Research - (2022) Volume 10, Issue 1
Regional Anesthesia for Ureteroscopy and Lithotripsy for Upper Ureteric and Solitary Pelvic CalculiâAn Experience at IGGGH & PGI Pondicherry
Hemanatha Kannan M1, Rajesh Kumar2* and Sudhakar K3
*Correspondence: Rajesh Kumar, DNB Resident Urology, IGGGH and PGI, Pondicherry, India, Email:
Abstract
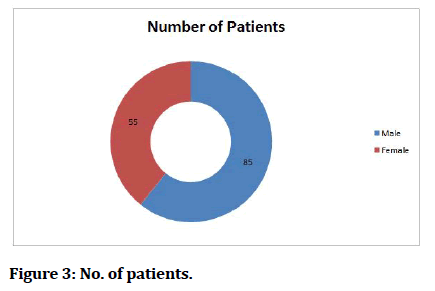
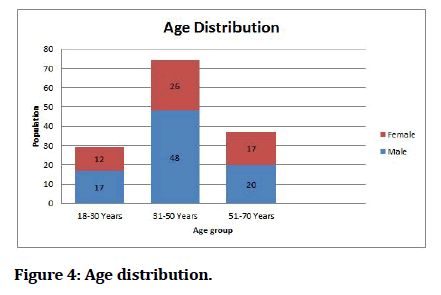
Objective: To estimate the limitations of regional anesthesia in ureterorenoscopy and lithotripsy for upper ureteric and solitary pelvic calculi at Indira Gandhi Government General Hospital and Post Graduate Institute (IGGGH & PGI), Puducherry. Patients and Methods: This prospective study was conducted at IGGGH and PGI, Pondicherry from December 2019 to September 2021. A total of 140 ASA-I patients, 85 male and 55 female, age ranging from 18 to 70 years, having upper ureteric or solitary pelvic calculi, were enrolled for the study. All received spinal anesthesia with 26G Quincke spinal needle at L3-4 interspace using 0.5% of (15mg) bupivacaine 3 ml and underwent ureterorenoscopy or insitu lithotripsy. Intraoperative and postoperative complications including hypotension, vomiting, plural effusion, pain on visual analgesia scale and duration of hospital stay were noted. Results: All patients had a successful motor block of hip and knee and sensory block up to T8. All with the exception of 4 patients achieved adequate anesthesia for the procedures. 4 patients had hypotension and 5 had bradycardia intraoperative. Vomiting occurred in 3 patients and PDPH in 3. All patients were shifted to ward 4 hours post operatively after confirmation of complete reversal of block and hemodynamic stability. The average stay of all patients in the hospital was 36-48 hours. Conclusions: Regional anesthesia can be safely used for lithotripsy of upper ureteric calculi and solitary renal pelvic calculi with decreased hospital stay and minimal post-operative and intra operative complications.
Keywords
Regional anesthesia, ureteric calculi, ureterorenoscopy, in situ lithotripsy
Introduction
Since 1980, ureterorenoscopy (URS) and in situ lithotripsy are routine urological procedures. In urology, URS has become a successful technique in the management of ureteral stones [1]. Use of advanced technology and modern equipment has not only increased the success rate of this procedure but also widened its indications [2]. Spinal Anesthesia has recently been widely used for urologic operations [3]. It permits early recognition of complications like perforation, and helps to prevent complications associated with delayed immobilization. The height of anesthesia can be tailored along the natural curve of spinal cord by adjusting the patient position after administration of drug [3].The aim of this study was to evaluate the usefulness and success of use of spinal anesthesia for upper urological procedures.
Materials and Methods
This study was conducted at Indira Gandhi Government General Hospital and Post Graduate Institute (IGGGH & PGI), Pondicherry from December 2019 to September 2021. 140 patients including 85 male and 55 female, ages ranging between 18 to 70 years, who were to undergo ureterorenoscopy or insitu lithotripsy for upper ureteric or solitary pelvic calculi and belonged to ASA 1 to III class were included in the study. Obese patients, any spinal deformity, mental disturbance and neurological disorder, and patients with multiple renal calculi or calculi accompanied with pelvic-ureteric junction calculi were excluded from the study. All patients were premedicated with Alprazolam 0.5 mg orally on the night before surgery. Drug therapy for concomitant medical problems was continued as deemed appropriate. All patients were preloaded with 1 litre of 0.9% NS fluid. All were monitored every 10 minutes for pulse, blood pressure, SpO2 and ECG.
