Review Article - (2022) Volume 10, Issue 8
Rehabilitation of Patients Post COVID-19
Swaroopa Chakole* and Ananya Chaudhary
*Correspondence: Swaroopa Chakole, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi Meghe, Wardha, India, Email:
Abstract
Coronavirus has emerged as a pandemic that leads to acute phase symptoms followed by a sequalae of events. Patients infected with this virus who are discharged from the hospital should undergo outpatient pulmonary rehabilitation as well as rehabilitation for the psychological symptoms encountered by them. The purpose of pulmonary rehabilitation is to reduce symptoms of shortness of breath, avoid complications, as well as improve cardiopulmonary performance. Infection with the coronavirus illness 2019 (COVID-19) necessitates rehabilitation as many people who have suffered from this disease may be at a risk of long-term impairment and disability. The main concern of researchers studying about the disease is to find the correct time as to when start the rehabilitation programs. Some researchers are of the view that it should be initiated as soon as during the active stage of the disease while others are of the opinion that it should be given the patient becomes COVID negative or has recovered. We undertook a study of the most current papers due to the paucity of English-language recommendations on the rehabilitation of these individuals. In this literature review, we included randomized control trials, proposals, which were conducted using the major research database. Because of the complexities of the disease and fast spread of the SARS coronavirus, which leads to fast occupancy of critical care unit beds, patients with COVID-19 who have moderate indicators of the disease should be discharged as early as feasible. For these reasons, rehabilitation programs for these patients are required to assist them regain bodily, pulmonary features while also reducing depression and sadness, mainly in patients with multiple disease and those who live alone or in remote areas, in order to reclaim a high quality of life.Keywords
COVID-19, Rehabilitation, SARS coronavirus 2Introduction
Coronavirus disease 2019 is the ongoing contagious disease pandemic which is still at large from being over. It is affecting millions of people directly and indirectly and resulting in mass causalities. The first sighting of the pandemic disease of coronavirus was in December 2019 near Wuhan, Hubei Province, China, from where it swiftly spread throughout the world [1]. It also had shown phases in its occurrence, successive phases being more and more lethal. By 28th of July 2020, the reported cases were 16,465,707 [2]. Many countries are still reeling under the pressure and reporting a large a number of cases in spite of more than a year of the pandemic. Vaccination drive is in progress throughout the world. The first phase of the disease mainly affected the geriatric population, but the scientists claim the second phase will prove to be more fatal for the children and young adults. In terms of virology, epidemiology, and clinical therapy, SARSCoV-2 is becoming better understood. However, because of a lack of sufficient data, no medicines or vaccines to treat SARSCoV-2 have been formally licensed [3]. COVID-19 is an extremely communicable pulmonary infection that causes pulmonary, bodily, and cognitive dysfunction in afflicted people [4]. There is minimal evidence on the symptoms and indicators of the disease in patients with coronavirus because the pandemic is still underway [5]. Patients are secluded to avoid the dissemination of SARS-CoV-2 since coronavirus is very communicable. These results in a significant decrease in social connections, making patients feel lonely and alienated [6]. Patients in the Critical Care Unit (CCU) are bedridden for longer period of time. Patients lie in prone position for long periods of time, which results in post-ICU swallowing difficulties, muscle paralysis, myopathy, and neuropathy as a result of severe illness [7,8]. Some individuals have severe respiratory failure as a result of lung fibrosis, which necessitates pulmonary rehabilitation [9,10]. Rehabilitation of patients is required in acute phase, post-acute phase and in the long run. Rehabilitation is a type of treatment that aims to minimize impairment and improve functionality in people who have health problems and interact with their surroundings. The main goal of these retraining programs is to improve recovery and reduce disability or the experience thereof. The rehabilitation program focuses on the following aspects-physical impairments, cognitive impairments, and psychological impairment. Many ideas for pulmonary rehabilitation have been cited in this review, but these are not based on experiences. For these individuals, a rehabilitation program is deemed required, although the location is unknown. As a result, we examined a number of articles on COVID-19 rehabilitation programs to get an idea of the efficacy of these programs as well as the know the initiatives that the medical professionals may do to help patients in post-acute phase.
