Research - (2021) Volume 9, Issue 5
Role of Inflammatory Markers as a Predictor of Peripheral Vascular Disease in Chronic Asymptomatic Diabetic Patients
D Sangeetha and V Padma*
*Correspondence: V Padma, Department of General Medicine, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
To identify whether inflammatory markers are good predictors of peripheral vascular disease in chronic asymptomatic type 2 Diabetes Mellitus patients. The reactive of the study is to identify overly sensitive inflammatory markers which will be useful in early detection of peripheral vascular disease in asymptomatic diabetic patients and to identify a simple blood test for this purpose. Total number of patients included in this study were 88. There were 31 males, 57 female patients ranging from 30 years to 70 years, who were diagnosed to have type 2 diabetes mellitus of more than 3years of duration. Although coronary and peripheral arterial diseases are macrovascular complications of diabetes, the clinical manifestations of peripheral vascular disease occur almost a decade later than coronary artery disease. Thus inflammatory markers serve as a sensitive tool to identify the subset of chronic diabetics who are at a high risk of developing peripheral vascular disease.
Keywords
Inflammation, Thrombosis, Lipoprotein metabolism, Oxidative stress.
Introduction
Peripheral vascular disease (PVD) is a Major cause of morbidity and mortality especially affecting the elderly population. The prevalence of PVD is multifold higher in patients with diabetes compared with age- and sex matched nondiabetic subjects, and this may be because of hyperglycemia, hypertension, hyperlipidemia, platelet factors, and other factors that are increased in diabetic subjects. Recent estimates by the World Health Organization show that India already has the largest number of diabetic patients in any given country, and this trend will continue in the future. Several studies have shown that the prevalence of coronary artery disease (CAD) is extremely high among Asian Indians. Unfortunat1;11/y, there is extraordinarily little epidemiological data on PVD in Indian population. Earlier clinic-based reports suggested that PVD is less common among Indian diabetic patients in South India. In the available studies, the overall prevalence of PVD estimated in the whole population was 3.2%, and it was 6.3% in the diabetic population. Thus, although prevalence of PVD is low among south Indian population, it is relatively high among those with diabetes Atherosclerotic vascular disease affects large- and mediumsized arteries of most circulatory beds and is the leading cause of death and disability in developed countries. Lower-extremity atherosclerotic peripheral arterial disease (PAD) is a significant public health problem. Conventional risk factors known to contribute to markers in pathways of inflammation, thrombosis, lipoprotein metabolism, and oxidative stress in determining susceptibility to PAD is not fully defined [1-5].
Validation of novel risk markers for PAD may allow earlier detection, an improved understanding of disease etiology and progression, and the development of new therapies. Since PAD may have varying clinical presentations, a valuable tool for investigating novel markers for this disease is the ankle-brachial index (ABI), an objective, reproducible, non-invasive measure that correlates with PAD severity. ABI=0.90 is 95% sensitive and 90% specific for the presence of a=50% narrowing of a lower extremity artery and is used in the clinical setting to establish a diagnosis of PAD. ABI over time provides a measure of PAD progression and ABI also provides prognostic information. Patients with severe PAD (ABI=0.40) have a significantly decreased survival, with only 24% of patients alive at 12 years. In recent years, several 'novel' circulating marker including C-reactive protein (CRP), fibrinogen, lipoprotein(a) (Lp(a)), and homocysteine have been examined as potential risk factors for atherothrombotic vascular disease. This review will focus on role of inflammatory markers in predicting the onset of PAD before the manifestation of clinical features [6-9].