Subarachnoid block was performed under all aseptic precautions with 26G Quincke Spinal needle at L3-4 interspace with patient in sitting position. Free flow of CSF was verified before and after the administration of 3 ml (15 mg) of 0.5% bupivacaine. The direction of needle aperture was cranial during the injection. Immediately after the injection, all patients were kept in 15 trendelenberg position for 3 minute and then returned to supine lithotomy position.
Hypotension (systolic BP <90 mmHg or 50 mmHg decrease from baseline) was treated with IV fluids and/or plasma expanders. Bradycardia (HR<50 bpm or decreased more than 20% from initial value) was treated with IV atropine 0.5mg. Other adverse effects like vomiting were recorded and treated accordingly. The level of sensory block defined by loss of sharp sensations using pinprick test was recorded at mid-clavicular line bilaterally. Motor block was assessed by testing the power of specific joints, L2 hip fexion and L3 knee extension. The sensory block was assessed at 5, 10, 20 and 30 minutes, end of operation and 2 hour after the injection. Pain was assessed by visual analog scale (VAS).
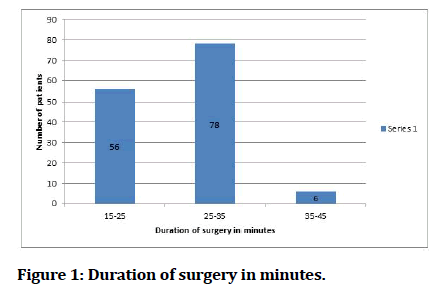
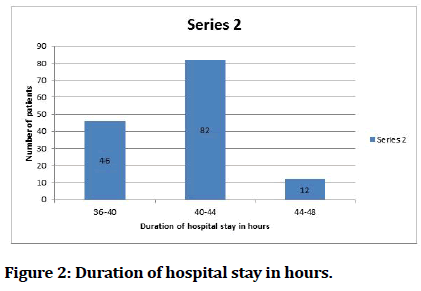
The average time for the procedure ranged 15-45 minutes. Postoperative pain was treated with inj. Tramadol 1 mg/kg IV body weight at the end of operation and inj Paracetamol 1000 mg IV 12 hourly. Headache was classified as Post spinal puncture headache (PDPH) if aggravated by erect or sitting position, relieved by lying flat, mainly occipital/frontal and increased on coughing, sneezing or lying flat. To prevent it, all patients were well hydrated with normal saline 0.9% pre operatively. Post Operatively foot end elevated, advised to lay supine and tab paracetamol 650 mg TDS. The patients were discharged from recovery when resolution of motor block was complete. The discharge criteria from the ward were stable vital signs, no nausea or vomiting, and no severe pain or bleeding and motor block completely recovered.
Results
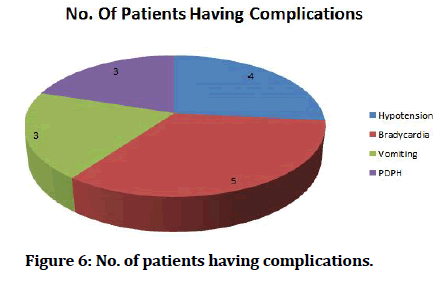
All patients had a successful motor block of hip and knee after 5 minutes. The average level sensory block achieved was T8. Adequate sensory block was established within 5-7 minutes after the injection. The time of injection to start of procedure was 10 -12 minutes. All patients with the exception of 4 achieved adequate anesthesia for the procedures. These 4 patients were supplemented with inj ketamine 2 mg/kg body weight to start the procedure. The duration of surgery ranged from 15 to 45 minutes. During the procedure, 2 anxious patients were given inj midazolam 2 mg as anxiolytic. 4 patients had hypotension needing plasma expanders and vigorous fluid treatment. 5 patients had bradycardia intraoperatively which was treated with inj atropine 0.5mg IV.