Literature Review
Methods
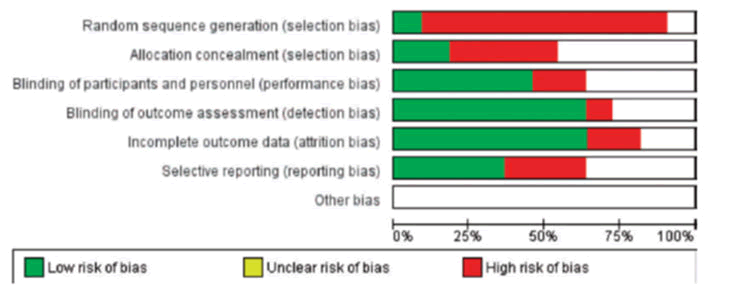
The titles and abstracts of the publications were originally screened. In a full-text review, items with ambiguous titles were assessed using the needed standards. Inclusion criteria were taken by 2 writers that were blinded to each other and the data that they collected from different studies came into the said criteria. To estimate the risk, the Cochrane Handbook recommendations were used. Selection bias, performance bias, detection bias, selective presentation of results, and other biases were separately assessed by 2 reviewers for the study quality (Figure 1).
Figure 1: Selection bias, performance bias, detection bias, selective presentation of results, and other biases were separately assessed by 2 reviewers for the study quality (bias risk).
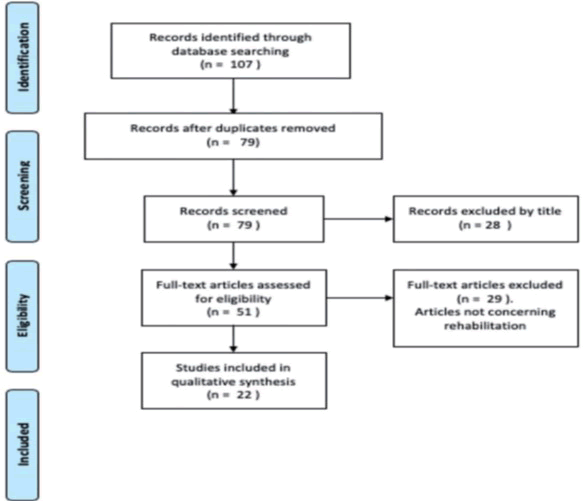
Disagreements in quality rating and differences in the retrieved data were addressed by a 3rd and 4th Author in order to establish a concord. The Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA-P) statement was followed when conducting this study (Figure 2). Informed consent and ethics approval were not obtained because this was a literature review [10].
Figure 2: Prism a flowchart.
Results
In the end, the review included a total of 22 papers (Figure 2). There is presently limited scientific knowledge to guide the rehabilitation in COVID-19 patients, partly due to the quick emergence of the epidemic. The conclusions of two articles produced by the same authors were comparable. Given the large number of patients in hospital needing critical care, it is expected that a huge number of COVID-19 survivors will require rehabilitation in the weeks and months [11]. As a result, many people believe that a customized rehabilitation program should be created according to each patient [12]. Presented a respiratory rehabilitation strategy which was built on the 4 S (simple, safe, satisfy, save) for patients who develop pneumonia by the new corona virus. The first to provide a recommendation based on professional judgments, distinguishing between patients with minor or serious illnesses and those who had been released was the Chinese Association of Rehabilitation Medicine according to Liu [13]. A respiratory rehabilitation program of 6 week may ameliorate pulmonary function, life quality, and nervousness in geriatric COVID-19 patients. The worry is whether or not to begin a rehabilitation program when the coronavirus is spreading at such a fast rate. According to Stam, early rehabilitation is a crucial step for the cure of sequelae in serious disease, for facilitating and improving slow recovery and patients' daily functioning, as well as for reducing the duration of respiratory support and hospital stays [14]. Early respiratory rehabilitation, which may be done at the bedside of the patient and maintained in a specialist rehabilitation facility, is recommended during the early phase, which is marked by breathing abnormalities and other respiratory symptoms [15,16]. Emphasis on early physical movement is critical for developing muscular strength, increasing mobility after discharge from the hospital, and enhancing life quality outside of the hospital. Early respiratory rehabilitation, on the other hand, is not advised by the Chinese Association of Rehabilitation Medicine and the Italian PRM Association since it is not well taken and results in fast desaturation [17]. According to the data in the regard, significant restructuring of facilities is necessary, with acute crises having priority over rehabilitation programs. For a variety of reasons, virtual OPD treatment may be given preference over face-to face contacts in the COVID-19 pandemic [18]. The gap can be bridged by the help of telemedicine and other online health care applications required during acute phase and rehabilitation services [19]. A tele rehabilitation system may be simply created utilizing a mix of technologies, with a physiotherapist observing patients while they complete rehabilitation activities for 20 minutes. Tele-rehabilitation, whether utilized in hospitals or in the community, might be a highly effective technique for addressing the social challenges connected with the current pandemic [20,21]. Huang presented a virtual as well as face to face multifaceted strategy for epidemic control, which showed little promise in the treatment of light disease and the detection of dangerous cases, by utilizing e-communication to allow for ongoing monitoring of patients' symptoms. Virtual care, on the other hand, has a number of drawbacks, including restricted scope for physical examination, non-availability of technology, technological faults, and the possibility for forced revelation of personal data. Furthermore, whether the patient can orient and interact in meetings without hesitance and speak properly is a major factor in this process [22].
