Research - (2022) Volume 10, Issue 11
Replacement and repair of direct restorations done by undergraduate and postgraduate students in Riyadh Elm University, Saudi Arabia. A Retrospective analysis
Khalid Fahad Alotaibi1* and Maha Mohammed Alotaibi2
*Correspondence: Khalid Fahad Alotaibi, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, Email:
Abstract
Objectives: Retrospective study aimed to investigate the number of direct restorations replaced and repaired, evaluate the reasons behind it, as well as compare between undergraduate and post graduate students in the dental hospital of Riyadh Elm University (REU). Methods: Patient records were retrospectively screened from the electronic data base system (DentoPlus) of REU hospital for restorations replaced and repaired in the past year. Patients that are >18 years old, had restorations that were repaired or replaced, and proper documentation was present were included in the study. A form with the information was filled. Data was analysed using the IBM-SPSS, version 25, Armonk, NY. Results: A total of 78,413 documented procedures dated form March 2017 till March 2020 were viewed by the examiners. A total of 2535 procedures (3.23%) were included in this study. Reasons for exclusion were restorations placed for the first time, procedures with improper documentation, or not approved by the instructor. Conclusion: Even though restorative procedures are the most preformed during any given clinical day at REU, the replacement/repair of restorations represents only around 3.23% out of all included restorative cases. Recurrent caries was the most mentioned cause of restoration failure by operators. Those failed restorations were seen mostly among female patients, and it was mostly observed in class II restorations. The decision making depends mainly on operator’s knowledge, and clinical skills in managing defected restorations. Clinical relevance: Our research emphasized the importance of proper documentation in order to make it efficient and have great success if faced with legal issues in the future. Also, proper documentation could lead to minimum invasive dentistry.
Keywords
Contagious disease, Oral hygiene, Questionnaire, Dental hospital
Introduction
Dental caries is an infectious‐contagious disease clarified as a public health problem. It is controlled by the individuals’ oral hygiene, bacterial colonization, saliva composition, and many more factors. The carious lesion is removed and replaced with a restoration. Direct restorative materials have been widely used in dental practice over the world in the past decades. The presence of carious lesion was found to be the most common indication for using direct restorations. One of the most routinely used materials now a days are composite resins [1]. Composite resin has been successfully used in both posterior stresses bearing area, and anterior esthetic areas, its use has increased significantly in the past 60 years due to the esthetic demands of patients [2,3]. The longevity of dental restorations is limited, prone to failure that is the reason re-treatment is indicated [4,5]. However, some research state that compliance with treatment protocols could prolong the life of the restoration, for up to 10 years and perform as well as amalgam [6,7]. These protocols include proper oral hygiene measures, steering clear of risk factors such as smoking, and beverage consumption, and reducing failure rate by treating bruxism, and xerostomia [7,8].
After placement of dental restorations, multiple structural changes and defects can be noticed. Management of defective restorations has been one of the most controversial topics in dentistry. Restoration failure can be related to the material used, the technical quality of the restoration, skills of the operator, and ultimately patient compliance [6,9]. Research states the main reason for failure of anterior restoration is fracture, and esthetics. Since appearance is affected, minor imperfections can compromise that, and restorations need to be redone [2]. Despite advancements done to composite resins, and restorative material, restoration replacement is one of the most common procedures in general practice. It constitutes 60% of the work performed in clinical practice, affecting both patient, and dentist causing enormous economic expense [2,8,10,11]. Replacement of some restorations is often easy to diagnose due to their failure. Defective restorations, and recurrent caries are the most common encounters [10,11]. Various studies have concluded secondary caries to be the most common cause of failure [6]. However, others are due to environmental concerns of mercury. Replacement of amalgam to composite resin fearing toxicity has increased in many countries, even in non-esthetic areas [8,10]. Studies have shown that failure of restorations could be due to different factors. In Saudi Arabia, Iqbal et al. in 2017, conducted a cross sectional study in Aljouf university and pointed out that the major causes of such failures are secondary caries, tooth sensitivity and overhang restorations [11]. Another study by Lempel et al. in 2015 found that composite restorations on posterior teeth are usually failed due to fracture of restoration and root canal treatment of the restored tooth [6]. Marginal discoloration of composite restoration is not always a sign of secondary caries in low to moderate risk patients [12]. However, in presence of clinical and radiographic pathological findings, some dentists would choose to keep the original restorations and repair them. For example, according to a questionnaire study done by Staxrud et al. in 2016, most of Norwegian dentists tend to repair composite restorations with various extent of damage by resin-based composite, and this finding was related to the age of dentist significantly [13]. A study by Brunton, et al. in 2017 found that education can play a major role in decision making as well as clinical experience [5]. After reviewing 401 papers on management and teaching of dental restoration repair, Kanzow, et al. in 2018 concluded that repair has been the most widely taught treatment in dental schools [14]. Another study by Nikolaos, et al. in 2012 has shown that Composite restorations can last for more than 8 years before they are indicated for replacement [15]. Repaired restorations on posterior teeth can last for more than 10 years [16]. A retrospective study for 15 years followup by van de Sande, et al. in 2019 showed that survival rates of composite repair of class III/V restorations were (64%-69%) [17]. In cases of high caries risk patients and history of missing dental appointments, repair of a defective restoration is contraindicated [1]. Replacement was chosen to be a treatment technique mostly for defective restorations with secondary caries [3]. Like repair, replacement has shown satisfactory results upon two-year follow-up [18]. Replacement is a more preferred option among dentists when the defective restoration is amalgam on a molar tooth [19]. A prospective study to measure the failures of repaired or replaced restorations found that if another treatment is needed after one-year, repaired restorations would require less aggressive procedures [20]. Repair and replacement of defective composite restorations have shown comparable results upon 15 years follow-up [2].