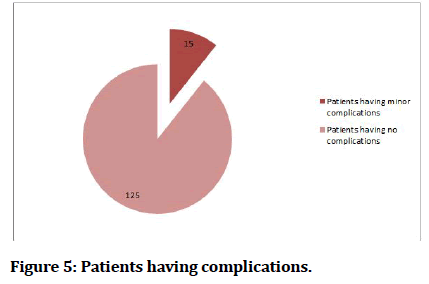
Complications like vomiting were encountered in 3 patients who were treated with an anti-emetic IV. The average time for total regression of block was 2.5 hours. 3 patients suffered from PDPH and were treated accordingly. All patients were shifted to ward 4 hours post operatively after confirmation of complete reversal of block and hemodynamic stability. The average stay of all patients in the hospital was 36-48 hours (Table 1 and Figures 1 to 6).
| No. of patients achieved motor block | 140 |
| No. of patients achieved sensory block | 136 |
| Anxious | 4 |
| No. of patients shifted toward within 4 hours | 138 |
| Patients kept for observation | 2 |
Table 1: Number of patients.
Figure 1: Duration of surgery in minutes.
Figure 2:Duration of hospital stay in hours.
Figure 3:No. of patients.
Figure 4:Age distribution.
Figure 5:Patients having complications.
Figure 6:No. of patients having complications.
Discussions
Regional anaesthesia is safest in the way, a small mass of drug, virtually devoid of systemic pharmacological effect, can produce profound, reproducible, surgical anesthesia [3]. The advantages include the ability to perform surgery on awake patient with decreased postoperative somnolence and less risk of pulmonary aspiration. Initially spinal anesthesia was used only for mid to lower uretric stones but with recent research on change of patient posture after injection of drug has helped using spinal anesthesia for upper abdominal surgeries including upper renal surgery [4,5]. Spinal anesthesia has been associated with minimal postoperative pain in these cases.
The treatment of kidney stones has changed significantly over the past two decades from primarily open surgical procedures to less invasive or completely non-invasive techniques [6]. URS is a vital procedure in the armamentarium of the modern day urologist for the management of ureteral and renal pathology [7]. Ureterorenoscopy has been most often used for the distal ureteral calculi. However advances in equipment have facilitated access to the proximal urinary tract and have broadened the indications for ureteroscopy [8]. The renal innervation is derived from T10 to L2 and, therefore, our level of anesthesia ranging up to a maximum of T8 provided successful pain-free state for almost all of our patients [9].
The change in posture immediately after the injection helped in achieving the adequate level of anesthesia. The natural curve of spinal cord not only helps us determine the approximate level of block achieved but also serves as a protection against the respiratory distress that might occur due to higher up spread of the drug [10]. Several studies have been previously done to study the effect of patient positioning on spinal anesthesia using hyperbaric local anaesthetic [10]. This effect of posture on the spread of local anesthetic has been in spinal anesthesia for intra renal surgery [11]. Since all patients were preloaded with 1 litre of fluid, intra operative hypotension was minimal and easily manageable. This finding is supported by Corke et al. in their study who proposed that the hypotensive episodes after spinal anesthesia are shorter and easier to treat if the patients are pre-loaded with 1 litre 0.9% normal saline or more of pre-anesthetic fluid [12-14]. Postoperative complications like PDPH were almost negligible in our study due to the use of 26G spinal needle reducing to minimum the leak of spinal fluid from dural puncture [15,16]. The use of fine needle in conjunction with the intravenous administration of fluids, rest, elevation of foot end of bed reduced the spinal headache to minimal. All patients were comfortable with the procedure as they remained pain-free intra and post operatively and were satisfied with the outcome. Since they were shown their stone being fragmented and removed on endovision camera monitor, it advanced their confidence in their stone management. This resulted in few if any postoperative complaints and reduced hospital stay [17,18].
Conclusion
We used regional anesthesia safely for insitu lithotripsy of upper ureteric calculi and solitary renal pelvic calculi with decreased hospital stay and minimal postoperative complications which can be easily managed.