Discussion
Coronavirus is a very communicative illness that causes patients to have pulmonary, bodily, and mental problems. In majority of COVID-19 infected patient's mild symptoms of fever, cough, dyspnoea is present, but the infection can have catastrophic consequences for a notable percentage of individuals, particularly those aged 65 or older and those who have comorbidities such as high blood pressure and diabetes mellitus. A significantly high number of patients needing hospitalization (20.3 percent) require ICU treatment, mainly due to multi organ failure or due to acute respiratory distress syndrome [23].
An efficient way to stop the dissemination of the extremely dangerous corona virus is quarantine. The majority of patients experience fever, exhaustion, and muscular discomfort, and they may be bedridden for a lengthy time. This causes a loss of muscular strength, which leads to inefficient sputum ejection and a considerable increase in the risk of DVT [24]. In ICU patients with extended non mobility and lengthy hours in prone position. Neuro muscular difficulties, severe muscle exhaustion, joint stiffness, swallowing difficulties, psychological difficulties, limited movement, severely degraded life quality and even quadriparesis can occur. Furthermore, prolonged cognitive impairment is frequently documented following CCU care, with pooled estimates indicating an increased frequency of anxiety (29 percent). Long term sequelae of physical, cognitive and emotional issues increase with the number of days stay in ICU. Fragile patients may start feeling depressed, alone, scared anxious and uncomfortable. Due to home isolation and shutdown of the outpatient clinics as a result, these patients are more likely to stop receiving therapy or have other psychiatric issues.
Respiratory rehabilitation aims to alleviate dyspnoea symptoms, relieve nervousness and anxiety, decrease problems, prevention and amelioration of non-functionality, decrease impairment, retain ability to the best degree possible, and enhance life quality in COVID-19 hospitalized patients. As of this writing, there is no proof on rehabilitation programs for COVID-19 patients. Majority of the articles that have been published have focused on the long-term effect of coronavirus on respiratory and neuromuscular system, they have also explained the anxiety and trauma of patients associated with the notion of being afflicted with the virus.
We had two points of view in this review the first one rooted on basic concepts of initial ventilatory recovery which also includes emotional help during the initial stage of corona virus, the 2nd point of view is rooted on the experiences of Italy and China, two nations who had to deal with the intensity of corona virus early in the pandemic and encountered a rehabilitation services deficit. Initial pulmonary restoration is not advised for seriously and gravely sick patients during times of probable and increasing illness, according to the findings of this analysis. After ruling out contraindications, the date for starting respiratory rehabilitation should be chosen, and all measures must be followed to prevent the spread of infection. In order to curtail the spread of the disease and to save resources of personal protection equipment, hospitalized patients should be made aware by videos, pamphlets, and monitor patients in rehabilitation. Respiratory rehabilitation may be taken by people who have survived from the virus and came back negative from it, for patients who are obese, who have multiple illnesses, and those with hypertension and diabetes require tailored respiratory rehabilitation services.