Aim of the study
The aim of this study is to:
Investigate, and evaluate the number and reasons for replacement of direct restorations done by undergraduate and post graduate students in dental hospital of Riyadh Elm University in the past 3 years.
Determine the association factors of replaced/repaired direct restorations.
Compare the number and reasons of replaced direct restorations of undergraduate with post graduate students in dental hospital of Riyadh Elm University in the past 3 years.
Methods
Patient records were retrospectively screened from the electronic data base system (DentoPlus) of REU hospital for restorations replaced and repaired in the past year. Patients that are >18 years old, had restorations that were repaired or replaced, with proper documentation were included in the study. A form with the information was filled. Data was analysed using the IBM-SPSS, version 25, Armonk, NY. Study was registered in Riyadh elm University Research center and approved with IRB number SRS/2020/34/225/221.
Data analysis
Data was analyzed using the Statistical Package for Social Sciences (SPSS, Chicago IL) version 22. Descriptive statistics was used to summarize the data. Categorical variables were expressed as proportions, and continuous variables expressed as the mean ± standard deviation (SD). The chi-square and independent t-tests were used to analyze categorical and continuous data, respectively. P value of <0.05 was considered significant.
Results
All the responses were entered into the statistical analysis software package (IBM-SPSS, version 25, Armonk; NY). Descriptive statistics of frequency distribution and percentages were calculated for the categorical variables. Cross-tabulation and chi-square analysis was applied to the data. A p value less than 0.05 was considered significant.
The data were obtained from patient’s files on REU dental clinic data base (DentoPlus).
A total of 78,413 documented procedures dated form March 2017 till March 2020 were viewed by the examiners. A total of 2535 procedures 3.23% were included in this study (2487 98% replacements and 45 repairs 2%).
First, in regards of patient data the average age was 35.4 years (with youngest being 18 years old and oldest being 74 years old). A total of 187 procedure (7.4%) of all replace/repair procedures were performed on a patient with a systematic disease. Diabetes mellitus was the most documented systemic disease by 64 cases 29.1%. Out of all replace/repair procedures, the procedures performed on female patients were consisting of 57% by 1437 cases and the male consisted of 43% by 1098 cases. There was statistical significance between the repair and replacement cases. Among the years, there was increase of procedures from 2017 till 2020, the repair cases were statistically significance (P.value =0.001) with an increase from 13.3% in 2017 to 82.2% in 2020 (Figure 1 and Table 1).
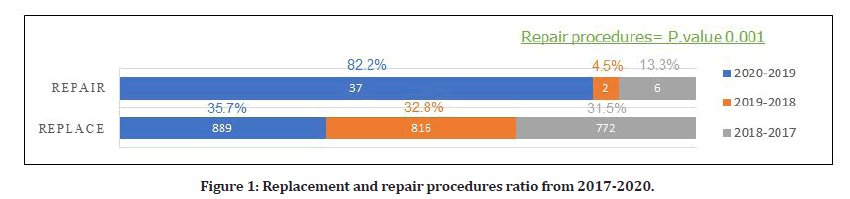
Figure 1: Replacement and repair procedures ratio from 2017-2020.
