Research - (2023) Volume 11, Issue 4
Rare variant of Ameloblastoma - A Case report of Acanthomatous Ameloblastoma
Shilpi Srivastava1*, Manisha Saxena2, Shiva Prasad Kyasanoor3, Swetha Meruva3 and Harini Gunda4
*Correspondence: Shilpi Srivastava, BDS, General dental practitioner, Mahatma Gandhi dental college and hospital, India, Email:
Abstract
Ameloblastoma is a non-cancerous epithelial odontogenic tumour. Ameloblastoma constitute 1% of all tumor’s and cysts developing in the jaws. It occurs usually in the third and fourth decade of life and sees in the molar ramus region of the mandible. It can have notable impact on patient morbidity and mortality. In this report we present a large multicystic Ameloblastoma in the left body-ramus region of the mandible in a 25-year-old man. The diagnosis was aided by CT and treated by hemi-mandibulectomy. The reconstruction was done by iliac crest bone.Keywords
Ramus, Mandibulectomy
Introduction
Ameloblastoma is tumor of epithelial origin. It is benign odontogenic tumour of the jaws that constitutes about 1% of all cysts and tumours of the jaws. It is usually painless, slow growing, locally aggressive tumour causing expansion and perforation of the lingual or the buccal cortical plate and invading the soft tissues. It has peak incidence in third and fourth decade of life but can be found in any age group with equal gender predilection (1:1). The relative frequency of mandible to maxilla is reported to be varying from 80–20% to 99–1%. In most cases Ameloblastoma are seen in the molar ramus region [1-3]. The aim of this presentation is to give a detailed knowledge about the classification, incidence, and nature, methods of diagnosis and management of ameloblastoma along with the presentation of the case.
Case Presentation
A male of 25 years of age reported to Oral Medicine and Radiology Department, Kota Medical College, with a swelling (Figure 1) on the left side of the face since 2 years. The swelling was gradual in onset and reached the present size. He also complains of pain while chewing food since 3 months. Patient did not give any history of trauma in the past. There was no discharge noted in swelling. The patient find difficulty and pain while chewing hard food. Past history and medical history were not significant. He was taking no medication and had no history of known drug allergy. The physical examination disclosed no abnormality other than those related to the chief complaint. The extra-oral examination showed a solitary ill-defined diffuse swelling over the left lower third of the face. (Figure 1) The superior-inferiorly extension of swelling was 4×5 cm from the left pretragus area to the lower border of the mandible. The swelling spread mediolateral 2 cm from the left corner of the mouth to the left lateral border of the mandible. The colour of mucosa over the swelling was normal and no secondary infection can be noted. The surface was smooth. On palpation the swelling was hard and non-tender. An intraoral examination revealed a vague solitary swelling (Figure 2 and 3) in the left lower posterior buccal vestibule extending from 34 to the retro molar region in antero-posterior direction. The medio-lateral extent was from buccal vestibule to lingual to molars. The mucosa over the swelling was stretched with no colour change. It was non-tender and hard in consistency.
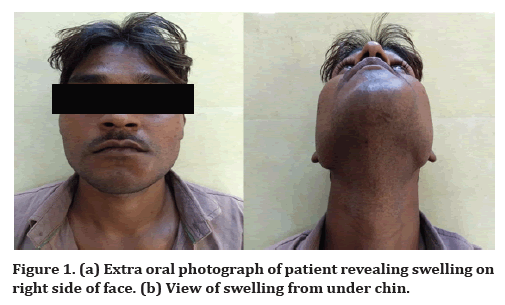
Figure 1. (a) Extra oral photograph of patient revealing swelling on right side of face. (b) View of swelling from under chin.

Figure 2. Intraoral photograph of patient showing swelling on left side of face.
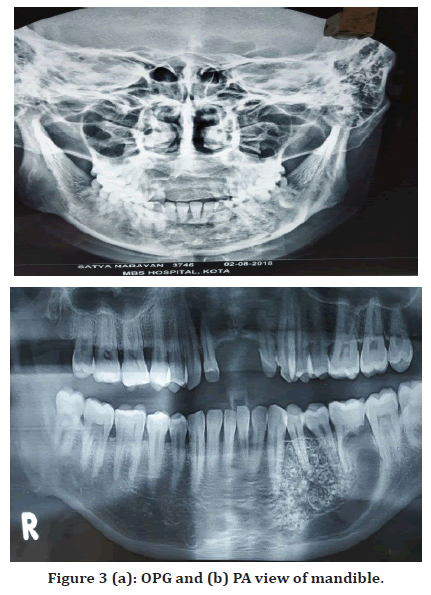
Figure 3. (a) OPG and (b) PA view of mandible.