References
- Anagnostou T, Tolley D. Management of ureteric stones. Eur Urol 2004; 45:714-721.
- Lotan Y, Gettman MT, Roehrborn CG, et al. Management of ureteral calculi: A cost comparison and decision making analysis. J Urol 2002; 167:1621-1629.
- Aitkenhead AR, Rowbothan DJ, Smith G. Textbook of Anaesthesia. 4th Edn. Edinburgh: Churchill Livingstone 2001; 555-75.
- Tobias JD, Flannagan J, Brock J, et al. Neonatal regional anesthesia: Alternative to general anesthesia for urologic surgery. Urology 1993; 41:362-365.
- Akhter MS, Hameed F, Akhtar FK. Ureteroscopy: New therapeutic indications. Biomedica 2000; 16:66-70.
- Cybulski PA, Joo H, Honey RJ. Ureteroscopy: anesthetic considerations. Urol Clin 2004; 31:43-47.
- Hollenbeck BK, Schuster TG, Faerber GJ, et al. Comparison of outcomes of ureteroscopy for ureteral calculi located above and below the pelvic brim. Urology 2001; 58:351-355.
- Morgan GE, Mikhail MS, Murray MJ, et al. Clinical anesthesiology. New York: Lange Medical Books/McGraw-Hill 2006.
- Veering BT, Immink Speet TT, Burm AG, et al. Spinal anaesthesia with 0.5% hyperbaric bupivacaine in elderly patients: Effects of duration spent in the sitting position. Br J Anaesth 2001; 87:738-742.
- Povey HM, Olsen PA, Pihl H. Spinal analgesia with hyperbaric 0.5% bupivacaine: Effects of different patient positions. Acta Anaesthesiol Scand 1987; 31:616-9.
- Tzovaras G, Pratsas K, Georgopoulou S, et al. Laparoscopic cholecystectomy using spinal anaesthesia. Br J Anaesth 2007; 99:744-745.
- Corke BC, Datta S, Ostheimer GW, et al. Spinal anaesthesia for caesarean section: The influence of hypotension on neonatal outcome. Anaesthesia 1982; 37:658-662.
- Jackson R, Reid JA, Thorburn J. Volume preloading is not essential to prevent spinal-induced hypotension at caesarean section. Br J Anaesth 1995; 75:262-265.
- Wright RG, Scnider SM. Hypotension and regional anaesthesia. In: Schnider SM, Leinson G. Anaesthesia for Obstetrics, 2nd Edn. Baltimore: William & Wilkins 1987; 293-9
- Ready LB, Cuplin S, Haschke RH, et al. Spinal needle determinants of rate of transdural fluid leak. Anesth Analg 1989; 69:457-460.
- Rasmussen BS, Blom L, Hansen P, et al. Postspinal headache in young and elderly patients: Two randomised, double blind studies that compare 20 and 25 gauge needles. Anaesthesia 1989; 44:571-573.
- Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trials. Br Med J 2000; 321:1493.
- Grass JA. The role of epidural anesthesia and analgesia in postoperative outcome. Anesthesiol Clin 2000; 18:407-428.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Hemanatha Kannan M1, Rajesh Kumar2* and Sudhakar K3
1FCA Consultant Cardiac Anesthetist, IGGGH & PGI, Pondicherry, India2DNB Resident Urology, IGGGH and PGI, Pondicherry, India
3MCH Consultant Urologist, IGGGH and PGI, Pondicherry, India
Citation: Hemanatha Kannan Regional Anesthesia for Ureteroscopy and Lithotripsy for Upper Ureteric and Solitary Pelvic Calculiâ??An Experience at IGGGH & PGI Pondicherry, J Res Med Dent Sci, 2022, 10(1): 371-374
Received: 23-Dec-2021, Manuscript No. Jrmds-21-45361; , Pre QC No. Jrmds-21-45361; Editor assigned: 27-Dec-2021, Pre QC No. Jrmds-21-45361; Reviewed: 10-Jan-2022, QC No. Jrmds-21-45361; Revised: 13-Jan-2022, Manuscript No. Jrmds-21-45361 (R); Published: 20-Jan-2022