Second, in regards of operator related data, the total performed procedures was almost equally done between male and female operators. But the gender of operator was statistically significant (P.value =0.002) with higher tendency to repair by female operators by 73.3% than males 26.7% (Table 1).
| Variables | Replace | Repair | Chi Sq | Df | P | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Gender | Female | 1233 | 49.40% | 29 | 74.40% | 9.569 | 1.00% | 0.002 |
| Male | 1263 | 50.60% | 10 | 25.60% | ||||
| Level | Undergraduate | 1945 | 77.90% | 27 | 69.20% | 1.68 | 1.00% | 0.195 |
| Postgraduate | 551 | 22.10% | 12 | 30.80% | ||||
| Year | 2019-20 | 909 | 36.40% | 30 | 76.90% | 27.439 | 2.00% | <0.001 |
| 2018-19 | 813 | 32.60% | 3 | 7.70% | ||||
| 2017-18 | 774 | 31.00% | 6 | 15.40% | ||||
Table 1: Pearson chi-square tests for the relationship between gender, level of operator and year with repair and replacement.
Thirdly, the documented causes for the replace/repair procedures, the “recurrence of caries” was the most documented by 82% with 2077 procedures.
According to tooth type, premolars were the most repaired teeth by 46.1% with 18 cases, while molars experienced more replacement procedures by 47.7% with 1204 cases.
Defects to necessitate replacement/ repair were significantly affecting occlusal surfaces. Where most of old restorations were composite restorations by 85.2% in 2156 of the included cases. Moreover, the most used type of new restoration was also composite by 2500 case representing 98.6%.
Results also showed that recurrent caries was significant in relation to tooth type &tooth position with highest in molar teeth by 49.3% with 1024 cases by (P.value =0.042) and upper arch (P. value=0.00) by 59.5% with 1236 cases. Likewise, discoloration and esthetic showed significance with tooth position with highest in maxillary arch (P.value=0.000). Also, they showed significant in relation to tooth type with highest in anterior teeth (P.value=0.00). Overhang and open margins showed significance with tooth type with the highest occurrence in premolars by 41.4% and significance of (P.value =0.015) (Figure 2 and Table 2).
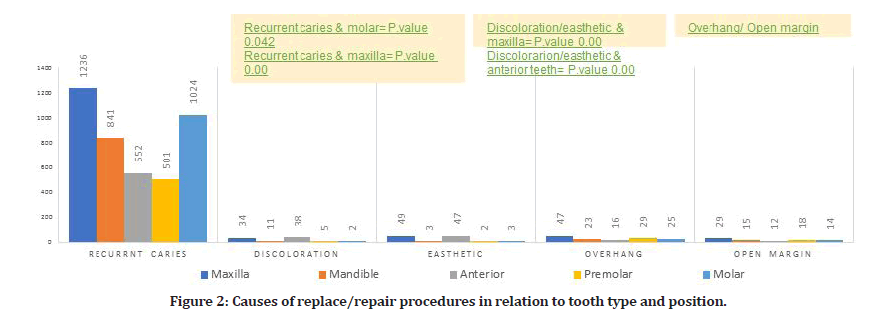
Figure 2: Causes of replace/repair procedures in relation to tooth type and position.
| Causes | Tooth Type | Tooth Position | Tooth Surface | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anterior | Premolar | Molar | Total | Maxillary | Mandible | Occlusal | Total | Mesial | Distal | Buccal/ Facial | Lingual/ Palatal | Incisal | ||
| Recurrent Caries | Chi-square | 4.031 | 12.328 | 4.132 | 22.530 | 32.833 | 0.905 | 34.781 | 3.769 | 8.158 | 3.814 | 12.481 | 1.535 | 13.207 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.045 | 0 | 0.042 | 0 | 0 | 0.341 | 0 | 0.052 | 0.004 | 0.051 | 0 | 0.215 | 0 | |
| Fracture | Chi-square | 1.189 | 1.058 | 0.432 | 3.646 | 4.107 | 0.844 | 1.369 | 1.152 | .646 | .801 | .081 | .647 | 17.325 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.275 | 0.304 | 0.511 | 0.162 | 0.043 | 0.358 | 242 | 283 | 0.422 | 0.371 | 0.776 | 0.421 | 0 | |
