Research - (2020) Advances in Dental Surgery
Role of Serum β Trace Protein and Neutrophil Gelatinase Associated Lipocalin in Early Diabetic Nephropathy in Type 2 Diabetes of Iraqi Patients
Sajjad K Shael1*, Manal K Rasheed1 and Sabah M Saeedi2
*Correspondence: Sajjad K Shael, Department of Clinical biochemistry, College of Medicine, University of Baghdad, Iraq, Email:
Abstract
Background: Diabetic nephropathy (DN) is part of the greatest broadly known diabetic microvascular intricacies inducing around 40% of patients with type 2-diabetes Mellitus (T2DM), Its advancements to end-stage renal disease (ESRD); the primary recognition of DN can be achieved with biomarkers of diabetes. This study evaluates the role of the power of the early biomarker recognition of DN in the T2DM serum. Design and Methods: A case-control study, it included 90-people, and composed from both genders and age range of individual study was (40-69 years); which divided into 3-groups by using the urinary albumin/ creatinine ratio (ACR). Included 60-patients with T2DM without/with proteinuria, which also divided into 2-groups group I, normoalbuminuria (<30 mg/g) and group II, microalbuminuria (30–300 mg/g); Addition to 30-persons, healthy control group (<30 mg/g), (free from any disease); the assay was applied by turbidimetric/ biochromatic rate. In all groups, β-TP and NGAL which were estimated in serum and both biomarkers having the same methodology by quantitative enzyme immunoassay, (double-antibody sandwich). Results: The serum β-TP and NGAL have significantly higher levels in diabetic patients with microalbuminuria (group II) as parallel with those with normoalbuminuria (group I) and healthy control, nevertheless their levels have no significant variance between group I and healthy control subjects. Conclusions: Results of this suggest that serum β-TP and NGAL in diabetic patients with type 2, can be considered a valuable biomarker for early detection of DN.
Keywords
Type 2-diabetes mellitus, Diabetic nephropathy, β-trace protein, Neutrophil gelatinase-associated lipocalin
Introduction
Diabetic nephropathy (DN) is part of the greatest broadly known diabetic microvascular intricacies inducing around 40% of patients with type 2-diabetes Mellitus (T2DM), Its advancements to end-step renal disease; in this way affecting the sickness and death of T2DMpatients [1]. Efficient DN treatment includes glycemic management and lowering blood pressure (BP). It's essential to identify DN within early stages as brief treatment can reduce the medical and economic burden of this sickness. At present, microalbuminuria is the most generally explored biomarker for the conclusion of DN; but its indicative value in beginning period DN is constrained as renal injury ordinarily goes before proteinuria. Consequently, there is a desperate requirement for progressively delicate and explicit biomarkers used for finding of DN in early process. It's been nice -hence this leads to glomerular distress, tubular injury, inflammatory reactions and oxidative stress advancement diabetic kidney illness [2].
Beta-trace protein (β-TP) also, Prostaglandin D-type lipocalin synthase (L-PGDS) [3] can be viewed as a protein with a twofold function: First, it works as an enzyme in the creation of PGD2 [4] by this enzyme advances the change of Prostaglandin H2 (PGH2) to prostaglandin D2 (PGD2) [3] and second, after being excretion, it works as an extracellular transporter because of its lipophilic nature. The β-TP is a low molecular mass glycoprotein and a novel endogenous marker of GFR [5]. It is freely filtered by the glomerulus without secretion or potentially reabsorption in renal tubules and it is excreted by through the kidneys. Elevated the β-TP concentrations in serum reflect diminished clearance of the protein. β-TP half-life is around 1-2 hours and there is minimal extrarenal clearance [6]. In this manner, serum β-TP has been projected as a marker of GFR in both kids and grown-ups [7]. Then again, the investigating of studies Sβ-TP by way of a dependable biomarker in T2DM of renal dysfunction are still exceptionally rare. additionally, there is a paucity of information on the estimation of Serum β-TP in various phases of nephropathy in T2DM patients [8]. In 2004, Kobata et al. [9] recommended that β-TP may foresee the beginning stages of CKD in T2DM-patients.
