Research Article - (2023) Volume 11, Issue 8
Role of an Oral Physician in Management of Herpes Zoster Infection
Ketan Adesh Dodal* and Swapnil Mohod
*Correspondence: Dr. Ketan Adesh Dodal, Department of Oral Medicine and Radiology, Datta Meghe Institute of Medical Sciences, Maharashtra, India, Email:
Abstract
Herpes zoster is an entity caused due reactivation of varicella zoster virus which is the secondary infection and the primary infection is chicken pox. Varicella zoster is dsDNA virus in which the growth is induce from viral open frame DNA template. The prevalence of herpes zoster stages from 1.2 to 3.4 per one thousand men and women in youthful wholesome people whilst prevalence is 3.9 to 11.8 per one thousand men and women, amongst sufferers older than sixty-five years. There is not any seasonal version visible with herpes zoster. Recurrences are maximum normally visible in sufferers who are immunosuppressed. Early diagnosis and managing could avoid the destruction caused by herpes zoster. By the use of antivirals, analgesics (topical, oral, IV), vaccine we can reduce the risk of reactivation of virus. Most common manifestation of this disease is post herpetic neuralgia which also could be managed by opioids. Virology, serology plays an excessively big role in rapid diagnosis of the Herpes antigen in the specimens taken by the swabs. Overall, the nature behind the pathogenicity of herpes zoster is directly associated with the host immune system.
Keywords
Physician, Management, Herpes zoster, Infection
Introduction
Herpes zoster a localized cutaneous viral entity which is profound since ancient times till date. Virology for herpes zoster is directly influenced by varicella zoster virus, it is an omnipresent dsDNA virus that is present in the dermatome of nerve fibers. In 1892 the association between varicella zoster and herpes zoster was established. The contamination commonly affords as awesome entities: Chickenpox (the number one contamination) and herpes zoster (additionally recognized as zoster), a secondary condition. VZV a virus of herpes group causes chicken pox. Primary VZV contamination commonly manifests in youngster as chickenpox, a seasonal viremia that has tendency to arise in epidemics [1].
In most cases of herpes zoster infection, is a sequel of varicella zoster infection which might get reactivated during life period due to weakening of immunity. After a VZV contamination resolves and immunity develops, geriatric patients are most risk because of secondary systemic diseases, immunosenescence associated with advancing age. It is present as vesicular rash, localized, burning pain, itching, lesions which shows less tendency towards discharge. Herpes zoster vaccine is the main tool aiding against the viral infection. Recent data shows 4 × more complexity in older patients. However, in managing of HZ need a prompt diagnosis, treatment with antivirals and adequate pain control. Chest dermatome (68%) was commonest to get involved followed by neck (14.5%), trigeminal (9.7%) and lumbar and sacral (8%). Management option includes-herpes vaccination, antivirals, herbal medicines [2].
Materials and Methods
Infection caused by varicella zoster virus
Morphology and pathogenesis: The Varicella-Zoster Virus (VZV) is a type of herpesvirus. Though signs of an infection with herpesviruses vary insidious, the taxonomy of the debris and the organic residences of all participants are very similar. Herpes Simplex Virus kind 1 (HSV-1), Herpes Simplex Virus kind two (HSV-2), VZV, Human cytomegalovirus (HM V). Epstein-Barr Virus (EBV) and the human herpesviruses kind six to eight (HHVG, HHV7, HHV8) belong to this division. Based on the morphology and the structure of virion they are classified into a separate group of viruses [3]. The virion of herpes virus is of 120 nm-300 nm, the size may vary. The core which contains DNA is covered by icosahedron capsid, which is bounded by tegument as middle layer and limited by envelop which has glycoprotein spikes. The viral growth of VZV is directly linked to open reading frame 5 which have ammino acids which codes for glycoprotein B, C, E. H, I, L and two reputed K and V, both of which plays a significant role in its growth [4].