Expansion of buccal and lingual cortical plate can be seen. Pertaining to the clinical observation, a probable diagnosis of benign tumour of the left side of mandible was made. Ameloblastoma comes on number one on list of differential diagnosis due to place of occurrence and age slot. Second comes odontogenic myxoma which also has same site of occurrence. An intra-oral incisional biopsy was advised and the specimen was sent for histopathological examination.
Investigations
The radiographic and routine hematological examination was performed. No relevant observation was noted in blood reports.
OPG and PA view
The swelling can be seen in OPG and PA view as illdefined radiolucency extending from 33 to retro-molar area.
Computed Tomography
The axial CT of the jaw (Figure 4) shows a very large well-defined radiolucent expansile lesion in the left body and ramus of the mandible causing expansion of the body and ramus. To know about the multilocular nature contrast CT is desired.
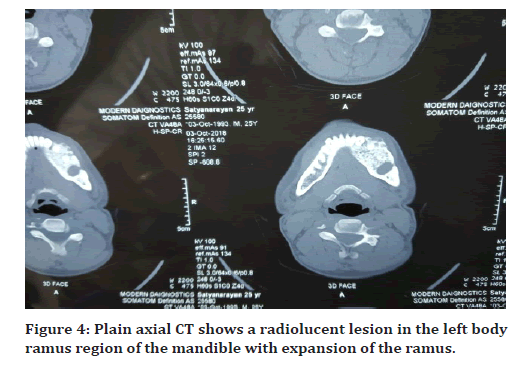
Figure 4. Plain axial CT shows a radiolucent lesion in the left body ramus region of the mandible with expansion of the ramus.
Histopathology
The biopsy specimen revealed circumscribed areas showing haphazardly arranged bony trabeculae irregular islands of desmoplastic surrounding’s islands of squamoid epithelial proliferations which is suggestive of Acanthomatous ameloblastoma.
Treatment
Due to wide involvement hemimandibulectomy was done. (Figure 5) The bone graft was taken from iliac crest bone moulded into shape of mandible and placed and fixed with plates (Figure 6 and 7).
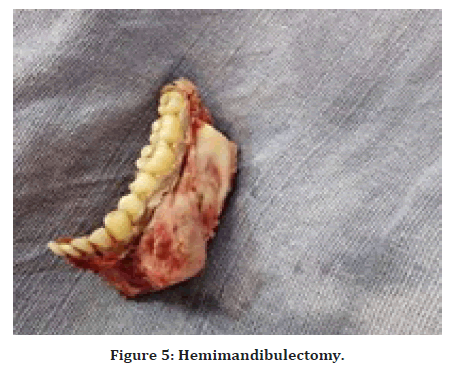
Figure 5. Hemimandibulectomy.
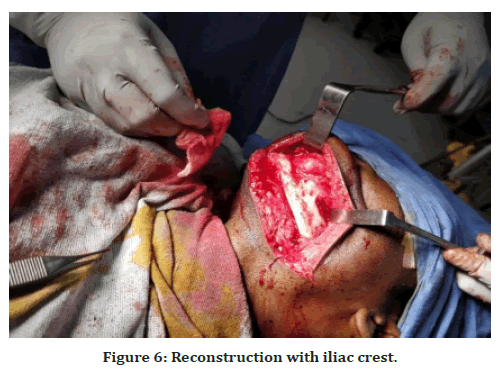
Figure 6. Reconstruction with iliac crest.

Figure 7. Bone graft from iliac crest stabilized with bone plating.
Outcome and follow up
The postoperative healing was good. The patient was looking aesthetically pleasing and function was restored. The patient was kept on follow-up for 6 months with no evidence of complication or recurrence (Figure 8). Currently the patient is under biannual follow-up.

Figure 8. Post-operative picture.
Discussion
The word ameloblastoma originates from the early English word “amel,” meaning enamel and the Greek word “blastos,” meaning germ. The first case was reported by Broca in 1868 and the first detailed description was given by Falkson in 1879. “Adamantinoma,” denotes the formation of hard tissue was coined by Malassez in 1885. Churchill in 1934 put forward the name “ameloblastoma” [4,5]. Ameloblastoma as, “it is usually unicentric, nonfunctional, intermittent in growth, anatomically benign and clinically persistent.” as suggested by Robinson in 1977. The World Health Organization (1991) defined ameloblastoma as a benign but locally aggressive tumor with a high tendency to recur, consisting of proliferating odontogenic epithelium lying in a fibrous stroma [6].