The Neutrophil Gelatinase-Associated Lipocalin (NGAL) is an individual from the lipocalin protein family. This family incorporates numerous little proteins, the vast majority of which go about as transporters, fundamentally for lipophilic substances. In any case, different jobs for these proteins have been found, for example, the regulation of cell division, differentiation, cell-cell adhesion, and cell survival. The NGAL is utilized as a renal injury biomarker because launch it is quickly as the response of tubular damage [10]. Curiously, among the most encouraging tubular biomarkers in the assessment of acute and chronic renal disease is NGAL, a small protein (25 kDa) estimated in both serum and pee, having a place with the lipocalin protein superfamily and created in renal tubules upon inflammation and tissue injury [11]. It is revealed inside 2-4 hours of renal injury, even before the albumin appearance in the urine [12]. Serum NGAL increments in the early stage of DN and drops down as the ailment progressive. In another word, Serum NGAL relates inversely with the amount of albuminuria [13]. In this study, we evaluate the role of early detection power of serum biomarkers for finding of diabetic nephropathy in T2DM-patients.
Topics and Practices
Topics
This case-control study included 90-subjects as total with age ranging between (40-69 years): 60-patients with T2DM, divided equally into 2-groups, 30-patients-Microalbuminuria (group I) and 30-patients-Normoalbuminuria (group II), in addition to 30-persons-Healthy (control group) were selected as a healthy person during the period from November 2019 to December 2019, the permission to do the research was obtained by the college in consultation unit of diabetes with the laboratory of biochemistry in Al-Zahra teaching hospital in Wasit/ Iraq. T2DM was diagnosed according to criteria of DM, when fasting blood glucose (FBG) level of 126 mg/ dL (7.0 mmol/L) at Alternatively blood sugar Around 200 mg/dL (11.1 mmol/L)) or greater in patients with classic hyper blood glucose symptoms or Hemoglobin A1C at just over 6.5 per cent [14]. Accordingly, a suitable regulator of T2DM was well-defined as (HbA1C <6.5%), while HbA1C levels (>6.5%), were used to categorize patients as those with the inadequate regulator of the disease; The grade This was calculated from early DN using the greatest usually used clinical index ACR: (30–300 mg/g) and GFR, estimated using the formulary of chronic kidney diseased epidemiological collaboration (CKDEPI)) [15].
CKD-EPI eGFR = 141 × min (SCr / κ, 1) α × max (SCr / κ, 1)-1.209 × 0.993age [× 1.018 (if female)] or [× 1.159 (if black)]
where: SCr in μmol/l, κ is 61.9 for females and 79.6 for males, α is -0.329 for females and -0.411 for males, min indicates the minimum of SCr/κ or 1, max indicates the maximum of SCr /κ or 1.
The study has approval from the moral committee at the College of Medicine, Baghdad University. Informed consent was attained from each contributor. Both patients and healthy-controls are free from CVD (acceptable within six months), hematological diseases, endocrine illnesses, glucocorticoid Therapy, pregnancy, tumors, acute infections, continuing inflammatory sickness and renal disease other than DN (diabetic patients with macroalbuminuria were excluded from the study).
Biochemical assessments
About 6 ml of blood samples were obtained from veins of healthy control subjects and patients having T2DM obtained from each fasting (8 hours fast) participant in this study. Each blood samples divided into two parts:
A) First, part 2.5 mL of whole blood retained in ethylenediaminetetraacetic acid (EDTA), tubes for measuring of glycated haemoglobin (HbA1C%) by measuring a boronated affinity assay by using NYCOCARD reader II.
