Review Article - (2023) Volume 11, Issue 8
Recurrent Aphthous Stomatitis: A Prevalent Condition in Growing Indian Population
Palak Bhaiyya1*, Aarti Panchbhai2, Pavan Bajaj2 and Gunjan Taori1
*Correspondence: Dr. Palak Bhaiyya, Department of Oral Medicine and Radiology, Datta Meghe Institute of Medical Sciences, Maharashtra, India, Email:
Abstract
Recurrent aphthous stomatitis also known as aphthous ulcer, aphthae or canker sores. These are the repeatedly occurring ulcers on oral mucous membrane characterized by pain and inflammation. The specific cause of its occurrence is unknown but various factors play a major role in it such as bacterial infection, Immunologic abnormalities, Iron, vitamin B12 and folic acid deficiency, genetic factors, etc. Other risk factors playing role are trauma, allergic reaction, psychic factors, systemic diseases, tobacco, endocrine factors and drugs. There are 3 types of recurrent aphthous stomatitis, as minor ulcers, major ulcers and herpetiform ulcers being the most prevalent. Most frequently they are characterized by many tiny round or oval mucosal ulcers having constricted edges, erythematous halos, yellow or grey floors. Minor form is seen in 80%, major RAS in 10% and herpetiform in 1 to 10% of the total cases. Rectification of defects like iron, folate, vitamin B12 or a combination of these elements helps in healing of ulcers. There is no specific therapy for healing of ulcers but avoiding meals like acidic food, hot beverages, etc. is proved helpful. Topical and systemic medication help to ease the pain and to avoid discomfort while eating. The present review article will provide insight into etiology and risk factors for occurrence of recurrent aphthous stomatitis.
Keywords
Recurrent aphthous ulcer, Aphthae, Canker sores, Stomatitis
Introduction
The literal meaning of recurrent aphthous stomatitis is:
• Recurrent: Occurring repeatedly
• Aphthous: Small ulcers occurring in groups
• Stomatitis: Inflammation of oral mucous membrane
Recurrent Aphthous Stomatitis (RAS) is a prevalent condition marked by the recurrence of benign, noninfectious mouth ulcers seen in healthy people. Canker sore is an informal word that is commonly used in USA. The aetiology is unknown yet it includes immune response by T lymphocytes that can be caused by a range of variables such as nutrient inadequacy, local injury, stress, endocrinal effects, hypersensitivity, hereditary changes, particular foods, lack of water consumption and certain dietary contents [1].
RAS is characterized by painful, recurring multiple ulceration of oral mucosa. Recurrent aphthous stomatitis can affect up to 7 out of 10 persons at a certain point in their lives. The most frequent ulcerative lesions of the oral cavity are RAS. Specific cause of these ulceration is not known, however various variables have a role in its progression. Local factors such as trauma, dysbiosis of the oral microbiota, hematinic deficiencies (iron, folic acid or vitamin B12), immunological variables and psychosocial stress are among them. Additionally, ulcers may be present due to a hereditary susceptibility. In up to 40% of patients, there is a positive family history. When both parents have recurrent aphthous stomatitis, the odds of recurring aphthous stomatitis is 90%, but only 20% when neither parent has recurrent aphthous stomatitis. The identification of harmful genetic variables has resulted from the detection of particular family patterns of recurrent aphthous stomatitis. Recently, genetic variables, especially genetic variants associated to immune system function have been investigated to see if they have a role in the development of mouth ulcers [2].
Literature Review
Etiology
Bacterial infection: The pathophysiology of RAS has been linked to a number of microorganisms. In the many investigations that have been published, some contradictory conclusions have been reported [3].
Oral streptococci and RAS: Streptococci in the mouth have long been thought to be microbial agents in the RAS pathogenesis. The L form of hemolytic streptococci, it has been suggested, S. sanguis; later identified as S. mitis was the disease's etiological factor [4].
Helicobacter pylori and RAS: Among the species involved in the etiopathogenesis of these ulcers has been identified as Helicobacter pylori. Helicobacter pylori is seen in significant concentrations in bacterial biofilm on tooth. Porter et al. investigated the levels of IgG antibodies against this bacteria in individuals with oral ulceration and found incidence of seropositivity was not significantly altered [5].