Varicella zoster a virus which is particularly a host specific, causes chickenpox in childhood and then it incubates itself into the ganglion, which might be the reason for muscle paresis, as the time progresses and consequently the immunity of the patient is compromised the varicella zoster virus multiply and induces the infection which present as cutaneous rashes over the body. After successive transmission of VZV to a varicella-prone individual, primarily the respiratory mucosa will become inflamed, mainly there is invasion into the epithelium of the tonsils, wherein there can be a few manufacturing of molecular-loose VZV which could probably be neutralized through passive immunization. Subsequently, at some point of the incubation duration of varicella, VZV infects CD4+ and CD8+ T lymphocytes [5]. During VZV viremia, which may also final for a few days, VZV-inflamed immune cells, which domestic to the pores and skin, deliver contamination to keratinocytes. This viremia can also infect different cells and tissues withinside the body. Innate immunity, regarding manufacturing of alpha interferon, transiently controls the multiplication of VZV with inside the pores and skin, however ultimately innate resistance in pores and skin is overcome, ensuing with inside the improvement of cutaneous lesions. The preliminary resistance that innates immunity affords has been postulated to gradual viral multiplication, thereby supplying time for the improvement of adaptive immunity, which sooner or later controls multiplication of the virus. The capacity of innate immunity to gradual the unfold of VZV backs up the diversion of VZV to overdue endosomes all through envelopment in inflamed cells, which guarantees gradual molecular-to-molecular transmission, and for this reason affords a fail-secure mechanism to save you VZV from overwhelming its host [6].
As a result of these mechanisms, which determine host survival, the virus acquires an adaptive value. The drug's ability to safeguard you clinically suspected disorder may be assisted by the exceptionally long gestation period of two to a few weeks [7]. VZV's molecular-to-molecular disintegration, which restricts virions from propagating just outside of the cell, explains why CD4 and CD8 T lymphocytes are more vital for host protection than specific antibodies. Patients with minimal innate and/or adaptive molecular-mediated host responses are at risk of suffering VZV infections, which could have been linked to the virus's immunization pressure remaining muted. VZV molecular-mediate study in the lab. Complications because of reactivation of VZV consist of an encephalomyelitis, segmental motor weak spot and myelopathy, cranial neuropathies, Guillain-Barre syndrome, enteric features and zoster sine herpete (Figure 1) [8].
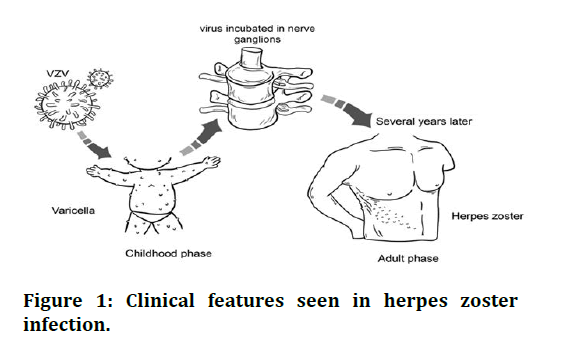
Figure 1: Clinical features seen in herpes zoster infection.
Clinical features seen in herpes zoster infection
Herpes zoster is an entity due seen due to reactivation of varicella zoster virus which was previously breached the nerve dermatomes for a specific time period in which various physiologic changes takes place such as ageing, systemic diseases which makes the reactivation of varicella zoster virus. The hope theory simpson reasoned that reactivation was prevalent and could arise with or without symptoms [9]. The prognosis of VZV contamination is typically made clinically with the aid of using the arrival of the pores and pruritus. In uncommon performing cases, the prognosis can be made with the aid of using figuring out VZV DNA in pores and skin lesions with the aid of using PCR. Isolating the VZV from pores and skin lesions a very sensitive technique but it can also be utilized, but it is significantly more costly, takes much longer, is scarce and is far less sensitive than PCR. In patients with suspected meningitis or encephalitis and various headaches caused by VZV, viral DNA can be detected in cerebrospinal fluid and/or saliva. Infants born to varicella-infected mothers during the first 20 weeks of pregnancy have quite a 2% probability of gaining congenital varicella syndrome. The affected newborns frequently have severe clinical manifestations these include their central nervous system, sites where ophthalmic nerve supply its motor and sensory fibers, upper limbs and lower limbs, skin and majority of them die in infancy or adolescent years [10].
Neurologic manifestations of herpes zoster:
• Oculomotor>Trochlear>Abducens: Ophthalmoplegia,
optic neuritis.
• Cranial nerve V: Keratitis, localized vesicles seen on
nasal tip (Hutchinson sign), loss of sight reversible or
irreversible, necrosis of bone and instinctive
exfoliation of teeth.
• Facial: Unilateral or bilateral facial muscle weakness,
rash present in ipsilateral fasion, external ear,
anterior two-thirds tongue or hard palate, Ramsay
hunt syndrome
• Cervical spine: Upper extremity weakness
diaphragmatic paralysis.