B) Second part 3.5 mL of blood were left for 30 min at temperature of room allow samples to clot in plain tube. After coagulation, sera were separated by centrifugation for 10 min at 3000 rpm. Sera were aspirated and divided into two aliquots in eppendorf tubes for: -
i. Aliquot 1: Immediate measurements of fasting blood sugar (FBG), uric acid (UA), serum creatinine (SCr), blood urea (Urea), serum triglycerides (TG) and serum high-density lipoprotein-cholesterol (HDL-C) were done using assay (colourimetric); and the assay was applied by the automated method by using Abbott Architect C4000.
ii. Aliquot 2: The rest were stored at (-55 to -65 Cº) until assayed for β-TP and NGAL and both biomarkers having the same methodology by quantitative enzyme immunoassay (doubleantibody sandwich) was measured by an enzyme-linked immunosorbent assay (ELISA) manufactured by (Melsin medical co., limited, china).
About (5-10 ml) of freshly voided morning urine samples were collected into a sterile container and divided into two aliquots.
Aliquot 1: used for general urine examination which includes macro-examination using urine strip kit supplied by Human diagnostics, and microscopic examination to exclude urinary tract infection (UTI).
Aliquot 2: The grade this was calculated from early DN using the greatest usually clinical indices used ACR, the assay was applied by turbidimetric/biochromatic rate and the automated method by using the Dimension clinical system of chemistry.
An analysis of statistics
Analysed results using SPSS V 23. Descriptive statistics (Mean ± SD with tables and figures) and inferential statistics (Chi-square, ANOVA, the multivariate linear regression, and operating receiver curve (ROC)/ Area below Curve (AUC), responsiveness and specificity have been established. used. Statistically important was the Price P of 0.05.
Results
In the Table 1 showed the clinical features of the three research groups. All study groups were identical regarding age, sex, BMI, serum uric acid, urea, creatinine and eGFR. While other variables like systolic and diastolic BP, FBG, HbA1c, HDL-C and TGs was varying greatly in both group of diabetic patients vs. healthy test (p<0.01). However, there was no sizeable difference regarding FBG, HbA1c, HDL-C and TGs for the team I and group II (p>0.05). The systolic and diastolic BP were significantly different in diabetic patients of both groups as compared with the healthy control.
Based on the description of hypertension according to 2017 Core of American society/Guidelines for the American college of cardiology, T2DMPatients- Microalbuminuria were significantly more hypertensive when compared with T2DMPatients- Normoalbuminuria and healthy control [16]. The study also showed that serum NGAL rates were substantially elevated in the group II patients as compared to group I and healthy controls, while the levels of β-TP were big increased in both collections of diabetics as Safe monitoring contrasted, with significantly higher group II levels as a group I levels (p<0.01).
The Person correlation coefficient between Serum β-TP and NGAL biomarkers in diabetic patients with all group studied were listed in the Table 2.
In this table, the biomarkers have correlations with each other. In all studied subjects (patients and healthy control) β-TP, NGAL and ACR were found to be significantly correlated with each other (P<0.001), while within the group of diabetic patients (normoalbuminuria and microalbuminuria) β-TP was significantly correlated with NGAL (P<0.04) and ACR (P<0.002), Still, and NGAL was more associated with the ACR (P<0.001). There was no significant correlation among β-TP, NGAL and ACR in subjects without nephropathy (normoalbuminuria and healthy control).
In the Table 3, ROC curve for assessment of β-TP and NGAL in T2DM-Patients for diagnosis of early-stage DN. Serum β-TP produced an AUC of 0.764 (95% CI, 0.646–0.883; P<0.001). The top value cut-off of β-TP was used for early detection DN is 635 ng/ml with sensitivity 56.7%, specificity 83.3%, PPV 77.3%, NPV 65.8% and accuracy 70%.
Serum NGAL produced an AUC of 0.957 (95% CI, 0.891–1.000; P<0.001). The top value cut-off of NGAL was used for early detection DN is 77.8 ng/ml with sensitivity 93.3%, specificity 96.7%, PPV 96.6%, NPV 93.5% and accuracy 95%.
Combined β-TP and NGAL has an AUC of 0.954 (95% CI, 0.902–1.000; P<0.001) with sensitivity 50% and specificity 100%, with PPV 100% and NPV 66.7%, and accuracy 75%.
