Research - (2020) Advances in Dental Surgery
Role of Vitamin D in Bronchial Asthma in Eastern India: A Case Control Study
Manjit Kumar Dhrubprasad1, Rakhi Sanyal1, Sagnik Dutta Sarma2, Uma Mohan3, Goutam Dutta Sarma4* and Ratneswar Bhattacharyya1
*Correspondence: Goutam Dutta Sarma, Department of Obstetrics & Gynaecology, ICARE Institute of Medical Sciences and Research, Haldia, Purba Medinipur, West Bengal, India, Email:
Abstract
Background: Thus the aim of our study was to study the role of serum vitamin D levels between asthmatic and non-asthmatic subjects in Eastern India and its role in the development of bronchial asthma. Materials & Methods: Approximately 5 ml venous blood samples were obtained from the patients as well as controls. Non-fasting serum samples of control and asthma subjects were analyzed for routine biochemical parameters immediately after collection while aliquots of the samples were also stored at - 200 C for the assay of 25-hydroxyvitamin D or IgE. 25-hydroxyvitamin D or IgE was assayed by using commercially available immunoassay ELISA kits. Results: There was no significant difference in age, sex distribution or BMI in either of the two groups between asthma and control subjects. Moreover, serum 25 OH vitamin D levels were lower in bronchial asthma cases as compared to controls and were statistically significant (12.83 ± 8.44 versus 25.34 ± 7.29 ng/ml; P < 0.001). However, serum IgE level was found significantly higher among bronchial asthma subjects with respect to controls (668.2 ± 247.3 versus 143.8 ± 72.06 IU/l; P < 0.001). Conclusion: Our study has seen drastically decrease in serum vitamin D levels in bronchial asthma and also observed an increase in IgE levels as compared to control subjects. Our study showed higher serum IgE levels in bronchial asthma subjects. There might be a link between total IgE and asthma, which appears to be independent of allergen sensitization.
Keywords
Bronchial asthma, Vitamin D, IgE, Case-control study
Introduction
Bronchial asthma is one of the common chronic diseases known to be the leading cause of morbidity worldwide [1,2]. The common respiratory symptoms include wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation [3]. Hypoxia and hypercapnia is the primary feature of asthma severity. The predominance of asthma is about more than 300 million people in both the developed and the developing countries worldwide. In India, the estimated load of asthma is more than 30 million. The important risk factors linked with asthma includes positive atopic status, exposure and sensitisation to environmental allergens and/or family history of allergic diseases. Vitamin D, a secosteroid stages a pivotal role in calcium or phosphate homeostasis and also a effective modulator of the immune system involved in regulating cell proliferation and differentiation [4]. Epidemiological evidence also suggests that there is a worldwide epidemic of vitamin D insufficiency or deficiency has been linked to severity of bronchial asthma [5,6]. The major factors leading to vitamin D deficiency are poor diet and/or limited sunshine exposure, prolonged breastfeeding without vitamin D supplementation, maternal vitamin D deficiency [7].
Thus, the aim of our study was to study the role of serum vitamin D levels between asthmatic and non-asthmatic subjects in Eastern India and its role in the development of bronchial asthma.
Materials and Methods
The preliminary case-control study consists of 38 bronchial asthma and 36 control subjects of 20 to 67 years of age group attending the Medicine Outpatient Department of a tertiary medical college, Haldia, West Bengal which is a tertiary care hospital in the eastern part of India. The healthy control subjects were age, sex and BMI matched attending the OPD for minor illness with no features of asthma or associated disorders. Informed consent were obtained from control subjects and bronchial asthma patients for the study. The inclusion criteria having a history of asthma with eosinophilia on blood smear present. The study was approved by the Institutional Human Ethics Committee according to Helsinki guidelines. All the healthy control subjects were also examined clinically to exclude any asthmatic symptoms. The exclusion criteria for the study were type 1 diabetes mellitus, protein energy malnutrition (PEM), taking drugs which interferes with vitamin-D metabolism like anti epileptic drugs or received vitamin D either oral/injection in last 6 months and subjects having any chronic liver, kidney or lung or neurological diseases.