The term peripheral arterial disease (PAD) is widely used to refer to chronic arterial disease of the legs of atherosclerotic origin. Atherosclerosis is by far the most common cause (>90%) of arterial problems in the leg (1). PAD affects about 5% of the elderly population over 55 years in the western world (2). Several studies have demonstrated that inflammation is also involved in the development of PAD (3-9). Previous studies have demonstrated that PAD is strongly associated with elevated plasma levels of the inflammatory markers Creactive protein (CRP) and fibrinogen Moreover, other studies [10,11]. Accordingly, diabetes shows a high prevalence in the general population and is a crucial risk factor for cardiac and arterial disease [12-15]. The pivotal and crucial role played by inflammation in the pathophysiology of PAD has received much attention. Based on our current knowledge, we propose that inflammatory mediators may be involved in PAD development. A substantial body of evidence has accumulated to support a key role for inflammation in the development and progression of atherosclerosis. Several studies have investigated the association of various markers of vascular inflammation including acute phase reactants (CRP), cytokines (interleukin-6(IL-6)), cellular adhesion molecules (CAMs), white blood cell (WBC) count, and beta2-microglobulin, with manifestations of atherosclerotic vascular disease. Novel circulating markers that have been implicated in PAD [16,17].
Materials and Method
Study population
This study was conducted in the Department of Medicine of Sree Balaji Medical College, Chennai, Tamil Nadu during the period of August 2010 to August 2011.Total number of patients included in this study were 88. There were 31 males, 57 female patients ranging from 30 years to 70 years, who were diagnosed to have type 2 diabetes mellitus of more than 3years of duration.
Study design
This study is a cross sectional study. This study is aimed to assess the role of inflammatory markers like high sensitivity CRP, apoA, apo-B, homocysteine level in asymptomatic type 2 diabetic patients as a predictor for peripheral vascular disease.
Inclusion criteria
✓ Male and female patients of age >30 years were selected.
✓ Subjects who are diabetic for >3 years with or without treatment were included.
✓ Subjects Blood Pressure should be between 110-140/70- 90mm Hg with or without treatment.
✓ Subjects with no history of heart disease or complaints related to cardiac disease like history of CAD, moderate to severe valvular disease, atrial fibrillation, or other severe arrhythmias and congenital heart disease were enrolled into the study.
✓ Subject with no history of End Stage Renal Failure.
✓ Subjects with normal Doppler study.
Exclusion criteria
✓ Subjects with presence of pathological Q waves, LV hypertrophy on voltage criteria, or ST/T wave abnormalities in ECG.
✓ Subjects with history of peripheral vascular disease
✓ History of Congestive Heart Failure.
✓ History of End Stage Renal Failure.
✓ History of Smoking.
✓ History of Alcohol.
✓ Subject with uncontrolled hypertension.
✓ Patient who is not willing to participate in the study.
✓ Individuals _who are cognitively impaired and/or who are unable to give informed consent.
✓ Any other health or mental condition that in the Investigator's opinion may adversely affect the subject's ability to complete the study.
✓ History of autoimmune disorders and connective tissue disorders.
Results
The mean age of the study population was about 50 years, and the mean duration of diabetes was 7 years. The renal function tests and liver function tests' mean were within normal limits. The mean apo-A level was 96 mg/dl (with 110mg/ dl being the upper limit for normal) with a range from 0.97 to 139 mg/dl. The mean apo-B level was 91.8 i:ng/dl with 90mg/dl being the upper limit for normal. The mean homocysteine level was 2.8mg/dl with 1 mg/dl being the upper limit for normal. Our study population consisted of mainly middle-aged diabetics in the age group of 40 to 60 years with a minority from below 40 years and above 61 years. Hence most of the people who were studied were middle aged diabetics with no major co morbid illness (Table 1).
| Age group | Frequency | Percent |
|---|---|---|
| Up to 40yrs | 19 | 21.6 |
| 41 - 50yrs | 22 | 25 |
| 51 - 60 | 28 | 31.8 |
| 61yrs or more | 19 | 21.6 |
| Total | 88 | 100 |
Table 1: Age groups.