Immunologic abnormalities: HLA types linked to aphthae include HLA-B12, HLA-B51, HLA-Cw7, HLA-A2, HLA-A11 and HLA-DR2. Systemic immuno-dysregulation, like cyclic neutropenia, HIV infection, can also cause aphthous-like ulceration. More acute oral lesions occur during this in cyclic neutropenia and healing is linked to the resolution of the underlying neutropenia. RAS in HIV may be linked to upsurge in the proportion of cytotoxic T cells produced by decrease in the number of T helper cells [6].
Iron, vitamin B12, folic acid deficiency: Nutrient deficits are far more frequent among RAS patients than in the general population, according to several additional studies. In a study of 330 individuals with recurrent aphthous stomatitis, researchers discovered that 47 (14.2%) were low in iron, folate, vitamin B12 or a combination of these elements. Another research found that 28.2% of 60 individuals were lacking in thiamin, riboflavin, or pyridoxine. The majority of the patients had full remission when their deficits were rectified. In those with RAS, lower dietary intake of folate and vitamin B12 is frequent, and therapy with 1000 mcg per day has been demonstrated to help independent of blood vitamin B12 levels [7].
Genetic history: A hereditary tendency for occurrence of RAS is strongly suggested, since around forty percent of individuals have genes of this condition, they evolve these lesions early which are at higher risk. Some cases show a hereditary trend. In identical twins, there is a significant correlation of RAS. RAS has been linked to particular HLA haplotypes [8].
Others: Mouth ulcers are also seen in some serious conditions like
• Cardiac diseases
• HIV
• AIDS
• Inflammatory bowel disease
• Diabetes mellitus
• Behcet’s disease
Risk factors
Trauma: Local anaesthetics, point tip teeth, dentical procedures, orthodontic treatments, tooth brush injuries to oral mucosa may lead to occurrence of ulcers. In 1981, Wray et al. postulated that mechanical damage may help identify and analyze individuals who are prone to aphthous stomatitis [9].
Allergic reactions: For ingested and many inhaled allergens, the mouth cavity is certainly the initial point of interaction. The histological appearance of the lesions, as well as the link between RAU and elevated blood antibodies to food antigens and atopy, imply an allergic response. Mast cell degranulation is crucial in the development of the aphthous lesion. An elimination diet is demonstrated to be operative in the treatment of a wide range of illness. The allergic agent does not always have to be a food [10].
Psychic factors: Psycological factors include stress. It is suggested causing harm to oral mucous membrane by habitual behavior such as lip or cheek biting, which leads to ulcers. There has recently been no relation discovered between stress levels and the intensity of aphthous events, indicating that mental pressure may act as an initiating or moderating factor rather than a causative factor in these individuals [11].
Endocrine conditions: Endocrine conditions include hormonal changes. There are conflicting studies on the link between endocrinal imbalance in female and RAS. Ulcers are linked to menstruation in studies. In 1992, Mc Cartan et al. found no link between ulcers and menstural cycle [12].
Systemic diseases: Ulceration resembling aphthous ulceration can arise as a result of a variety of systemic diseases. Although these lesions are morphologically and histologically comparable to aphthous stomatitis ulcers, some sources do not regard this form of oral ulceration to be real aphthous stomatitis. Oral ulcers, vaginal ulcers, anterior uveitis are all symptoms of Behcet's illness. Aphthous-like ulceration is the most common symptom of Behcet's illness, although it is frequently more critical than RAS without systemic aetiology. In 25-75 percent of patients, aphthous-like ulcers is the earliest symptom of the illness [13].
Tobacco: A number of studies have found a link connecting smoking and tobacco chewing with RAS. Elevated levels of keratinization of mucosa may be one possible cause. Nicotine is a defending feature because it enhances synthesis of adrenal hormones via hypothalamus adrenal axis and inhibits the production of TNF, IL1 and IL6. For individuals who develop RAS after quitting smoking, nicotine replacement therapy is considered a therapeutic option [14].
Drug: ACE inhibitor captopril, Au salts, phenindione, phenobarbital and NaClO are all linked to progress in RAU. NSAIDS induce ulcers in the same way as RAS does [15].