Approximately 5 ml venous blood samples were obtained from the patients as well as controls. Non-fasting serum samples of control and asthma subjects were analyzed for routine biochemical parameters immediately after collection while aliquots of the samples were also stored at - 200 C for the assay of 25-hydroxyvitamin D or IgE. 25-hydroxyvitamin D or IgE was assayed by using commercially available immunoassay ELISA kits.
Statistical analysis of different biochemical parameters was performed by Students' t-test. All variables were expressed as mean ± SD (standard deviation). Means obtained from two normally distributed sample groups were compared by Student's unpaired two-tailed “t”- test and for nonparametric Mann-Whitney U “t” test. All statistical analyses were performed by using Graph Pad prism software (version 5, 2007, San Diego, California, USA). Statistical analysis for sex distributions was evaluated by chi-square test by using statistical software STATA (version 8, Copyright 1984–2003, Stata Corporation, Texas, USA).
Results
The demographic profile as well as biochemical profile of the bronchial asthma subjects and healthy controls is depicted in Table 1. There was no significant difference in age, sex distribution or BMI in either of the two groups between asthma and control subjects (Table 1). Moreover, serum 25 OH vitamin D levels were lower in bronchial asthma cases as compared to controls and were statistically significant (12.83 ± 8.44 versus 25.34 ± 7.29 ng/ml; P < 0.001) (Figure 1). However, serum IgE level was found significantly higher among bronchial asthma subjects with respect to controls (668.2 ± 247.3 versus 143.8 ± 72.06 IU/l; P < 0.001) (Table 1).
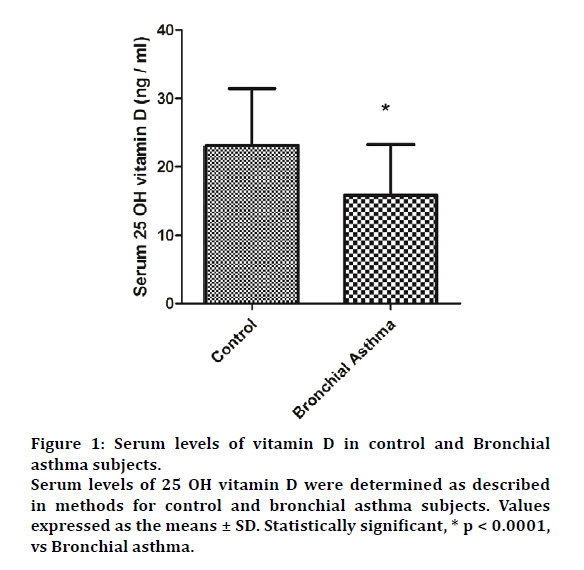
Figure 1: Serum levels of vitamin D in control and Bronchial
asthma subjects.
Serum levels of 25 OH vitamin D were determined as described
in methods for control and bronchial asthma subjects. Values
expressed as the means ± SD. Statistically significant, * p < 0.0001,
vs Bronchial asthma.
| Control (n=36) | Bronchial Asthma (n=38) | |
|---|---|---|
| Age (in years) | 38.64 ± 12.1 | 37.94 ± 11.96 |
| Sex (M/F) | 27-Sep | 28-Oct |
| BMI (kg/m2) | 24.72 ± 1.64 | 25.96 ± 3.92 |
| RBS (mg/dl) | 86.23 ± 11.52 | 82.7 ± 14.22 |
| Serum IgE (IU/L) | 143.8 ± 72.06 | 668.2 ± 247.3* |
RBS: Random blood sugar. Age, BMI, and serum levels of biochemical parameters were expressed as the means ± SD. Statistically significant, * p<0.05 vs. Control.
Table 1: Demographic and biochemical profile of subjects.