Our study population consisted of predominantly female population, due to regular outpatient visits and compliance with follow up protocols by females compared to males in our study group (Table 2). Apo-A levels were only elevated in a minority of the study group (20.5%) whereas Apo-B levels were elevated in about (70.5 %) of the study group (Table 3). Overly sensitive CRP levels were elevated in about 64.8% of the study population One parameter was elevated in almost 40 % of the study population and two parameters were elevated in 35 % of study population thus adding up to a significant percentage of those studied (Table 4). Table 5 shows the Number of parameters abnormal levels. Table 6 and 7 Shows the APO A and TC levels.
| Gender | Frequency | |
|---|---|---|
| Male | 31 | 35.2 |
| Female | 57 | 64.8 |
| Total | 88 | 100 |
Table 2: Shows the Gender and frequency.
| APO A Level | Frequency | Percent |
|---|---|---|
| Normal | 70 | 79.5 |
| Abnormal | 18 | 20.5 |
| Total | 88 | 100 |
Table 3: Shows the APO levels.
| HCRP Level | Frequency | Percent |
|---|---|---|
| Normal | 31 | 35.2 |
| Abnormal | 57 | 64.8 |
| Total | 88 | 100 |
Table 4: HCRP levels.
| Number of parameters abnormal | Frequency | Percent |
|---|---|---|
| None | 12 | 13.6 |
| One | 35 | 39.8 |
| Two | 31 | 35.2 |
| Three | 10 | 11.4 |
| Total | 88 | 100 |
Table 5: Number of parameters abnormal levels.
| Variable | Elevated | N | Mean | Std. Dev | Min | Max | F-Value | P-Value |
|---|---|---|---|---|---|---|---|---|
| APOA mg/dl | None | 12 | 118.18 | 8.1 | 111.1 | 139.2 | 28.16 | <0.001 |
| One | 35 | 102.11 | 8.44 | 90.3 | 122.9 | |||
| Two | 31 | 89.48 | 7.52 | 77.4 | 109.7 | |||
| Three | 10 | 68.31 | 35.39 | 1 | 88.5 | |||
| Total | 88 | 96.01 | 19.27 | 1 | 139.2 |
Table 6: APO A level.
| Variable | Elevated | N | Mean | Std. Dev | Min | Max | F-Value | P-Value |
|---|---|---|---|---|---|---|---|---|
| TC | None | 12 | 184.08 | 46.61 | 107 | 256 | 1.99 | 0.122 |
| One | 5 | 176.71 | 47.24 | 114 | 345 | |||
| Two | 31 | 165.45 | 44.9 | 89 | 287 | |||
| Three | 10 | 142.5 | 34.74 | 106 | 210 | |||
| Total | 88 | 169.86 | 45.9 | 89 | 345 |
Table 7: TC levels.
Thus, from the above Figure 1 it is clear that Apo-B is the variable that is significantly elevated in 70.5% of the study population with a mean value of 91.8mg/dl, which is higher than the upper limit of normal (90 mg/dl). the association was statistically significant with p value of 0.009. hCRP was elevated in 64.8 % of the study population with mean value of 2.85 mg /dl, which was significantly higher than the normal level (1 mg/dl). The association was statistically significant with a p value of <0.001. Apo-A value was only elevated in 20.5% of the study population with a mean value of 96.01 mg/dl which is lower than the upper limit of normal (110 mg %). Hence hCRP and apo B were the variables elevated in our study population with a significant p value.
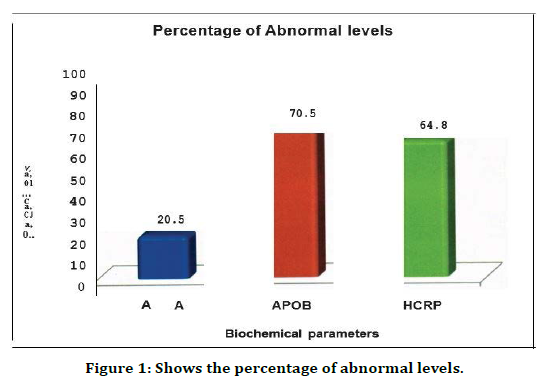
Figure 1. Shows the percentage of abnormal levels.