Ameloblastoma can be categorized into 4 subtypes: solid or multicystic, Unicystic, desmoplastic, and peripheral [7]. Multi-cystic or conventional type has multiple large cystic spaces. Unicystic variety or plexiform pattern represents cystic lesions with clinical, radiographic, features of a jaw cyst, but histology resembles a typical ameloblastomatous epithelium lining. They account for 10% of ameloblastoma and are seen in young patients and in anterior part of mandible [8]. According to Gum gum and Hogoren, the plexiform pattern is less aggressive and has a significantly lower recurrence rate [9]. Desmoplastic ameloblastoma resemble a fibroosseous lesion with no obvious ameloblastoma whilst dominated by dense collagenous tissue. The peripheral subtype accounts for 2% of all ameloblastomas.
There are six histologic subtypes of ameloblastoma: follicular, plexiform, acanthomatous, granular, basal cell, and desmoplastic. Data from studies categorized follicular ameloblastoma as the most prevalent histological variant (64.9%). Plexiform (13.0%), desmoplastic (5.2%), and acanthomatous (3.9%) follows the series in descending manner.
Ameloblastoma rarely metastasize and if metastasize, lung is most common place [10].
About 80% of all cases occur in the mandible, of which 70% cases are seen in the ramus [11]. Ameloblastoma in the mandible can increase to great size and cause facial asymmetry, displacement of teeth, loose teeth, malocclusion, and pathologic fractures. Tumor size may range from 1 to 16 cm at presentation which results from expansion of bone and invasion into soft tissue [12]. Patients may come with complain of a slow-growing mass, malocclusion, loose teeth, and sometimes with paresthesia and pain. Many times ameloblastoma are detected incidentally on radiographs in asymptomatic patients [13], noticed swelling of the affected region (38.3%), paranesthesia of the innervated region of the mandibular nerve (13.3%) and altered occlusion of teeth in 10% of cases in most of the mandibular ameloblastoma.
The radiographic picture of ameloblastoma depicts an expansile, radiolucent, multiloculated cystic lesion, with a characteristic “soap bubble-like” appearance. Thinning and expansion of the cortical plate with erosion through the cortex can be seen. The associated unerupted tooth may be displaced and resorption of the roots of adjacent teeth is common. The location of acanthomatous ameloblastoma is considered to be rare and uncommon and more commonly appearing in the mandible (81%) than the maxilla (19%). In maxilla, the lesion found most were in the molar area (47%), antrum, and nasal floor (33%). Of the many types encountered, acanthomatous ameloblastoma is a very rare variant. The histology of acanthomatous type shows central squamous cell differential with keratin formation. Few authors quoted that formation of squamous metaplasia may be due to chronic irritation of calculus and oral sepsis. It was reported that acanthomatous ameloblastoma usually seen in older individual rather than younger ones, whereas in our case it is a young male patient [14].
In some studies it was observed that acanthomatous ameloblastoma if left untreated can develop into an invading squamous cell carcinoma. It is important to note in these circumstances that metaplasia of the odontogenic epithelium toward the squamous cell type in Acanthomatous ameloblastoma can simulate the appearance of both a squamous cell carcinoma and a basal cell carcinoma. Although histological features of acanthomatous ameloblastoma are different, it is now believed to be identical to the other types of ameloblastoma with no special extensive local infiltration and bone destruction or risk of recurrence. There are controversies about the biological behavior of Acanthomatous ameloblastoma; some authors believe that it is locally aggressive and frequently invades the alveolar bone or recurs after marginal surgical excision and some others believe that there is no difference among the various subtypes of ameloblastoma [15]. Thus, the study of molecular mechanisms of cell proliferation can be helpful to predict the aggressiveness of ameloblastoma and especially p16 (cyclin-dependent kinase inhibitor) which is a tumoral suppressor protein encoded by CDKN2A gene. A high score in immune expression of the p16 protein may indicate lower aggressiveness and a lower rate of recurrence [16].
The criteria for treating ameloblastoma are based on an individual patient's situation and the best judgment of a surgeon. The surgery should be planed keeping the histology type, clinical picture, tumor size, and age of the patient in mind. The surgical margin should extend 1.5–2 cm beyond the radiological limit, in order to ensure all the ‘micro cysts’ and ‘daughter cysts’ are removed. In our case also marginal clearance of 2 cm was achieved as histopathology of specimen revealed it to be acanthomatous variety.
Mandibular reconstruction of large defect can be planned with microvascular surgery using donor site from fibula, iliac crest, scapula and radial forearm [17]. In our case as well, tumour was treated with hemi-mandibulectomy as it was quite an extensive lesion. Hemimandibulectomy, simultaneously with reconstruction using iliac crest bone reduces the morbidity while retaining the aesthetics of the patient.