Patient's unique challenges should be looked into for a tailored program. Throughout the respiratory rehabilitation process, patients should be monitored using multiple tools. The coronavirus outbreak has had a huge effect on implications of health care all across the world, especially casualty, critical care, laboratories, and radiology departments. As the epidemic spreads, practically every aspect of health care will be affected, including post-acute care and rehabilitation. A combination of precision and professional pragmatism is required in this tough situation.
Patients who have appropriate caregiver support and who have mild symptoms and can be managed at home environment should be discharged early to make way for patients who are more in need. In order to satisfy the needs of patients who live alone or in remote areas, or who have comorbidities, a discharge rehabilitation program is needed. Patients discharged after COVID-19 infection may have poor fitness and breathing difficulties after exertion, as well as muscle wasting (including respiratory and trunk muscles) and psychological disorders such as post-traumatic stress disorder, according to current evidence in discharged patients with SARS and Middle East Respiratory Syndrome (MERS), as well as clinical experience with patients with ARDS. Patients with mild pulmonary dysfunction should be put through a rehabilitation program to assist them restore fitness while also lowering worry and despair.
Patients with COVID-19 who are critically sick and have crossed the pivotal point of the respiratory illness but still display signs of respiratory impairment should receive pulmonary retraining. The results of the first clinical study evaluating a pulmonary retraining program for patients recovering following coronavirus infection were recently reported. The results revealed an improved performance in pulmonary ability, life quality, and fear in a geriatric population, who completed the following pulmonary retraining program: breathing muscle strength and conditioning, coughing exercises, diaphragmatic training, stretching exercises, and home exercises, which were done twice a week for six weeks, once a day for ten minutes.
An inflow of patients with varied degrees of handicap will put post-acute care institutions under growing strain. For the sharing of information, open communication across rehabilitation centres is required, allowing centres that do not yet provide home-based program to swiftly learn from centres that have successfully implemented this approach. Telemedicine offers a lot of potential in this situation. It's a mechanism for linking people with health-care providers while staying within social-safety guidelines. Self-monitoring tools, field reports, fitness regimes, and emotional counselling may all be provided through digital health initiatives. People's interest in the management of critically ill patients in acute care settings has peaked so far.
Less emphasis has been paid to the ability of the post-acute medical care system to handle a large number of patients following coronavirus infection, that is, when patients transfer from the clinic to a long-term care facility or return home. As a result, rehabilitation will have to focus on screening program as a part to restore the normalcy gradually. Outpatient and home retraining will be required for a high percentage of COVID-19 patients. Establishing enough screening opportunities is critical. This can be done by a primary care physician or by a multi-disciplinary team that includes a physiatrist, physiotherapist, emotional counsellor, ICU specialist, and others. The study approach employed (including telemedicine and other e-medical techniques) is determined by the resources availability, the local medical system, and the availability of further retraining services.
COVID-19 patients will require a high number of OPD and home retraining therapies, and the detrimental effect coronavirus has had on health care units may make meeting patients' needs challenging. Hospital remodelling that reduces hospital rehabilitation services may result in longer wait times and the necessity to use a private office. Repurposing clinics, sporting facilities, or gyms to create temporary post-acute care facilities, when suitable, might quickly extend the available space for adaptive physical exercise.
Conclusion
COVID-19 is still evolving and mutating and lowering the guard would be disastrous in such scenario. Given the vast percentage of population infected with coronavirus around the world, and the constrained scientific understanding and proof currently offered, it is reasonable to expect that physiatrists and physiotherapists will become more engaged in the care of this population in order to improve respiratory abilities, bodily and cognitive performance, and a good life quality. Researches are still going on about the long-term impact of the disease and so one must be vigilant. Mental health is not a topic that can be dealt with at home it needs professional counselling. As the virus can only be eliminated by positive and coordinated efforts which are synchronized and time bound, planning ahead of time along with careful preparation will assist to mitigate the effects of this unexpected event.
References
- Cruz MP, Santos E, Cervantes MV, et al. COVID-19 a worldwide public health emergency. Revi Clin Esp 2021; 221:55-61.
- COVID E. Situation Update Worldwide, as of Week 2. 2021. Evolution of trends 198 in 14-day COVID-10 cases and death notification rates by country and continent or 199 region. 19.
