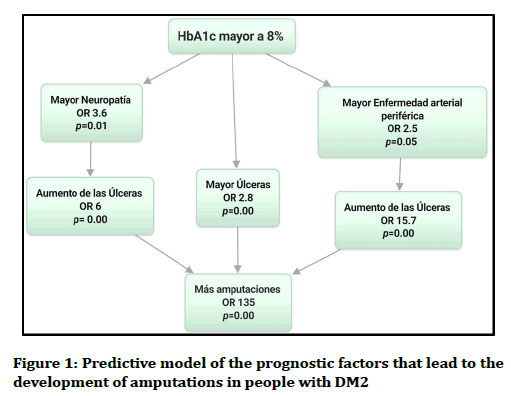
Figure 1. Predictive model of the prognostic factors that lead to the development of amputations in people with DM2
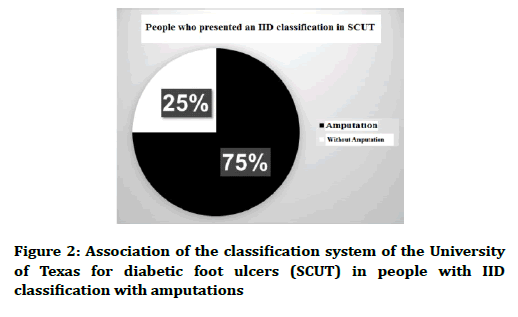
Figure 2. Association of the classification system of the University of Texas for diabetic foot ulcers (SCUT) in people with IID classification with amputations
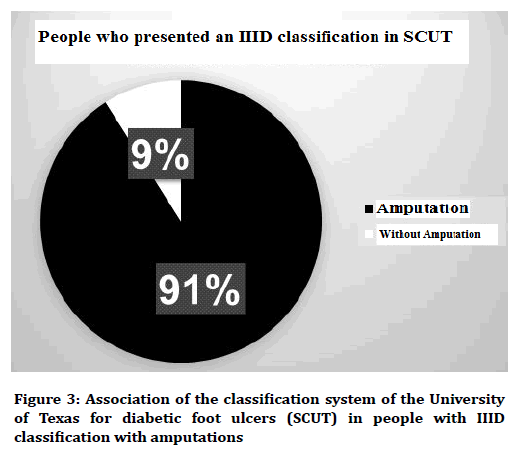
Figure 3. Association of the classification system of the University of Texas for diabetic foot ulcers (SCUT) in people with IIID classification with amputations
Discussion
The main prognostic factors identified for the development of amputations in people with DM2 are the history of ulcers, PAD, diabetic neuropathy and the increase in HbA1c greater than 8%. These factors were determined by means of a statistical analysis with the measure of association of the OR.
The importance of the study resides in the predictive model of the complications that lead to the development of amputations since in the review of the literature it is only contemplated that with the increase of HbA1c greater than 9% complications occur, with our study being demonstrates that with only an elevation of more than 8% of HbA1c is already a strong predictor for the onset of complications that lead to amputations.
The significance of these results for people with DM2 is that with adequate control of HbA1c maintaining levels of less than 8%, it will be possible to prevent up to 75% to 90% of the main complications (ulcers in pelvic limbs, PAD, diabetic neuropathy) that lead to amputations in pelvic limbs.
As mentioned by Alothman et al. [10], of people with amputation in the lower extremities, 49% have DN, 48% ulcer in the foot and 58% have a diagnosis of PAD. Likewise, 28.9% had two risk factors and 23.6% had three risk factors to develop an amputation in the lower extremities.
In the study it was determined that 75% of the people who had a history of ulcers suffered an amputation, presenting a parallelism with other studies where it was identified that amputations were preceded by up to 85% by ulcers [11], while people who did not have ulcers only 2% suffered an amputation. Therefore, the prevention of ulcers is fundamental to avoid the appearance of amputations in people.
As the main prognostic factor for the development of the amputations, the history of ulcers was identified, so it was decided to determine the association that the other factors had for the development of the same. Where of the people who presented PAD 95% of them developed ulceration. Being consistent with other studies conducted such as, the study by Mohammedi et al. [12], who observed the risk of microvascular disease associated with the high risk of chronic ulceration in the lower extremities, with a hazard ratio 2.1 and the Malyar et al. study [13], which identified that PAD is present in approximately 50% to 70% of ulcers per diabetic foot. Being that people who present a PAD have 15.7% more risk of developing ulceration than people who do not have PAD. In relation to the DN, it was identified that 90% of the people who presented it developed an ulcer. Determining that people who have a DN have 6 times more risk of developing ulceration than people who do not have a neuropathy. With respect to the increase in HbA1c, of the people who had HbA1c levels greater than 8%, 75% of them had ulceration.
It was determined that the main reason why people developed the pathologies that lead to ulcers was metabolic decontrol, so the association of increased HbA1c with PAD and DN was identified, being that people with higher HbA1c 8% have 2.5 more risk of presenting an PAD than people with HbA1c levels below 8%. Where, 12% of people who had HbA1c levels below 8% developed a PAD. As Laiteerapong et al. [14] mentions HbA1c levels ≥ 6.5% are associated with an increase in microvascular and macrovascular events (microvascular: risk ratio 1.2 (95%, CI 1.1-1.4)). The longest periods of exposure to HbA1c levels ≥ 8.0% were associated with an increase in the microvascular event and the risk of mortality.
With regard to the DN, it was identified that people with HbA1c greater than 8% have 3.6 more risk of presenting a DN than people who have HbA1c levels of less than 8%. Whereas 10% of people who had HbA1c levels below 8% developed a DN.