Mucosal barrier: In aphthous stomatitis, the thickness of the mucosa may play a role. Ulcers usually occur on the mouth's thinner, non-keratinizing mucosal surfaces. Factors that reduce mucosa thickness increase the frequency of incidence, whereas factors that improve mucosa thickness correspond with lower ulceration. Local trauma has also been linked to aphthous stomatitis, and trauma has been shown to weaken the mucosal barrier. Injury of local anesthetic injections in oral cavity, while doing other dental procedures, as well as injury from point tip surface in oral cavity.
Discussion
Classification
Recurrent aphthous minor/canker sore: This is the most prevalent symptom of the condition, accounting for 70% to 85% in total. It can be seen like little spherical lesions encircled by an erythematous halo, covered by a gray-white pseudo membrane. Each minor RAS episode generally results in the formation of 1-5 ulcers with a diameter not more than one cm. These episodes are selflimiting, lasting 4-14 days and leaving no scars.
Recurrent aphthous major/sutton’s disease: This is one of the serious form of disorders, accounting for 10% of all of the cases. Ulcers bigger than one cm in diameter arise on soft palate, lips, throat in this subtype. Lesions can last for up to 6 weeks and leave scars.
Recurrent herpetiform ulcers: Recurrent breakouts of tiny, deep and painful ulcers define herpetiform ulcers, which accounting for 1%-10% of all of the cases. Up to 100 aphthae, each averaging 2 mm-3 mm in diameter, can grow at the same time, however it have tendency to mix to produce bigger ulcers having uneven shape. Among all the three clinical categories of the illness, this presentation is more common in women and in patients who are older.
Recurrent ulcers with behcets syndrome: Mouth ulcers, eye irritation, dermatitis and abscesses and genitalial blisters are all symptoms of the condition. Behcet's syndrome might be an autoimmune disorder in which the immune system erroneously attacks some of the body's own healthy cells. Environmental and genetic factors are likely to play a role.
Based on severity
Simple aphthosis: Simple aphthosis is characterised by ulcers that are smaller than 1 cm in diameter, develop one or two at a time and heal without therapy in 7 to 10 days without scarring.
Complex aphthosis: Ulcers in complicated aphthosis can be greater than 1 cm in diameter, appear in clusters or in a herpetiform pattern and take longer to heal, sometimes leaving scars (Figure 1).
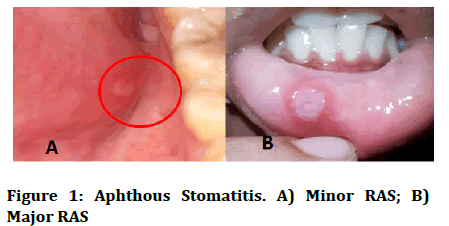
Figure 1: Aphthous Stomatitis. A) Minor RAS; B) Major RAS
Diagnosis
Characteristics: RAS is a common oral condition characterized by tiny, round or oval mucosal ulcers having constricted edges, erythematous halos, yellow or grey floors that first occur in the course of infancy or adolescence. Most of the disorders affecting the oral cavity might appear with identical clinical symptoms, making diagnosis challenging and sometimes delaying treatment.
Findings: A RAS diagnosis is made based on the patient's medical history and clinical findings. The ulcers might be one or many spherical, shallow, painful ulcers that repeat in episodes ranging from days to months. The most common kind of RAS is minor RAS, which affects roughly 80% of RAS patients. It can be seen like little spherical lesions encircled by an erythematous halo, covered by a gray-white pseudo membrane. It mainly affects nonkeratinized surfaces while it rarely affects keratinized tissue. Ulcers heal in 10 to 14 days on average. Major apthous is a severe type of RAS that affects roughly 10% of people with the disease; ulcers can be as big as 1 cm in diameter and appear on the lips, soft palate, and fauces. These can last up to 6 weeks. It usually appears after puberty, and can persist up to 20 years or more. RAS patients with herpetiformis ulcers account for roughly 1%-10% of all RAS patients. About hundred ulcers can exist at a given time but individual ulcers are just few mm in diameter, they tend to aggregate into enormous, uneven masses; the women are more likely to develop these. Despite its name, no evidence of a link to the herpesvirus has been discovered.