The above Figure 2 shows that one parameter was alone elevated in 39.8% of the study group and two parameters were elevated in 35.2 % of the study group and three parameters were elevated in 11.4 % of the study group and only 13.6% of the study population had all parameters within normal range.
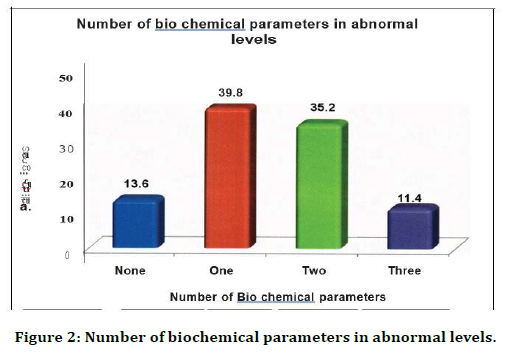
Figure 2. Number of biochemical parameters in abnormal levels.
Discussion
Although coronary and peripheral arterial diseases are macrovascular complications of diabetes, the clinical manifestations of peripheral vascular disease occur almost a decade later than coronary artery disease. Majority of patients with peripheral vascular disease have associated coronary artery disease, however the opposite isn't true. Although atherosclerosis in patients with diabetes is similar to that seen in non-diabetic patients, it is generalized, occurs prematurely and progresses at an accelerated pace. Peripheral vascular disease in -- diabetics differs from that in non-diabetics in many aspects [18].
In non-diabetics the sites of occlusion are usually the infrarenal aorta, iliac ana superficial femoral arteries, with sparing of distal vessels. Whereas, in diabetics occlusive lesions occur in crural arteries, namely tibials and peroneals, with sparing of the arteries of the foot. This characteristic vascular involvement in diabetics had made it possible to carry out vascular reconstruction, where proximal vessel like popliteal is anastomosed to foot vessels like dorsalis pedis thus bypassing the obstructed tibial and peroneal vessels., This pedal artery bypass technique has led to a significant decline in the incidence of all levels of limb amputations .Hence the need to diagnose peripheral vascular disease in diabetics at an early stage so that prevention of complications by early intervention is possible [19]. The overall prevalence of PVD among Indians is considerably low as compared to the Western patients. Mohan et al have reported the prevalence of PVD in South Indian diabetics to be 3.9%. in Western series the prevalence ranges between 22 - 45%. The prevalence of PVD in diabetics increases with age increasing from 3.2% in those below 50 yrs of age to 33% in those above 80 yrs. of age. The prevalence of PVD in diabetics also increases with the duration of diabetes from 15% to 45% at 10 to 20 years respectively after the diagnosis of diabetes. In India, the number of diabetic patients above the age of 80 years or with duration of diabetes more than 30 years is extremely low, thus explaining the low prevalence of PVD in diabetics. In the coming years with better disease care, longevity of our diabetics would significantly increase, and it will not be surprising to see an alarming increasing prevalence of PVD in Indian diabetics [20,21].
Indian diabetics also present with peripheral vascular disease at an advanced stage h foot ulcers and advanced vascular disease where even limb salvage is not possible. The existing investigations like Doppler, duplex Doppler, ct angiogram, MR Angiogram all detect vascular disease after onset and there are no standard tests to diagnose peripheral vascular disease before the onset. we generally investigate for peripheral vascular disease only in a symptomatic patient with positive history for claudication pain [22-24]. In such symptomatic patients we also preformed serum inflammatory markers along with Doppler study to find out the association between them. we found serum proinflammatory markers were significantly elevated in peripheral vascular disease patients. This was the basis for our study to be performed in chronic asymptomatic diabetic patient, as a predictor of peripheral vascular disease [25].