Conclusion
Ameloblastoma is the most commonly occurring odontogenic tumour in the mandible, in the middle age group. The differential diagnosis such as odontogenic keratocyst, odontogenic myxoma, and central giant cell granuloma has similar clinical picture but different radiographic appearance and has to rule out. The best treatment of ameloblastoma is aggressive enbloc resection with simultaneous reconstruction. The key points we learnt are
• Ameloblastoma being the most common should always be considered first in the list of differential diagnosis for any swelling in the mandibular posterior region in the middle age group.
• Conventional radiographs are sufficient for small lesions but large lesions require advanced imaging such as CT for better surgical management of the lesion.
• High recurrence rates are seen Multilocular/solid ameloblastoma among all types of ameloblastoma. Therefore wide resection of the lesion with a safety margin of healthy bone should be practiced in surgery.
• Simultaneous reconstruction should be planned after resection in order to restore the aesthetics of the patient as well as function of the jaw.
References
- Kahairi A, Ahmad RL, Wan Islah L, et al. Management of large mandibular ameloblastoma–a case report and literature reviews. Arch Orofac Sci 2008; 3:52-55.
- Giraddi GB, Bimleshwar SC, Singh C, et al. Ameloblastoma—series of 7 treated cases—and review of literature. Arch Orofac Sci 2011; 1:152-55.
- Vohra FA, Hussain M, Mudassir MS. Ameloblastomas and their management: A review. Pak J Surg 2009; 14:136-42.
- Pizer ME, Page DG, Svirsky JA. Thirteen-year follow-up of large recurrent unicystic ameloblastoma of the mandible in a 15-year-old boy. J Oral Maxillofac Surg 2002; 60:211-215.
- Churchill HR. Histological differentiation between certain dentigerous cysts and ameloblastoma. Dent Cosmos 1934; 76:1173-1178.
- Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumours. A commentary on the second edition. Cancer 1992; 70:2988-2994.
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer 1995; 31:86-99.
- Singh A, Shaikh S, Samadi FM, et al. Maxillary unicystic ameloblastoma: A review of the literature. J Maxillofac Surg 2011; 2:163.
- Gumgum S, Hosgoren B. Clinical and radiologic behavior of ameloblastoma in 4 cases. J Can Dent Assoc 2005; 71:481.
- Madiedo G, Choi H, Kleinman JG. Ameloblastoma of the maxilla with distant metastases and hypercalcemia. Am J Clin Path 1981; 75:585-591.
- Bansal M, Chaturvedi TP, Bansal R, et al. Acanthomatous ameloblastoma of anterior maxilla. J Indian Pedodontic Soc Prev Dent 2010; 28:209-211.
- Kahairi A, Ahmad RL, Wan Islah L, et al. Management of large mandibular ameloblastoma-A case report and literature reviews. Arch Orofac Sci 2008; 3:52-55.
- Singh G, Agarwal R, Kumar V, et al. A canthomatous ameloblastoma-a case report. J Int Oral Healt 2013; 5:54.
- Becelli R, Carboni A, Cerulli G, et al. Mandibular ameloblastoma: Analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofac Surg 2002; 13:395-400.
- Anneroth G, Heimdahl A, Wersall J. Acanthomatous ameloblastoma. Int J Oral Surg 1980; 9:231-236.
- Olimid DA, Florescu AM, Cernea D, et al. The evaluation of p16 and Ki67 immunoexpression in ameloblastomas. Rom J Morphol Embryol 2014; 55:363-367.
- Shirani G, Arshad M, Mohammadi F. Immediate reconstruction of a large mandibular defect of locally invasive benign lesions (a new method). J Craniofac Surg 2007; 18:1422-1428.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Shilpi Srivastava1*, Manisha Saxena2, Shiva Prasad Kyasanoor3, Swetha Meruva3 and Harini Gunda4
1BDS, General dental practitioner, Mahatma Gandhi dental college and hospital, Jaipur, India2MDS in Oral Medicine and Radiology, Founder of Shining Bright Academy and Consultant, India
3BDS, Kamineni Institute of Dental Sciences, Telangana, India
4BDS, Government Dental College and Hospital, Hyderabad, India
Citation: Shilpi Srivastava, Manisha Saxena, Shiva Prasad Kyasanoor, Swetha Meruva, Harini Gunda, Rare Variant of Ameloblastoma- A Case Report of Acanthomatous Ameloblastoma, J Res Med Dent Sci, 2023, 11(4): 12-16.
Received: 29-Mar-2023, Manuscript No. jrmds-23-92146; Accepted: 01-Apr-2023, Pre QC No. jrmds-23-92146; Editor assigned: 01-Apr-2023, Pre QC No. jrmds-23-92146; Reviewed: 15-Apr-2023, QC No. jrmds-23-92146; Revised: 22-Apr-2023, Manuscript No. jrmds-23-92146; Published: 29-Apr-2023