- Li H, Zhou Y, Zhang M, et al. Updated approaches against SARS-CoV-2. Antimicrob agents and chemothe 2020; 64:483-520.
- Zhao HM, Xie YX, Wang C. Chinese Association of Rehabilitation Medicine; Respiratory Rehabilitation Committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation. Recommendations for respiratory rehabilitation in adults with coronavirus disease 2019. chin Med J 2020; 133:1595-6102.
- Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis 2020; 18.
- Xi ZJ, Zhi Z. In Recommendations for respiratory rehabilitation of COVID-19 in adults 2020.
- Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post-acute phase.'Instant paper from the field' on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med 2020; 56:323–326.
- Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Ame J Phy Med Rehab 2020; 99:470.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clinic Epidemiol 2009; 62:1-34.
- Boldrini P, Bernetti A, Fiore P, et al. Impact of COVID-19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine physicians' activities in Italy An official document of the Italian PRM Society (SIMFER). European J Phy Rehab Med 2020; 56:315-318.
- Yang F, Liu N, Hu JY, et al. Pulmonary rehabilitation guidelines in the principle of 4S for patients infected with 2019 novel coronavirus (2019-nCoV). Zhonghua jiehe he huxi zazhi 2020; 43:180-182.
- Liu K, Zhang W, Yang Y, et al. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract 2020; 39:101166.
- Stam HJ, Stucki G, Bickenbach J, et al. Covid-19 and Post Intensive Care Syndrome: A Call for Action. J Rehabil Med 2020; 52:00044.
- Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J physio 2020; 66:73-82.
- Mukaino M, Tatemoto T, Kumazawa N, et al. Staying active in isolation: telerehabilitation for individuals with the severe acute respiratory syndrome coronavirus 2 infection. Ame J Physical Med Rehab 2020; 99:478.
- Huang S, Xiao Y, Yan L, et al. Implications for online management: two cases with COVID-19. Telemedicine and e-Health. 2020; 26:487-494.
- Barker RE, Jones SE, Banya W, et al. The effects of a video intervention on posthospitalization pulmonary rehabilitation uptake. A randomized controlled trial. Ame J Resp Critical Care med 2020; 201:1517-1524.
- Brugliera L, Spina A, Castellazzi P, et al. Rehabilitation of COVID-19 patients. J Rehab Med 2020; 1-12.
- Lazzeri M, Lanza A, Bellini R, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis 2020; 90.
- Boldrini P, Kiekens C, Bargellesi S, et al. First impact on services and their preparation. 'Instant paper from the field' on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med 2020; 56:319-322.
- Chaturvedi SK. Covid-19, coronavirus and mental health rehabilitation at times of crisis. J Psychosoc Rehabil Ment Health. 2020; 7:1-2.
- McNeary L, Maltser S, Verduzco-Gutierrez M. Navigating coronavirus disease 2019 (COVID-19) in physiatry: a CAN report for inpatient rehabilitation facilities. PMR 2020; 12:512-515.
- Percy E, Luc JG, Vervoort D, et al. Post-discharge cardiac care in the era of coronavirus 2019: how should we prepare. Canadian J Cardiol 2020; 36:956-960.
- Chinese Association of Rehabilitation Medicine, Respiratory rehabilitation committee of Chinese Association of Rehabilitation Medicine, Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation. Recommendations for respiratory rehabilitation of COVID-19 in adults. Zhonghua Jie He He Hu Xi Za Zhi 2020; 43:E029.
Author Info
Swaroopa Chakole* and Ananya Chaudhary
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi Meghe, Wardha, IndiaCitation: Swaroopa Chakole, Ananya Chaudhary, Rehabilitation of Patients Post COVID-19, J Res Med Dent Sci, 2022, 10 (7): 000-000
Received: 26-May-2022, Manuscript No. JRMDS-22-49556; , Pre QC No. JRMDS-22-49556; Editor assigned: 30-May-2022, Pre QC No. JRMDS-22-49556; Reviewed: 13-Jun-2022, QC No. JRMDS-22-49556; Revised: 26-Jul-2022, Manuscript No. JRMDS-22-49556; Published: 04-Aug-2022