This study shows that inflammatory markers like hCRP, apo-A and apo-B which are sensitive markers for detection of peripheral vascular disease are also elevated in diabetics who do not have overt vascular disease [26-29]. Overly sensitive CRP was elevated in 64.8% of the population,20.5% of them had elevated apo-A and apo-B was around 70.5% of the total population. Among all these bio-markers apo-B was significantly found to be elevated in our study. Also it demonstrates that only 13.5% of the diabetic patients remain to be unaffected, rest all the diabetic patients showed significant elevation in the serum biomarkers. The main aim of our study is to identify the diabetic patients prior to this development of macrovascular complications using a simple screening tool [30- 33]. Hence these simple blood tests can be used to follow up this subset of diabetic population who are at high risk of development of peripheral vascular disease so that early intervention is possible.
Conclusion
Inflammatory markers have been proven to have a role in diagnosing cardiovascular disease at an early stage before the onset of symptoms. They have also been studied extensively in peripheral vascular disease and found to have a role in the diagnosis of peripheral vascular disease at an early stage. In this study we have studied the levels of inflammatory markers in chronic diabetic population (>3 years) and found out that 2 inflammatory markers i.e., hCRP and apo-B were elevated in the study population. This subset of population is being monitored for the onset of peripheral vascular disease by using ABI and Doppler imaging. Thus, inflammatory markers serve as a sensitive tool to identify the subset of chronic diabetics who are at a high risk of developing peripheral vascular disease.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Criqui MH. Peripheral arterial disease: Epidemiological aspects. Vase Med 2001; 6:3-7.
- Muller-Buhl U, Wiesemann A, Oser B, et al. Correlation of hemodynamic and functional variables with the angiographic extent of peripheral arterial occlusive disease. Vase Med 1999; 4:247-251.
- Doobay AV, Anand SS. Sensitivity and specificity of the ankle branchial index to predict future cardiovascular out-comes: A systematic review. Arterioscler Thromb Vase Biol 2005; 25:1463-1469.
- McKenna M,Wolfson S, Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis 1991; 87:119-128.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). Circulation 2006; 113:e463-e654.
- Feinglass J, McCarthy WJ, Slavensky R, et al. Effect of lower extremity blood pressure on physical functioning in patients who have intermittent claudication. The Chicago claudication outcomes research group. J Vasc Surg 1996; 24:503-512.
- Wang CH, Li SH, Weisel RD, et al. C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation 2003; 107:1783-1790.
- Torzewski J, Torzewski M, Bowyer DE, et al. C-reactive protein frequently colocalizes with the terminal complement complex in the intima of early atherosclerotic lesions of human coronary arteries. Arterioscler Thromb Vase Biol 1998; 9:1386-1392.
- Ridker PM, Cushman M, Stampfer MJ, et al. Plasma concentration of C-reactive protein and risk of developing peripheral vascular disease. Circulation 1998; 97:425-428.
- Pradhan AD, Shrivastava S, Cook NR, et al. Symptomatic peripheral arterial disease in women: nontraditional biomarkers of elevated risk. Circulation 2008; 117:823-831.
- Bloemenkamp DG, van den Bosch MA, Mali WP, et al. Novel risk factors for peripheral arterial disease in young women. Am J Med 2002; 113:462-467.
- Unlu Y, Karapolat S, Karaca Y, et al. Comparison of levels of inflammatory markers and hemostatic factors in the patients with and without peripheral arterial disease. Thromb Res 2006; 117:357-364.
- Yu HI, Sheu WH, Song YM, et al. C-reactive protein and risk factors for peripheral vascular disease in subjects with Type 2 diabetes mellitus. Diabet Med 2004; 21:336-341.
- McDermottMM, Green D, Greenland P, et al. Relation of levels of hemostatic factors and inflammatory markers to the ankle brachial index. Am J Cardiol 2003; 92:194-199.
- Pande RL, Perlstein TS, Beckman JA, et al. Association of insulin resistance and inflammation with peripheral arterial disease: the national health and nutrition examination survey, 1999 to 2004. Circulation 2008; 118:33-41.
- Vidula H, Tian L, Liu K, et al. Biomarkers of inflammation and thrombosis as predictors of near-term mortality in patients with peripheral arterial disease: A cohort study. Ann Intern Med 2008; 148:85-93.