To determine the efficiency of (β-TP, NGAL, β-TP with NGAL, and ACR) in early detection of DN, the most sensitive biomarkers for the early stage of DN is NGAL (Sensitivity 93.3%), followed by β-TP (Sensitivity 56.7%). While the combination of both β-TP and NGAL has a sensitivity of 50% but it is highly specific for early detection of DN (Specificity 100%). As described in the Figure 1.
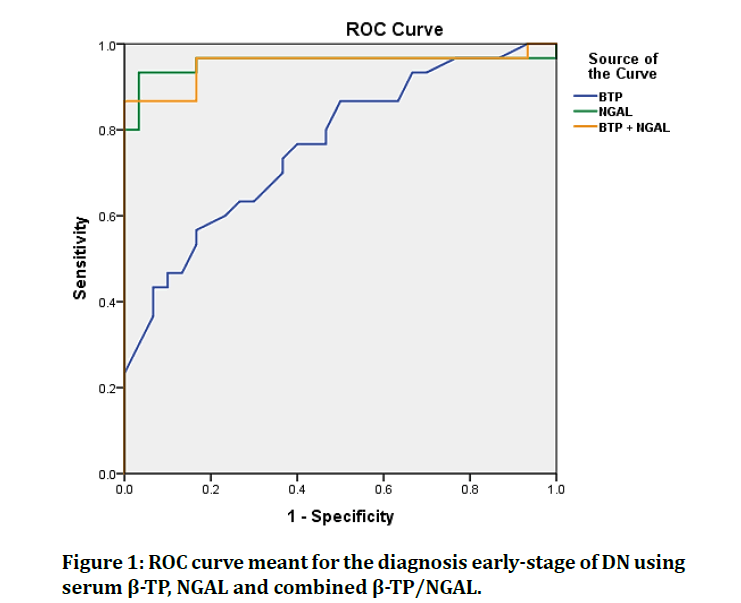
Figure xxxx: ROC curve meant for the diagnosis early-stage of DN using serum ß-TP, NGAL and combined ß-TP/NGAL.
Discussion
Most of the patient with the diabetic illness will create renal infection [17]. Around half of the people with T2DM and 33% of individuals with T1DM create DKD, a microvascular complication that is presently the main source of CKD and ESKRD world [18]. In this academic work, we have tried to create the role of circulating β-TP and NGAL levels in patients with T2DM to predict DN in early-stage even if the kidney function was normal.
There are several mechanisms shared between DM and hypertension, of these abnormal activations of angiotensin aldosterone system, excessive production of reactive oxygen species, sympathetic nervous system activation and abnormal renal sodium handling [19]. In this case-control study, no significant difference was noted in SBP and DBP in diabetic patients with normo- and microalbuminuria, this is in agreement with Motawi et al. [20]. Quite the same, Mahfouz et al. [21] Important disparity found in both SBP and DBP between diabetic patients within normoalbuminuria and microalbuminuria. However, according to the definition of hypertension based on 2017 US College of cardiology/American heart association whelton guidelines Whelton et al. [16], the study showed an elevated frequency of hypertension among others diabetic customers with microalbuminuria compared with normoalbuminuria and group control. The Unified Kingdom potential diabetes schoolwork (UKPDS) found that the hypertension is a significant hazard factor for the advancement of microalbuminuria and retinopathy and powerful systolic pulse control was altogether connected with the diminishing of long-haul complications of DM [22,23].
No substantial difference could be found in the FBG and HbA1C levels between groups of diabetic patients (I, II); while their levels were significantly superior in diabetic patients compared with the control group. Our finding is in an agreement with the Motawi et al. [20]. Other studies showed a significant difference in FBG in patients with microalbuminuria compared with normoalbuminuria Zhang et al. [2] and Mahfouz et al. [21], there is combined proof that diabetic nephropathy is emphatically connected with poor glycemic control [24].
The currently underway study showed lipid patterns the serum has was level from TG was significantly higher in both groups of diabetes than in the control group; HDL-C in diabetics, on the other side, was slightly lower patients' groups compared to the control group. This finding is consistent with other studies of dyslipidemia in diabetic patients Fouad et al. [25]. There is no sizeable difference in TG and HDL-C levels between diabetic patients of both groups, a finding that is inconsistent with what was demonstrated in previous studies Motawi et al. [20] and Zhang et al. [2].