| Pain | Chi-square | 0 | 0.030 | 0.037 | 2.585 | 0.012 | 0.086 | 343 | 3.418 | 0.736 | 0.062 | 0.14 | 0.519 | 0.08 |
| df | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0 | 0.862 | 0.847 | 0.275 | 0.913 | 0.77 | 558 | 0.065 | 391 | 0.804 | 0.708 | 0.471 | 0.777 | |
| Sensitivity | Chi-square | 0.014 | 15.622 | 0.009 | 1.539 | 19.592 | 0 | 0.579 | 2.627 | 0.217 | 0.413 | 0.661 | 0.415 | 0.064 |
| df | 1 | 1 | 1 | 2 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.905 | 0 | 0.923 | 0.463 | 0 | 0 | 0.447 | 0.105 | 0.641 | 0.52 | 416 | 0.519 | 0.8 | |
| Discoloration | Chi-square | 0.565 | 0.152 | 0.019 | 71.734 | 0.414 | 0.238 | 62.159 | 4.402 | 2.022 | 0.262 | 1.285 | 399 | 15.768 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.452 | 0.696 | 0.892 | 0 | 520 | 0.626 | 0 | 0.036 | 0.155 | 0.608 | 257 | 0.528 | 0 | |
| Esthetics | Chi-square | 18.621 | 0.061 | 0.028 | 100.308 | 21.272 | 0.064 | 93.439 | 25.411 | 5.164 | 0.807 | 301 | 0.817 | 1.759 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0 | 0.806 | 868 | 0 | 0 | 0.8 | 0 | 0 | 0.023 | 0.369 | 584 | 366 | 0.185 | |
| Patient Preference | Chi-square | 22.446 | 0.061 | 0.074 | 1.105 | 7.692 | 0.086 | 0.501 | 0.427 | 0.343 | 0.755 | 0.45 | 0.044 | 0.209 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0 | 0.806 | 0.785 | 0.576 | 0.006 | 0.77 | 0.479 | 0.514 | 0.558 | 0.385 | 502 | 0.833 | 0.647 | |
| Overhang | Chi-square | 0.230 | 5.878 | 2.676 | 11.647 | 0.378 | 13.787 | 0.4 | 1.371 | 10.372 | 15.979 | 7.568 | 3.610 | 1.154 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.631 | 0.015 | 0.102 | 0.003 | 0.539 | 0 | 0.527 | 242 | 0.001 | 0 | 0.006" | 0.057 | 283 | |
| Open Margin | Chi-square | 0.172 | 0.560 | 27.901 | 7.457 | 1.314 | 1.556 | 0.842 | 569 | 0.386 | 11.741 | 0.947 | 0.205. | 0.139 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.678 | 0.454 | 0 | 0.024 | 252 | 212 | 0.359 | 0.451 | 0.534 | 0.001 | 0.33 | 0.650b | 0.709 | |
| Defective | Chi-square | 0.855 | 4.168 | 0.046 | 1.084 | 5.217 | 0.286 | 0.087 | 0.001 | 1.891 | 1.206 | 7.795 | 1.406 | 0.007 |
| df | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Sig. | 0.355 | 0.41 | 0.831 | 0.582 | 0.022 | 0.593 | 0.768 | 0.978 | 0.169 | 0.272 | 0.005 | 0.236 | 0.934 | |
Table 2: Pearson chi-square tests for the cross tabulation between causes and tooth type, position, and surface.
Next, the surfaces affected according to causes. The occlusal surface was mentioned in 1461 cases by 57.6%. The occlusal surfaces showed significance with recurrent caries (P.value=0.000). While the incisal was significantly associated with fracture by (P.value=0.00).
While mesial and distal were more encountered with overhang and open margin cases with (P.value=0.001) (Figure 3 and Table 2).
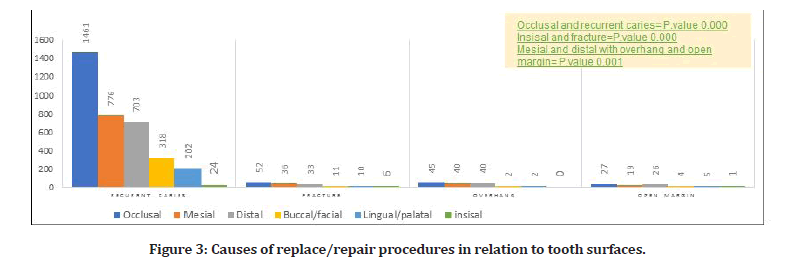
Figure 3: Causes of replace/repair procedures in relation to tooth surfaces.