- Beckman JA, Preis 0, Ridker PM, et al. Comparison of usefulness of inflammatory markers in patients with versus without peripheral arterial disease in predicting adverse cardiovascular outcomes (myocardial infarction, stroke, and death). Am J Cardiol 2005; 96:1374-1378.
- Jialal I, Stein D, Balis D, et al. Effect of hydroxymethyl glutaryl coenzyme a reductase inhibitor therapy on high sensitive C-reactive protein levels. Circulation 2001; 103:1933-1935.
- Albert MA, Danielson E, Rifai N, et al. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA 2001; 286:64-70.
- Despres JP, Lemieux I, Pascot A, et al. Gemfibrozil reduces plasma C-reactive protein levels in abdominally obese men with the atherogenic dyslipidemia of the metabolic syndrome. Arterioscler Thromb Vase Biol 2003; 23:702-703.
- Levin EG, Miles LA, Fless GM, et al. Lipoproteins inhibit the secretion of tissue plasminogen activator from human endothelial cells. Arterioscler Thromb 1994; 14: 438-442. 390.
- Grainger DJ, Kirschenlohr HL, Metcalfe JC, et al. Proliferation of human smooth muscle cells promoted by lipoprotein (a). Science 1993; 260:1655-1658.
- Valentine RJ, Graybum PA, Vega GL, et al. Lipoprotein is an independent, discriminating risk factor for premature peripheral atherosclerosis among white men. Arch Intern Med 1994; 154:801-806.
- Valentine RJ, Kaplan HS, Green R, et al. Lipoprotein (a), homocysteine, and hypercoagulable states in young men with premature peripheral atherosclerosis: A prospective, controlled analysis. J Vase Surg 1996; 23:53-61.
- Widmann MD, Sumpio BE. Lipoprotein (a): A risk factor for peripheral vascular disease. Ann Vase Surg 1993; 7:446-451.
- Cheng SW, Ting AC,Wong J. Lipoprotein (a) and its relationship to risk factors and severity of atherosclerotic peripheral vascular disease. Eur J Vase Endovasc Surg 1997; 14:17-23.
- Sofi F, Lari B, Rogolino A, et al. Thrombophilic risk factors for symptomatic peripheral arterial disease. J Vase Surg 2005; 41:255-260.
- Tseng CH. Lipoprotein(a) is an independent risk factor for peripheral arterial disease in Chinese type 2 diabetic patients in Taiwan. Diabetes Care 2004; 27:517-521.
- Kraft HG, Lingenhel A, Koehl S, et al. Apolipoprotein(a) kringle IV repeat number predicts risk for coronary heart disease. Arterioscler Thromb Vase Biol 1996; 16:713-719.
- Kronenberg F, Kronenberg MF, Kiechl S, et al. Role of lipoprotein(a) and apolipoprotein(a) phenotype in atherogenesis: Prospective r4u lts from the Bruneck study. Circulation 1999; 100:1154-1160.
- Marcovina SM, Albers JJ, Wijsman E, et al. Differences in Lp(a) concentrations and apo(a) polymorphs between black and white Americans. J Lipid Res 1996; 37:2569-2585.
- Paultre F, Pearson TA, Weil HF, et al. High levels of Lp(a) with a small apo(a) isoform are associated with coronary artery disease in African American and white men. Arterioscler Thromb Vase Biol 2000; 20:2619-2624.
- Kostner GM, Gavish D, Leopold B, et al. HMG CoA reductase inhibitors lower LDL cholesterol without reducing Lp (a) levels. Circulation 1989; 80:1313-1319.
Author Info
D Sangeetha and V Padma*
Department of General Medicine, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: D Sangeetha, V Padma, Plasma Role of Inflammatory Markers as a Predictor of Peripheral Vascular Disease in Chronic Asymptomatic Diabetic Patients, J Res Med Dent Sci, 2021, 9 (5):264-270.
Received: 06-May-2021 Accepted: 24-May-2021