• Thoracic, lumbosacral spine: Extremity weakness and
gastrointestinal dysfunction
• Post herpetic neuralgia: It is an untreated neurologic
pain elicited by acute herpes zoster, managed bytricyclic
antidepressants, gabapentin
Presentation of rash on the body: The rash of herpes zoster is present unilaterally which is a pathognomic feature is and may include neighboring dermatomes, with the most common being thoracic plexus, cervical plexus and trigeminal plexus involvement [11]. In trigeminal plexus the ophthalmic division is most commonly involved. During a 7-10-day period, it advances from a maculopapular rash to one with clusters of vesicles that ulcerate and crust, an attempt toward healing which very unaesthetic. On average, healing takes 2-4 weeks. Once all lesions have crusted, the rash is considered non-infectious. Scarring and pigmentation are the most common complication of crusting. When the herpes zoster rash appears, the differential diagnosis includes herpes simplex virus, contact dermatitis, insect bites, folliculitis, impetigo, candidiasis and scabies [12].
Results and Discussion
Epidemiology of herpes zoster in Indian population and in orofacial region
According to the study done in 2013, 120 patients were subjected for study the incidence based on age group and prodromal symptoms (Figure 2) [13].
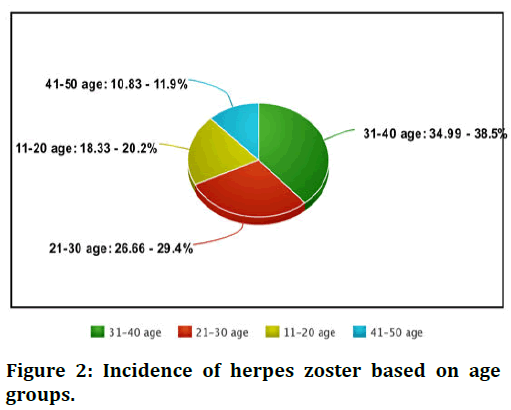
Figure 2: Incidence of herpes zoster based on age groups.
Incidence of herpes zoster based on age groups showing most commonly involved age group is 31-40 nearly 34.99% people are involved the least involved age group is 41-50 i.e., 10.83%. In middle age groups and children's and teenagers they are moderately involved (Figure 3) [14].
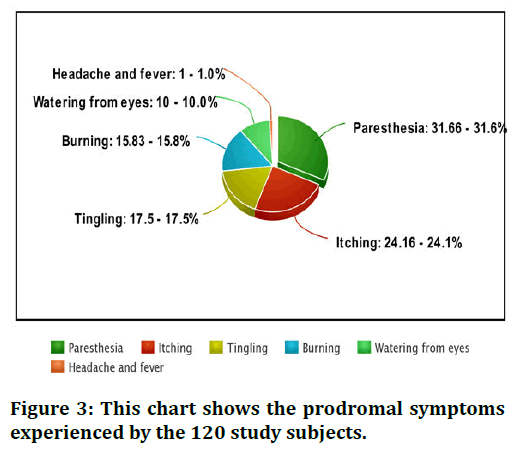
Figure 3: This chart shows the prodromal symptoms experienced by the 120 study subjects.
Oral manifestations of herpes zoster
Oral manifestation for herpes zoster seen when mandibular and maxillary divisions and mandibular division of trigeminal nerve is infiltrated by varicella zoster virus. Craniofacial osseous and dental defects such as devitalization of tooth, internal root resorption, maxillary and mandibular necrosis. Distinct ulcerative lesions are noticed on GB sulcus, buccal mucosa, palate, lips. Prompt investigations and correct management of entity is required to avoid significant morbidity. Trigeminal nerve is involved in 20% of cases of herpes zoster. All the divisions of trigeminal nerve like opthalmic, maxillary, mandibular nerves (Figures 4,5 and Table 1).
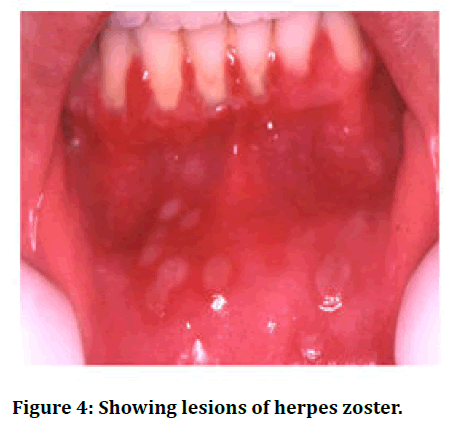
Figure 4: Showing lesions of herpes zoster.