Furthermore, the causes in relation to operator level. The results showed the operator level was statically significant (P.value=0.000) with recurrent caries which was found by undergraduate students in 1648 cases by 83.6%, while it was documented by 429 cases representing 76.2% of postgraduates. However, fracture showed significance (P.value=0.05) which was more seen by postgraduate students by 26 cases representing 4.6%, while in undergraduate students documented 58 cases representing 2.9% (Table 3).
| OP level | Pearson Chi-Square Tests | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Undergraduate | Postgraduate | Total | |||||||
| Count | Column N % | Count | Column N % | Count | Column N % | ||||
| Recurrent Caries | No | 324 | 16.40% | 134 | 23.80% | 458 | 18.10% | Chi square | 16.075 |
| Yes | 1648 | 83.60% | 429 | 76.20% | 2077 | 81.90% | df | 1 | |
| Sig | 0.000 | ||||||||
| Fracture | No | 1914 | 97.10% | 537 | 95.40% | 2451 | 96.70% | Chi square | 3.844 |
| Yes | 58 | 2.90% | 26 | 4.60% | 84 | 3.30% | df | 0.050 | |
| Sig | 0.50 | ||||||||
| Pain | No | 1970 | 99.90% | 560 | 99.50% | 2530 | 99.80% | Chi square | 4.141 |
| Yes | 2 | 0.10% | 3 | 0.50% | 5 | 0.20% | df | 1 | |
| Sig | 0.042 | ||||||||
| Sensitivity | No | 1969 | 99.80% | 562 | 99.80% | 2531 | 99.80% | Chi square | 0.18 |
| Yes | 3 | 0.20% | 1 | 0.20% | 4 | 0.20% | df | 1 | |
| Sig | 0.893 | ||||||||
| Discoloration | No | 1943 | 98.50% | 547 | 97.20% | 2490 | 98.20% | Chi square | 4.724 |
| Yes | 29 | 1.50% | 16 | 2.80% | 45 | 1.80% | df | 1 | |
| Sig | 0.030 | ||||||||
| Esthectics | No | 1930 | 97.90% | 553 | 98.20% | 2483 | 97.90% | Chi square | 0.273 |
| Yes | 42 | 2.10% | 10 | 1.80% | 52 | 2.10% | df | 1 | |
| Sig | 0.602 | ||||||||
| Patient preference | No | 1964 | 99.60% | 558 | 99.10% | 2522 | 99.50% | Chi square | 1.998 |
| Yes | 8 | 0.40% | 5 | 0.90% | 13 | 0.50% | df | 1 | |
| Sig | 0.158 | ||||||||
| Overhang | No | 1921 | 97.40% | 544 | 96.60% | 2465 | 97.20% | Chi square | 1.014 |
| Yes | 51 | 2.60% | 19 | 3.40% | 70 | 2.80% | df | 1 | |
| Sig | 0.314 | ||||||||
| Open Margin | No | 1935 | 98.10% | 556 | 98.80% | 2491 | 98.30% | Chi square | 1.029 |
| Yes | 37 | 1.90% | 7 | 1.20% | 44 | 1.70% | df | 1 | |
| Sig | 0.310 | ||||||||
| Defective | No | 1834 | 93.00% | 502 | 89.20% | 2336 | 92.10% | Chi square | 8.913 |
| Yes | 138 | 7.00% | 61 | 10.80% | 199 | 7.90% | df | 1 | |
| Sig | 0.003 | ||||||||
Table 3: Pearson chi-square tests for the cross tabulation between causes and operator level.
Finally, the repair/replace cases performed in relation to (G.V Black). Class II restoration showed a statistically significance (P.value=0.013) which included a 923 replace procedures done constructing 37% of all replacement cases and 22 repair procedures were done constructing 56.4% of all repair cases (Figure 4 and Table 4).
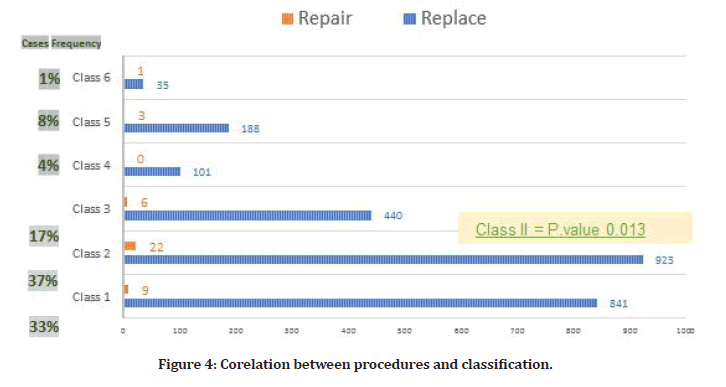
Figure 4: Corelation between procedures and classification.
| Classification | Replace | Repair | p | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Class_1 | No | 1655 | 66.3% | 30 | 76.9% | 0.163 |
| Yes | 841 | 33.7% | 9 | 23.1% | ||
| Class_2 | No | 1573 | 63.0% | 17 | 43.6% | 0.013 |
| Yes | 923 | 37.0% | 22 | 56.4% | ||
| Class_3 | No | 2056 | 82.4% | 33 | 84.6% | 0.715 |
| Yes | 440 | 17.6% | 6 | 15.4% | ||
| Class_4 | No | 2395 | 96.0% | 39 | 100.0% | 0.200 |
| Yes | 101 | 4.0% | 0 | 0.0% | ||
| Class_5 | No | 2308 | 92.5% | 36 | 92.3% | 0.970 |
| Yes | 188 | 7.5% | 3 | 7.7% | ||
| Class_6 | No | 2461 | 98.6% | 38 | 97.4% | 0.543 |
| Yes | 35 | 1.40% | 1 | 2.60% | ||
Table 4: Repair and replacement of the restorations based on classification of the cavities level.