Histopathology: The appearance of histopathology is not diagnostic. A fibrinous membrane covers a core ulcer zone in early lesions. Inflammatory infiltration comprised of lymphocytes, histiocytes and neutrophils is present in connective tissue deep to the ulcer. The ulcer's epithelium has spongiosis and the basal third has a large number of mononuclear cells. Lymphocytes and histiocytes can also be seen in the connective tissue surrounding deeper blood vessels near the ulcer, which is called "perivascular cuffing" histologically.
Treatment
Avoiding risk factors: The great majorities of aphthous stomatitis patients have minimal symptoms and do not require treatment. During an episode of ulceration, modest dietary modifications like shunning hot and acidic meals as well as beverages can typically make the discomfort bearable. A variety of topical and systemic treatments have been offered, with slight or no confirmation of effectiveness when officially evaluated. Several outcomes of therapies might be due to a placebo effect. Treatment aims to ease discomfort, improve healing and minimize the frequency of ulceration episodes, although no therapy is curative.
Tropical treatment: Corticosteroids, cyclosporine, retinoids, antimicrobials and anesthetics may be used for topical therapy. The topical corticosteroids are used to minimize the local inflammation that causes ulceration. Dexamethasone (0.5 mg/5 mL), triamcinolone (0.1% gel), fluocinonide (0.05 % gel) and clobetasol are among them (0.05% gel). Clobetasol is a superpotent steroid of that produces improved outcomes.
Anesthetics like topical lidocaine and benzocaine are both utilized for reliving the discomfort of RAS. Gelclair, sucralfate, bismuth subsalicylate, and 2-octyl cyanoacrylate among other occlusive and bio adherent agents, have been effectively utilized in RAS treatment as it form a preventive layer which covers open and overstimulated nerve terminals.
Systemic treatment: Progestogen or modified oral contraceptive can be proved helpful in women whose ulcers are linked to their menstruation or oral contraceptives. Nicotine replacement treatment has also been documented for persons who have acquired mouth ulcers after quitting smoking. Resuming smoking does not generally improve the situation. Avoiding rough or sharp foods along with care of teeth while cleaning can help to minimize trauma. If sodium lauryl sulphate is the cause, avoiding goods that contain this ingredient may be beneficial in preventing recurrence in some people. Likewise, patch testing might reveal hypersensitivity reaction to specific food product is held responsible so the intake should be adjusted appropriately. If deficiency states are discovered during the research, correcting the deficit may result in the ulceration disappearing. Vitamin B12 supplementation, for example, has been shown to reduce the risk of recurrence in certain people.
Others: Many other treatment modalities have been mentioned in the literature. Although clinical removal of aphthae is documented, it is an inefficient and unsuccessful therapy. The chemical cauterant silver nitrate has also been utilized. Apart from the abovementioned mainstream techniques, there are plenty of other untested therapies varying from herbal remedies to unconventional cures, for example aloe vera, Myrtus communis, Rosa damascena, potassium alum, zinc sulphate, omega-3, nicotine, polio virus vaccine and prostaglandin E2. At last, dexamethasone elixirhas been demonstrated to be highly helpful against both pre-sores and existing sores.
Conclusion
Recurrent aphthous stomatitis is a prevalent condition affecting oral mucosa although there can be other causes for recurring ulcers in the oral cavity. It is considered as non-infectious stomatitis. The specific cause of its occurrence is unknown but various factors play a major role in it such as bacterial infection, immunologic abnormalities, iron, vitamin B12 and folic acid deficiency and genetic factors. Diagnosis is mostly and reliably based on the clinical appearance. The most important diagnostic feature is a history of recurrent, self-healing ulcers at fairly regular intervals. A systemic cause is more likely in adults who suddenly develop recurrent oral ulceration with no prior history. Appropriate knowledge of probable cause and contributory risk factors may help to treat the apthous stomatitis.
References
- Rivera C. Essentials of recurrent aphthous stomatitis. Biomed Rep 2019; 11:47-50.
- Akintoye SO, Greenberg MS. Recurrent aphthous stomatitis. Dent Clin North Am 2005; 49:31-47.
[Crossref] [Google Scholar] [PubMed]
- Slebioda Z, Szponar E, Kowalska A. Recurrent aphthous stomatitis: Genetic aspects of etiology. Adv Dermatol Allergol/Postepy Dermatol Alergol 2013; 30:96-102.