The adjustments in raised degrees of TG and diminished HDL-cholesterol might be discovered quite a while before the beginning of overt diabetes [26]. Albeit low degrees of HDL related with cardiovascular sicknesses, this change is an autonomous hazard factor for the advancement of DM itself [27].
The β-TP is a low-atomic weight glycoprotein and it's currently considered as a novel marker for evaluating GFR. β-TP is predominantly found in cerebrospinal liquid, with lower focuses in serum [28]. It is unreservedly separated by the glomerulus and broadly reabsorbed and debased by the proximal tubule, with just modest quantities discharged in the pee under typical conditions [29]. β-TP helps in transformation of prostaglandin H2 (PGH2) to PGD2 the later assumes a significant job in platelet conglomeration, vasodilation, irritation, adipogenesis, and bone rebuilding [28]. This research revealed that the serum was β-TP level was significantly advanced in diabetic patients compared with control group and the elevation was more pronounced in microthan normoalbuminuria group. this finding is an agreement with Motawi et al. [20] studies which found that β-TP was developed in the DN group compared with a diabetic patient without nephropathy and control. Also, the result is consistent with Hebah et al. [8] that found that the serum of β-TP is higher in diabetic group than the control group which related to kidney dysfunction in T2DM patient as β-TP elimination limited to the kidney.
The NGAL is a 25 kDa protein of 178 amino acids and is predominantly generated in kidney tubules light of structural tumours of the kidneys. As opposed to serum NGAL, creatinine or blood urea nitrogen, is considered a proxy for systemic renal damage [30].
The serum level of NGAL in the current study was increased especially in patients with DN '' microalbuminuria'' compared with diabetic patients without nephropathy ''normoalbuminuria'' and control; Suggesting that the serum NGAL as a tubular injury marker precedes the presence in albuminuria as a glomerular injury marker, the study also found a highly significant difference in serum NGAL levels among the studied groups and was corresponding to the severity on kidney damage and being lower in the healthy control group and increased as ACR increase. Our results are in consent with the Motawi et al. [20] The one who finds the serum levels of NGAL were in T2DM with microalbuminuria group significantly higher than in T2DM with normoalbuminuria and control teams with a strong positive association with DM age and period. Kaul et al. [31] found that diabetes patients with normoalbuminuria had significantly higher levels of serum NGAL than control group suggested that tubular dysfunction in early DN is not secondary to albuminuria. On the other hand, Kim et al. [32] suggested in their trial that differences in NGAL value between control, normoalbuminuria, and microalbuminuria were nonsignificant, contradicting NGAL as an early marker of DN.
Wajda et al. [33], also, found that β-TP a significant correlation with SCr, NGAL and age in a patient with kidney disease. When comparing diabetic patients of both groups with healthy control β-TP, NGAL and ACR were positively correlating with each other. The same correlation also found when a patient with DN was compared with the diabetic patient without nephropathy, suggested that the β-TP and NGAL is a useful and sensible calculation predictor to be interested early of the renal in diabetes.
The ROC curves were used to test the diagnostic efficiency of β-TP and NGAL, and whether they were can be used as diagnostic tools instead of ACR with almost the same sensitivity and specificity of ACR. The present study found that NGAL has more sensitivity and specificity than β-TP in early detecting diabetic patients with nephropathy than β-TP. but when these two biomarkers are combined and used to detect early DN they lead to most specific than each other but they have the lowest sensitivity; these results made NAGL more sensitive and specific than β-TP in the predication of DN. these results made NGAL more useful than β-TP and combined β-TP /NGAL in detecting early DN. These results are in consent with Mahfouz et al. [21] Who noticed that serum NGAL in micro- and macroalbuminuric diabetics increased significantly compared to the control group. Other studies also found comparative results Sueud et al. [34] and Motawi et al. [20]. On the other hand, Kobata et al. [9] stated that there were no big differences in the mean levels of β-TP between diabetic patients with normoalbuminuria and analbuminuria, however, β-TP was a good marker for the identification of early renal dysfunction in type 2-diabetes.