Discussion
Despite many research having been conducted to study replacement vs. repair of failed direct restorations, no studies in Saudi Arabia were done about this controversy. In our study, we aim to find the relation between variables that can determine the treatment option among postgraduate and undergraduate students for such cases in REU, KSA.
Similar to previous studies like the one by Gordan, et al. in 2012, replacement cases were significantly higher than repair, where he found that replacement cases constructed 75% (7,073) while repair only represented 25% (2,411) of the total cases included [19].
In our study, the replacement cases represented 98% (2487) while only 2% (45) was repair cases of the total included cases. This could be explained by multiple factors for instance, most of amalgam restorations are prone to be replace rather than repair because of patient preference. Moreover, dentist would choose to replace over repair since they are not the ones who have placed the original restorations.
In relation to the patient related factors, we were enabled to conduct the average age which was around 35 years old. Also, the health state of patient where we found a total of (187) 7.4% of procedure were done on patient with a systemic disease. Diabetes mellitus was the most mentioned one. Lastly, the gender of patient, where females were the higher with 57% and males 43% of total included cases. More factors could have been considered as mentioned in Javidi, et al. in 2015 study where they include patient factors like pre-treatment anxiety, pain intensity where they found that anxiety levels were lower in patient with repair procedures [21]. While for pain had no significant difference.
In regard of operator factors, we have been able to document the operator gender and level. Unlike what was found by Gordan, et al. in 2012, where he conducted that the gender of operator was not significant [19]. And as per stated by Kattan, et al. in a recent cross-sectional study that was done in the United States, gender of the practitioner was not associated with the treatment option [22]. Our results showed that it was significant where replacement was performed more by female operators while male operators tend to replace more. We may explain that by the fact of the difference in operatorpatient relationship based on the gender of the operator where female operator mostly has a better interpersonal communication than males. Female operator can be more compassionate and expressive which enhance their relationships with their patient that can get more comfortable and cooperative. Adding to that female operator are more willing to engage the patient in the decision making of the treatment, especially if the patient was a female too as an empowering gesture? All adds up eventually to get a better insight to patients’ history thus a better treatment plan making, commitment to follow the treatment plane and end results [17].
Also, in regards of the level of operator, clinicians tend to make decisions based on what they have been taught, tempered by their clinical experience and judgment, based on whether to replace or repair a defective composite restoration [23]. Gordan’s study witnessed a higher rate of that younger dentist vs. the older ones where he explained that younger ones were more exposed to the minimal invasive treatment approach in the recent curriculum in dental schools [19]. Our results showed that replacement procedures were performed more by postgraduates while undergraduates tend more to replace. We can relate that to the level of experience in the field and managing cases. Also, the undergraduates work would be more under the supervision of older generation of doctors from different schools, which can influence the undergrad operator decision. The decision should consider that even if one or more minor defects are discovered in a restoration, this does not necessarily mean that irreversible damage has taken place to such an exten that it needs to be immediately replaced. Since restoration defects typically develop gradually over prolonged periods, clinicians have the opportunity to examine the origin of the problem and to correct the defect with a minimally invasive treatment [21].
Next, the tooth related information. We have determined several factors like: the tooth type, the position of the tooth (arch) and the surface involved. Consistent with other studies, in which Gordan, et al. in 2012 found that restorations on molars were the most replaced by 72% [19]. Moreover, Kanzow, et al. in 2020 stated that replacement was found to be in the upper arch by 67.4% of total cases [2]. In present study, molar teeth experienced more replacement with 47.7% of the cases, while premolars were the most repaired type by 46.1%.