[Crossref] [Google Scholar] [PubMed]
- Dudding T, Haworth S, Lind PA, et al. Genome wide analysis for mouth ulcers identifies associations at immune regulatory loci. Natur Comm 2019; 10:1052.
[Crossref] [Google Scholar] [PubMed]
- Leimola‐Virtanen R, Happonen RP, Syrjanen S. Cytomegalovirus (CMV) and Helicobacter pylori (HP) found in oral mucosal ulcers. J Oral Pathol Med 1995; 24:14-17.
[Crossref] [Google Scholar] [PubMed]
- Porter SR, Barker GR, Scully C, et al. Serum IgG antibodies to Helicobacter pylori in patients with recurrent aphthous stomatitis and other oral disorders. Oral Surger Oral Medi Oral Pathol Oral Radiol Endodontol 1997; 83:325-328.
[Crossref] [Google Scholar] [PubMed]
- Preeti L, Magesh KT, Rajkumar K, et al. Recurrent aphthous stomatitis. J Oral Maxillofacial Pathol 2011; 15:252.
[Crossref] [Google Scholar] [PubMed]
- Zhou Y, Chen Q, Meng W, et al. Evaluation of penicillin G potassium troches in the treatment of minor recurrent aphthous ulceration in a Chinese cohort: A randomized, double-blinded, placebo and no-treatment–controlled, multicenter clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2010; 109:561-566.
[Crossref] [Google Scholar] [PubMed]
- Meng W, Dong Y, Liu J, et al. A clinical evaluation of amlexanox oral adhesive pellicles in the treatment of recurrent aphthous stomatitis and comparison with amlexanox oral tablets: A randomized, placebo controlled, blinded, multicenter clinical trial. Trial 2009; 10:1-7.
[Crossref] [Google Scholar] [PubMed]
- Liang MW, Neoh CY. Oral aphthosis: Management gaps and recent advances. Ann Acad Med Singapore 2012; 41:463-470.
[Google Scholar] [PubMed]
- Scully C, Porter S. Oral mucosal disease: Recurrent aphthous stomatitis. Br J Oral Maxillofac Surg 2008; 46:198-206.
[Crossref] [Google Scholar] [PubMed]
- Gallo CD, Mimura MA, Sugaya NN. Psychological stress and recurrent aphthous stomatitis. Clinics 2009; 64:645-648.
[Crossref] [Google Scholar] [PubMed]
- McCartan BE, Sullivan A. The association of menstrual cycle, pregnancy, and menopause with recurrent oral aphthous stomatitis: A review and critique. Obstetr Gynecol 1992; 80:455-457.
[Google Scholar] [PubMed]
- Maged A, Abdel Moneim W. Prevalence of aphthous and aphthous like ulcers and their relation to precipitating factors among a sample of Egyptian population. Egypt Dent J 2017; 63:2377-2388.
- Gondivkar SM, Bhowate RR, Gadbail AR, et al. Development and validation of oral health‐related quality of life measure in oral submucous fibrosis. Oral Dis 2018; 24:1020-1028.
[Crossref] [Google Scholar] [PubMed]
Author Info
Palak Bhaiyya1*, Aarti Panchbhai2, Pavan Bajaj2 and Gunjan Taori1
1Department of Oral Medicine and Radiology, Datta Meghe Institute of Medical Sciences, Maharashtra, India2Department of Periodontics, Datta Meghe Institute of Medical Sciences, Maharashtra, India
Citation: Palak Bhaiyya, Aarti Panchbhai, Pavan Bajaj, Gunjan Taori, Recurrent Aphthous Stomatitis: A Prevalent Condition in Growing Indian Population, J Res Med Dent Sci, 2023, 11 (08): 053-057.
Received: 10-Dec-2021, Manuscript No. JRMDS-22-49445; , Pre QC No. JRMDS-22-49445 (PQ); Editor assigned: 15-Dec-2021, Pre QC No. JRMDS-22-49445 (PQ); Reviewed: 29-Dec-2022, QC No. JRMDS-22-49445; Revised: 19-Jul-2023, Manuscript No. JRMDS-22-49445 (R); Published: 16-Aug-2023