These biomarkers correlate with the developing of renal impairment via changing different concentrations according to the degree of the nephron damage. Part of it's due to its low molecular weight these biomarkers the formed glomerulus is filtered and reabsorbed at the proximal tubule. If the renal tubule is scratched, the reabsorption declines of biomarkers while its creation from epithelial cells increases, resulting in increases their levels in the blood and urine; as it is secreted within a few hours of nephropathic damage, even before glomerular involvement. Therefore, these biomarkers are a promising biomarker to detect DN in the earliest stages.
Conclusion
Through increased levels of serum β-TP and NGAL as endogenous filtration biomarkers in diabetic patients with type 2, it considered as a predictive biomarker which forces linked in early detection of diabetic nephropathy.
References
- Marathe PH, Gao HX, Close KL. American diabetes association standards of medical care in diabetes 2017. J Diabetes 2017; 9:320-324.
- Zhang D, Ye S, Pan T. The role of serum and urinary biomarkers in the diagnosis of early diabetic nephropathy in patients with type 2 diabetes. Peer J 2019; 7:e7079.
- Filler G, Kusserow C, Lopes L, et al. Beta-trace protein as a marker of GFR-history, indications, and future research. Clin Biochem 2014; 47:1188-1194.
- Bacci MR, Cavallari MR, de Rozier-Alves RM, et al. The impact of lipocalin-type-prostaglandin-D-synthase as a predictor of kidney disease in patients with type 2 diabetes. Drug Des Devel Ther 2015; 9:3179-3182.
- Uehara Y, Makino H, Seiki K, et al. Urinary excretions of lipocalin-type prostaglandin D synthase predict renal injury in type-2 diabetes: A cross-sectional and prospective multicentre study. Nephrol Dial Transplant 2009; 24:475-482.
- Urade Y, Hayaishi O. Biochemical, structural, genetic, physiological, and pathophysiological features of lipocalin-type prostaglandin D synthase. Biochim Biophys Acta 2000; 1482:259-271.
- Inker LA, Tighiouart H, Coresh J, et al. GFR estimation using ß-Trace protein and ß2-microglobulin in CKD. Am J Kidney Dis 2016; 67:40-48.
- Hebah HA, Afifi EN, Abd El-Megeid SZ, et al. Beta-trace protein as an early predictor of diabetic nephropathy in type II diabetes. J Egypt Soc Nephrol Transplant 2018; 18:96-102.
- Kobata M, Shimizu A, Rinno H, et al. Beta-trace protein, a new marker of GFR, may predict the early prognostic stages of patients with type 2 diabetic nephropathy. J Clin Lab Anal 2004; 18:237-239.
- Buonafine M, Martinez-Martinez E, Jaisser F. More than a simple biomarker: the role of NGAL in cardiovascular and renal diseases. Clin Sci 2018; 132:909-923.
- Kapoula GV, Kontou PI, Bagos PG. Diagnostic accuracy of neutrophil gelatinase-associated lipocalin for predicting early diabetic nephropathy in patients with type 1 and type 2 diabetes mellitus: A systematic review and meta-analysis. J Appl Lab Med 2019; 4:78-94.
- Assal HS, Tawfeek S, Rasheed EA, et al. Serum cystatin C and tubular urinary enzymes as biomarkers of renal dysfunction in type 2 diabetes mellitus. Clin Med Insights Endocrinol Diabetes 2013; 6:7-13.
- Sharif E, Alwakeel M. Neutrophil gelatinase associated lipocalin: Is not an early marker inductor for diabetic nephropathy in qatari population. Biomed J Scientific Tech Res 2019; 22:16345-16355.
- ADA. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2020. Diabetes Care. 2020; 43:S14-S31
- Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604-612.
- Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. hypertension 2018; 71:e13.
- Nasri H, Rafieian-kopaei M. Diabetes mellitus and renal failure: Prevention and management. J Res Med Sci 2015; 20:1112-1120.