According to tooth position, teeth in maxillary arch were the most treated teeth in replacement cases by 61.4%, while mandible was mostly in repair cases with 46.6%. We can explain the previous results in molar and maxillary higher replacement rate with the difficulty of performing a proper restoration by the operator in upper jaw or might be related to uneasy access by the patient to keep good oral hygiene in such areas. While in case of the repair procedures where premolars and mandibular teeth were the most repaired, we might assume that is due to easier access by operator and later the patient. Also, the cleansing and protective function of saliva is more active in lower arch which lead to less damage of tooth structure facilitated more conservative treatment modality for such cases. Next, the causative factors for replace/repair procedures. We have included all the common causes that can be mentioned as the cause of replace/repair an existent restoration in our study. The recurrence of caries was the most documented cause by 82% of the cases. Like other studies, secondary caries had the highest prevalence among different causes by 41.8% of total cases, and it was found by Iqbal, et al. to be 69%, also found by costa et al.,2021 by 46.7% [10,11,24].
The major cause to perform replacement and repair procedures was secondary caries which indicates that caries is a widespread dental problem among the populations. In view of that fact, the occlusal surface is most prone surface to caries. And in consistent with that, we have found that it was significantly the most of investigated teeth with secondary caries detected on occlusal surface by 57.6%. On the other hand, mesial and distal surfaces were the most effected by overhang and open margin by 62% and 54.8%.
Other causes like, discoloration and esthetic reasons or patient preference were mostly documented in upper arch anterior teeth. These causes depend on both the operator diagnosis and patient decision as well because the perception of esthetic is not the same for everyone. A dentist is more likely to criticize the esthetic appearance than patient as they compare it to a higher stander [25].
In view of that, our results also showed that tooth-colored composite restoration was the most preferred material used for replacement, which is also the most chosen material by 36.5% in a study done by Gordan et al. in 2012[17]. This can be explained by the advantages that composite can provide like, adhesion to tooth structure, reasonable cost and more importantly esthetic. The downside is that it’s longevity can be affected by factors like, extent of cavity, caries risk, operator’s skill in work and patient parafunctional habits [24].
Lastly, in accordance with the classification of the restoration, we have found the Class II restorations were the most treated by both approaches by 37% since most defects effect different surfaces in the original restoration. We can relate that to the difficulties that can affect Class II restoration placement like, extent of caries, cavity preparation, isolation during placement, material manipulation, finishing and polishing of the restoration [24,26].
Limitation
The main limitation we faced in this study is absence of determinant documentations in the investigated files. These include caries risk assessment, source of old restoration, difficulty in finding repair/replacement cases by DentoPlus codes, and the criteria used in choosing one treatment option over the other. For that, we recommend having proper documentations regarding caries risk assessment since secondary caries was the most common cause in included cases. Caries Management by Risk Assessment (CAMBRA) could be considered to prevent complications and to choose the treatment effectively. Another helpful tool for proper assessment and management is taking clinical digital photographs of indicated cases [27].
Also, since failure due to caries was mostly in molar teeth and occlusal surface, preventive treatments like Fluoride application and fissure sealants should be carried out to reduce the need of restoring teeth at first stage and replacement eventually. Moreover, since replacement is more followed method by undergraduates, we recommend that repair and minimal invasive dentistry should be more implemented in educational materials. It was also noted that composite restorations are most common material in restorative procedures in line with high prevalence of recurrent caries. So, these procedures should be done under close supervision to ensure properly performed techniques and correct placement of restorations. Regarding extracting data by using DentoPlus software, new codes should be added to facilitate accessing data since repair and replacement procedures share the same codes. Further research should include follow-up of patients to examine performed replacements and repairs and assess the longevity of each treatment modality.
Conclusion
Even though restorative procedures are the most preformed during any given clinical day at REU, the replacement/repair of restorations represents only around 6.3% out of all included restorative cases. Recurrent caries was the most mentioned cause of restoration failure by operators. Those failed restorations were seen mostly among male patients, and it was more observed in class II restorations. The decision making depends mainly on operator’s knowledge, and clinical skills in managing defected restorations.
References
- Blum IR, Özcan M. Reparative dentistry: Possibilities and limitations. Curr Oral Health Reports 2018; 5:264.
- Kanzow P, Wiegand A. Retrospective analysis on the repair vs. replacement of composite restorations. Dent Mater 2020; 36:108-118.
- Asghar S, Ali A, Rashid S, et al. Replacement of resin-based composite restorations in permanent teeth. J Coll Physicians Surg Pak 2010; 20:639-643.
- Silvani S, Trivelato RF, Nogueira RD, et al. Factors affecting the placement or replacement of direct restorations in a dental school. Contemp Clin Dent 2014; 5:54-58.
- Brunton PA, Ghazali A, Tarif ZH, et al. Repair vs. replacement of direct composite restorations: A survey of teaching and operative techniques in Oceania. J Dent 2017; 59:62-67.