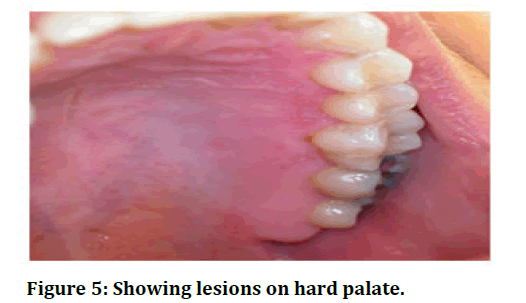
Figure 5: Showing lesions on hard palate.
| Presence of herpes zoster the head and neck region | Herpes zoster opthalmicus, herpes zoster oticus | Intraocular involvement, vestibulocochlear deformity |
| Herpes zoster present with moderate-to-severe acute disease-associated pain | Painful, draining lesions | Post herpetic neuralgia |
| Herpes zoster with cutaneous lesions | Abberent vesicles, necrotic lesions | Post herpetic neuralgia, visceral dissemination |
| Herpes zoster with visceral involvement | Cutaneous destruction of fascia's | Cutaneous lesions |
| Herpes zoster in immunocompromised patients | Malignancy, organ transplantations | Systemic viremia |
Table 1: Complications of herpes zoster infection.
Diagnosis and management of herpes zoster
Management of herpes zoster requires prompt investigations and accurate diagnosis to avoid morbidity.
Diagnosis of herpes zoster: The rash may be present on all over the body but most predominantly present in oral cavity. The patient may complain of ulcerative lesion over the buccal mucosa, labial mucosa, palate, lips. Patient may complain of burning sensation. Swab is taken from the lesion and is sent to microbiologist is preserving media. The diagnosis is mostly done by virology methods, serological methods. The lab diagnosis of VZV is done by examining the clinical specimens present with the infectious viral DNA. Immunofluorescence with polyclonal or monoclonal antibodies for VZV is used for rapid detection of viral antigens. Cell culture methods are time taking process to detect any cytological changes. Hybridization and PCR techniques are very sensitive the error is less than 1% but due to quite expensive diagnostic tool, this method is not much commonly used. Serological investigation is used most commonly because of rapid detection of viral antigens but they are not that sensitive as much as PCR, hight IgG values are expected in individual with acute infection of VZV. The range of IgG determine the immune level of the suspected individual (Tables 2 and 3).
| Primary herpetic gingivostomatitis | Keratinized mucosa (palate, labial, buccal) |
| Aphthous ulcers | Non vesiclulous, nonkeratinized |
| Herpangina | Acute, multiple ulcers, posterior oral cavity, mild systemic symptoms, more common in children |
| Bechet disease | Uveitis, genital ulcers, acneiform lesion, pseudo folliculitis, erythema nodosumlike lesions, arthritis |
Table 2: Differential diagnosis of oral ulcers.
Prevention and management
Prevention the reactivation of VZV, newer vaccine was developed to reduce the morbidity of the infection. This includes:
• Passive antibody prophylaxis is made of high titre
preparation of IgG antibodies, it produces prophylaxis
against the virus. However, this is not advised for
highly suspected individuals, infants. Criteria for
dosage should be administered within 96 hrs after
exposure.
• Antiviral prophylaxis is used to prevent the
reactivation but is used very rarely in clinics.
• Live attenuated varicella vaccine contains the VZV
strain Oka using the Takahashi method. However, this
is contraindicated in pregnancy, blood dyscrasias.
• Antivirals.
| Drug agent | Dose regimen | Duration |
|---|---|---|
| Acyclovir I.V, O | 8 mg-10 mg iv TDS, 800 mg oral five times a day | 7 days |
| Valacyclovir/Oral | 1000 mg TDS | 7 days |
| Famciclovir/Oral | 250 mg TDS | 7 days |
Table 3: Antivirals drug and doses.
Pain management in herpetic patients: Managing the pain in the herpes zoster pain is a very challenging task to cover, where initially the pain is insidious and progressive.
• Strong opioids: Hydromorphone
• Mild opioids: Tramadol, tilidine
• Non opioids analgesics: NSAIDS
Post treatment complications
Coin has two sides, in this case good outcome of treatment and poor/bad outcome of the treatment, vaccines, oral antivirals, analgesics. Few trails were conducted in which vidarabine drug action was studied. Its neurotoxicity led the reduced use of the drug.