- Alicic RZ, Neumiller JJ, Johnson EJ. sodium–glucose cotransporter 2 inhibition and diabetic kidney disease. Diabetes 2019; 68:248-257.
- Sowers JR, Whaley-Connell A, Hayden MR. The role of overweight and obesity in the cardiorenal syndrome. Cardiorenal Med 2011; 1:5-12.
- Motawi TK, Shehata NI, ElNokeety MM, et al. Potential serum biomarkers for early detection of diabetic nephropathy. Diabetes Res Clin Pract 2018; 136:150-158.
- Mahfouz MH, Assiri AM, Mukhtar MH. Assessment of neutrophil gelatinase-associated lipocalin (NGAL) and retinol-binding protein 4 (RBP4) in type 2 diabetic patients with nephropathy. Biomark Insights 2016; 11:31-40.
- Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): Prospective observational study. BMJ 2000; 321:412-419.
- Sowers JR. Diabetes mellitus and vascular disease. Hypertension 2013; 61:943-947.
- Tuttle KR, Bruton JL, Perusek MC, et al. Effect of strict glycemic control on renal hemodynamic response to amino acids and renal enlargement in insulin-dependent diabetes mellitus. N Engl J Med 1991; 324:1626-1632.
- Fouad M, Fathy H, Zidan A. Serum uric acid and its association with hypertension, early nephropathy and chronic kidney disease in type 2 diabetic patients. J Bras Nefrol 2016; 38:403-410.
- Dean JD, Durrington PN. Treatment of dyslipoproteinaemia in diabetes mellitus. Diabet Med 1996; 13:297-312.
- Abbasi A, Corpeleijn E, Gansevoort RT, et al. Role of HDL cholesterol and estimates of HDL particle composition in future development of type 2 diabetes in the general population: the PREVEND study. J Clin Endocrinol Metab 2013; 98:E1352-E1359.
- White CA, Ghazan-Shahi S, Adams MA. ß-Trace protein: A marker of GFR and other biological pathways. Am J Kidney Dis 2015; 65:131-146.
- Liu X, Foster MC, Tighiouart H, et al. Non-GFR determinants of low-molecular-weight serum protein filtration markers in CKD. Am J Kidney Dis 2016; 68:892–900.
- Papadopoulou-Marketou N, Skevaki C, Kosteria I, et al. NGAL and cystatin C: Two possible early markers of diabetic nephropathy in young patients with type 1 diabetes mellitus: one year follow up. Hormones 2015; 14:232–240.
- Kaul A, Behera MR, Rai MK, et al. Neutrophil gelatinase-associated lipocalin: As a predictor of early diabetic nephropathy in type 2 diabetes mellitus. Indian J Nephrol 2018; 28:53-60.
- Kim SS, Song SH, Kim IJ, et al. Clinical implication of urinary tubular markers in the early stage of nephropathy with type 2 diabetic patients. Diabetes Res Clin Pract 2012; 97:251-257.
- Wajda J, Dumnicka P, Sporek M, et al. Does beta-trace protein (BTP) outperform cystatin c as a diagnostic marker of acute kidney injury complicating the early phase of acute pancreatitis? J Clin Med 2020; 9:205.
- Sueud T, Hadi NR, Abdulameer R, et al. Assessing urinary levels of IL-18, NGAL and albumin creatinine ratio in patients with diabetic nephropathy. Diabetes Metab Syndr 2019; 13:564-568.
Author Info
Sajjad K Shael1*, Manal K Rasheed1 and Sabah M Saeedi2
1Department of Clinical biochemistry, College of Medicine, University of Baghdad, Iraq2Nephrology and Dialysis Center, Wasit Health Directorate, Iraq
Citation: Sajjad K Shael, Manal K Rasheed, Sabah M Saeedi, Role of Serum ? Trace Protein and Neutrophil Gelatinase Associated Lipocalin in Early Diabetic Nephropathy in Type 2 Diabetes of Iraqi Patients, J Res Med Dent Sci, 2020, 8 (7): 526-533.
Received: 03-Nov-2020 Accepted: 19-Nov-2020 Published: 28-Nov-2020