- Lempel E, Tóth Á, Fábián T, et al. Retrospective evaluation of posterior direct composite restorations: 10-Year findings. Dent Mater 2015; 31:115-122.
- Kodzaeva ZS, Turkina AY, Doroshina VY. The long-term results of teeth restoration with composite resin materials: A systematic literature review. Stomatologiia 2019; 98:117-122.
- Milnar FJ. The evolution of direct composites. Compendium 2011; 32:80.
- van de Sande FH, Moraes RR, Elias RV, et al. Is composite repair suitable for anterior restorations? A long-term practice-based clinical study. Clin Oral Investig 2019; 23:2795-2803.
- Pallesen U, van Dijken JW, Halken J, et al. A prospective 8-year follow-up of posterior resin composite restorations in permanent teeth of children and adolescents in public dental health service: Reasons for replacement. Clin Oral Investig 2014; 18:819-827.
- Iqbal A, Khan MS, Maxood A, et al. The factors responsible for the failure of direct composite restorations in patients reported to college of dentistry, Al Jouf University. Inter Med J 2017; 24:475-477.
- Dennison JB, Yaman P, Fasbinder DJ, et al. Repair or observation of resin margin defects: Clinical trial after five years. Oper Dent 2019; 44:355-364.
- Staxrud F, Tveit AB, Rukke HV, et al. Repair of defective composite restorations. A questionnaire study among dentists in the public dental service in Norway. J Dent 2016; 52:50-54.
- Kanzow P, Wiegand A, Göstemeyer G, Schwendicke F. Understanding the management and teaching of dental restoration repair: Systematic review and meta-analysis of surveys. J Dent 2018; 69:1-21.
- Nikolaos A. Chrysanthakopoulos. placement, replacement, and longevity of composite resin-based restorations in permanent teeth in Greece. Int Dent J 2012; 62:161–166.
- Casagrande L, Laske M, Bronkhorst EM, et al. Repair may increase survival of direct posterior restorations: A practice-based study. J Dent 2017; 64:30-36.
- Weisman CS, Teitelbaum MA. Physician gender and the physician-patient relationship: Recent evidence and relevant questions. Soc Sci Med 1985; 20:1119-1127.
- Gordan VV, Shen C, Riley J, et al. Two-year clinical evaluation of repair versus replacement of composite restorations. J Esthet Restor Dent 2006; 18:144-153.
- Gordan VV, Riley JL, Geraldeli S, et al. Repair or replacement of defective restorations by dentists in the dental practice-based research network. J Am Dent Assoc 2012; 143:593-601.
- Gordan VV, Riley JL, Rindal DB, et al. Repair or replacement of restorations: A prospective cohort study by dentists in the national dental practice-based research network. J Am Dent Assoc 2015; 146:895-903.
- Shujaat S, Bornstein MM, Price JB, et al. Integration of imaging modalities in digital dental workflows-possibilities, limitations, and potential future developments. Dentomaxillofac Radiol 2021; 50:20210268.
- Kattan W, Urquhart O, Comnick C, et al. Repair versus replacement of defective direct restorations: A cross-sectional study among US dentists. J Am Dent Assoc 2021; 152:927-935.
- Brunton PA, Ghazali A, Tarif ZH, et al. Repair vs. replacement of direct composite restorations: a survey of teaching and operative techniques in Oceania. J Dent 2017; 59:62-67.
- Costa MB, Tomisaki ET, dos Santos DC, et al. Clinical evaluation of composite resin restorations in posterior teeth. J Health Sci 2021; 23:39-43.
- Mehl CJ, Harder S, Kern M, et al. Patients’, and dentists' perception of dental appearance. Clin Oral Investig 2011; 152:193-199.
- Javidi H, Tickle M, Aggarwal VR. Repair vs. replacement of failed restorations in general dental practice: factors influencing treatment choices and outcomes. Br Dent J 2015; 218:2.
- de Almeida CV, Pintado-Palomino K, Fortes JH, et al. Digital photography vs. clinical assessment of resin composite restorations. Odontology 2021; 109:184-192.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Khalid Fahad Alotaibi1* and Maha Mohammed Alotaibi2
1King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia2Ministry of Defence, Riyadh, Saudi Arabia
Received: 17-Oct-2022, Manuscript No. jrmds-22-77744; , Pre QC No. jrmds-22-77744(PQ); Editor assigned: 19-Oct-2022, Pre QC No. jrmds-22-77744(PQ); Reviewed: 02-Nov-2022, QC No. jrmds-22-77744(Q); Revised: 07-Nov-2022, Manuscript No. jrmds-22-77744(R); Published: 15-Nov-2022