In relation to the classification of ulcers according to the University of Texas, it was determined that a correct physical examination on the feet of people with DM2 is of utmost importance for the timely diagnosis of ulcers on the feet, which is of utmost importance the use of this diagnostic tool to perform an adequate and timely intervention in these wounds, thus avoiding the progression to a more advanced classification, which considerably favors the development of amputations.
In order to improve the health care provided to people with DM2, a continuous training program for health professionals is needed to help improve the care of the population with DM2, providing better care through clinical tools. easy access to health workers but with great importance in the prevention of complications such as the measurement of the ankle arm index, where in Boyko et al. study [15], the macrovascular disease measured by the ankle arm index showed an association with the risk of amputation, since the lower and higher levels were associated with an increased risk of amputation. A high ankle arm index ≥ 1.3 was associated with an increase of more than double the risk of amputation. According to the University of Texas, in order to achieve correct classification of the injuries and a correct detection and identification of the feet at risk, the monofilament test was done.
The main limitations of the study resides in the design of the research being that in the case-control studies the information is obtained from past expositions that are based on the memory or the existence of previous records. In addition to this, the OR, the main statistical measure in these studies, is only an approximation of relative risk as long as the prevalence of the phenomenon of interest is less than 10%.
Conclusion
For the prevention of amputations and the main pathologies that lead to the development of these, metabolic control is essential through an adequate control of HbA1c levels.
To ensure that people are empowered with their health, health education programs should be implemented with the objective of ensuring that people have knowledge of the dangers and benefits of proper treatment adherence, through proper nutrition and physical activities that must be followed to improve and preserve your health. As well as illustrative information to make you, aware of the complications associated with DM and the teaching of specific actions to be carried out at home to avoid the appearance of injuries to your feet.
Conflict of Interest
In order to guarantee the integrity and validity of the research, the researchers declare that there are no conflicts of interest, given that the present work does not intend to show the institution or the staff, nor are there any economic interests involved, given that the study was self-financed.
References
- Cho NH, Kirigia J, Mbanya JC, et al. IDF diabetes Atlas.
- Hernández-Ávila M, Rivera-Dommarco J, Shamah-Levy T, et al. International Diabetes Federation: National Survey of Health and Nutrition of Midway, 2016. Final Results Report 2016.
- www.guiasalud.es/GPC/GPC_429_Diabetes_2_Osteba_compl.pdf
- Domínguez MC, Fernández IP. Clinical practice guide for type 2 diabetes mellitus. Arch Med 2014; 10:2.
- Mendoza OF, Moreno ÁG. Amputation, disarticulation: Definition, indications; upper and lower limb amputation levels: Types of orthosis or prosthesis; amputation in children and in peripheral vascular diseases; operative techniques. Cirugía Radical Aparato Locomotor 2012: 235-44.
- Jiménez EG, Martínez BMT, Gómez AM, et al. Level of knowledge about diabetes mellitus in patients with type 2 diabetes. Medisur 2007; 5.
- salud.edomex.gob.mx/cevece/dt_reportes
- López FR, Yanes SR, Suárez SPR, et al. Predictive statistical model for diabetic foot disease in patients with type II diabetes mellitus. Medisur 2016; 14:42-52.
- Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. John Wiley & Sons 2013.
- Alothman S, Alenazi A, Waitman LR, et al. Neuropathy and other risk factors for lower extremity amputation in people with diabetes using a clinical data repository system. J Allied Health 2018; 47:217-21.
- Agale SV. Chronic leg ulcers: Epidemiology, aetiopathogenesis, and management. Ulcers 2013; 2013:1-9.
- Mohammedi K, Woodward M, Hirakawa Y, et al. Microvascular and macrovascular disease and risk for major peripheral arterial disease in patients with type 2 diabetes. Diabetes Care 2016; 39:1796-803.
- Malyar NM, Freisinger E, Meyborg M, et al. Amputations and mortality in in-hospital treated patients with peripheral artery disease and diabetic foot syndrome. J Diabetes Complications 2016; 30:1117-22.
- Laiteerapong N, Ham SA, Gao Y, et al. The legacy effect in type 2 diabetes: Impact of early glycemic control on future complications (the Diabetes & Aging Study). Diabetes Care 2019; 42:416-26.
- Boyko EJ, Seelig AD, Ahroni JH. Limb-and person-level risk factors for lower-limb amputation in the Prospective Seattle Diabetic Foot Study. Diabetes Care 2018; 41:891-8.
Author Info
Víctor Horacio Orozco-Covarrubias1*, Carlos Enrique Cabrera-Pivaral1, María de los Ángeles Aguilera-Velasc1, Noé Alfaro-Alfaro1, Guillermo González-Gálvez2 and Blanca Leticia Sánchez-Michel3
1Centro Universitario de Ciencias de la Salud, Universidad de Guadalajara, Guadalajara, Mexico2Jefe Del Servicio de Endocrinología en el Hospital Civil de Guadalajara "Dr. Juan I. Menchaca", Guadalajara, Mexico
3Médico Adscrito al Servicio de Endocrinología Del Hospital Civil de Guadalajara "Dr. Juan I. Menchaca", Guadalajara, Mexico
Citation: Víctor Horacio Orozco-Covarrubias, Carlos Enrique Cabrera-Pivaral, María de los Ángeles Aguilera-Velasco, Noé Alfaro-Alfaro, Guillermo González-Gálvez, Blanca Leticia Sánchez-Michel, Prognostic factors for the development of amputations in people with type 2 diabetes mellitus, J Res Med Dent Sci, 2019, 7(2): 219-224
Received: 30-Mar-2019 Accepted: 25-Apr-2019