• C/F of vidarabine induced neurotoxicity
• Grossly tremors
• Coma
• Death
Conclusion
As the oral cavity is mirror for most of the diseases, many systemic problems are reflected in the oral cavity, as dentists are in prime concerned about the oral cavity of the patient. As the herpes zoster is the secondary infection of varicella zoster, where therein presence of ulcerative lesions is seen on the buccal, labial mucosa, hard palate, soft palate, the patient may complain to the dentist that he is unable masticate properly, pain during mastication, burning sensation, red lesions in the oral cavity. A role of a dentist in diagnosis and management of the herpes zoster is very dominant, as their appearance of these lesions in the oral cavity. Early diagnosis plays very important role in avoiding the morbidity.
References
- Shah S, Singaraju S, Einstein A, et al. Herpes zoster: A clinicocytopathological insight. J Oral Maxillofacial Pathol 2016; 20:547.
[Crossref] [Google Scholar] [PubMed]
- John AR, Canaday DH. Herpes zoster in the older adult. Infect Dis Clin 2017; 31:811-826.
[Crossref] [Google Scholar] [PubMed]
- Das AL, Sayal SK, Gupta CM, et al. Herpes zoster in patients with HIV infection. Ind J Dermatol Venereol Leprol 1997; 63:101-104.
[Google Scholar] [PubMed]
- Dolin R, Reichman RC, Mazur MH, et al. Herpes zoster-varicella infections in immunosuppressed patients. Ann Intern Med 1978; 89:375-388.
[Crossref] [Google Scholar] [PubMed]
- Kennedy PG, Gershon AA. Clinical features of varicella-zoster virus infection. Virus 2018; 10:609.
[Crossref] [Google Scholar] [PubMed]
- Bergelson J, Zaoutis T, Shah SS. Pediatric infectious diseases E-Book: Requisites. Elsevier Health Sciences, USA, 2008, pp. 1-18.
- Awan A, Einstein G, Tulp O. Pathogenesis and chemotherapy of a thymidine kinase deficient mutant strain of HSV‐1 in a murine zosteriform infection model. FASEB J 2021; 35.
- Wehrhahn MC, Dwyer DE. Herpes zoster: Epidemiology, clinical features, treatment and prevention. Aus Prescrib 2012; 35.
- Rahaus M, Schunemann S, Wolff MH. Morphological and biological characteristics of varicella-zoster virus. Contribut Microbiol 1999; 3:1-9.
[Crossref] [Google Scholar] [PubMed]
- Mo C, Suen J, Sommer M, et al. Characterization of varicella-zoster virus glycoprotein K (open reading frame 5) and its role in virus growth. J Virol 1999; 73:4197-4207.
[Crossref] [Google Scholar] [PubMed]
- Furue M, Yamazaki S, Jimbow K, et al. Prevalence of dermatological disorders in Japan: A nationwide, cross‐sectional, seasonal, multicenter, hospital‐based study. J Dermatol 2011; 38:310-320.
[Crossref] [Google Scholar] [PubMed]
- Frisch S, Guo AM. Diagnostic methods and management strategies of herpes simplex and herpes zoster infections. Clin Geriatr Med 2013; 29:501-526.
[Crossref] [Google Scholar] [PubMed]
- Arvin AM. Varicella-zoster virus. Clin Microbiol Rev 1996; 9:361-381.
- Gross GE, Eisert L, Doerr HW, et al. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia. J Der Deutschen Dermatologischen Gesellschaft 2020; 18:55-78.
Author Info
Ketan Adesh Dodal* and Swapnil Mohod
Department of Oral Medicine and Radiology, Datta Meghe Institute of Medical Sciences, Maharashtra, IndiaCitation: Ketan Adesh Dodal, Swapnil Mohod, Role of an Oral Physician in Management of Herpes Zoster Infection, J Res Med Dent Sci, 2023, 11 (08): 048-052.
Received: 16-Nov-2021, Manuscript No. JRMDS-22-47645; , Pre QC No. JRMDS-22-47645 (PQ); Editor assigned: 19-Nov-2021, Pre QC No. JRMDS-22-47645 (PQ); Reviewed: 03-Dec-2021, QC No. JRMDS-22-47645; Revised: 19-Jul-2023, Manuscript No. JRMDS-22-47645 (R); Published: 16-Aug-2023