Discussion
The deficiency of vitamin D is promising to be a global health problem worldwide due to sedentary lifestyle, poor dietary intake, limited exposure to sunshine, sunscreen use, increased time spent indoors and intrinsic factors such as the skin melanin content and increased cutaneous destruction of vitamin D3. The deficiency of vitamin D is quite common in India in all the age groups. Several studies have randomly reported in the relation of vitamin D deficiency which is associated with an increased incidence of asthma and other allergy symptoms [8]. Some studies have also established vitamin D deficiency as the strongest predictor of asthma or serum IgE levels and familial history of vitamin D deficiency also being a predictor of asthma [3].
Similarly, our study has seen drastically decrease in serum vitamin D levels in bronchial asthma and also observed an increase in IgE levels as compared to control subjects. A more than few mechanisms have been improvised which suggests the modulation of vitamin D in the pathogenesis of asthma. The function of many immune cells including monocytes, macrophages, lymphocytes, and epithelial cells is modulated by vitamin D that serves as a trigger for the deterioration of asthma [9].
A study by Li et al. in 435 asthma patients older than 18 years (268 women and 167 men); showed lower concentration of 25(OH) vitamin D which is similar to our study [10]. Moreover, another study from Shaaban and Hashem investigated serum vitamin D level in 75 adults with asthma and 75 healthy controls older than 18 years which reports the deficiency of vitamin D level which is in affirmation with our study [11]. This may be due to the fact that reduced serum vitamin D levels are associated with increased expression of tumor necrosis factor-α, suggesting that enhanced expression of this proinflammatory cytokine is one potential pathway through which decreased vitamin D levels could exert a proinflammatory effect in asthma [12]. A study in 280 adults with asthma noted that 25(OH)D concentrations in adult asthmatics were lowered in bronchial asthma subjects.They concluded due to the strong correlation between severity of asthma and 25(OH)D concentrations, which suggests an impact of hormonal effects on the asthmatic inflammation or vice versa. Airway epithelia which contains high levels of the enzyme converts circulating 25-OH-vitamin D3 to its active form 1,25-OH-vitamin D3 which has local effects in response to respiratory infections and might dampen the inflammation that is the consequence of these infections [13]. One study also established an association between serum 25(OH) Vitamin-D levels and risk of an asthma related emergency department visit or hospitalization and concluded that vitamin D deficiency may be the strongest predictor of asthma, stronger than familial history of asthma or serum IgE levels [3].
Our study showed higher serum IgE levels in bronchial asthma subjects which is in confirmation with the study by Thirunavukkarasu et al. where they attributed that there might be a link between total IgE and asthma, which appears to be independent of allergen sensitization [14].
These studies indicate that low level of Vitamin D is associated with bronchial asthma in both developed and the developing countries. The severity of Vitamin D deficiency was found to be associated with severity of bronchial asthma. Moreover, vitamin D and total IgE, the degree of atopy and the use of inhaled or oral steroids may be potentially competent of overcoming the poor glucocorticoid responsiveness in severe asthmatics through the upregulation of interleukin-10 production (a potent antiinflammatory cytokine) from CD4+ T cells. Thus, vitamin D may be capable of reestablishment with regulatory T cells from steroid-resistant patients with bronchial asthma to secrete interleukin-10 in response to steroids.
There were few limitations in our study which needs to be mentioned. The sample size of the study was less. Secondly, few of the patients were taking some other drugs such as antihistamines, topical corticosteroids which might interfere with serum vitamin D levels. Despite these limitations it has been observed that serum vitamin D levels were lower and IgE levels were higher in patients suffering from bronchial asthma. However, supplementation of vitamin D may be beneficial and can be considered as an adjuvant therapy in the prevention of the pathogenesis of bronchial asthma. Moreover, a large longitudinal study needs to be done to conclude the fact.
Conflict of Interest
None declared.
References
- Masoli M, Fabian D, Holt S, et al. Global initiative for asthma (GINA) program. The global burden of asthma: Executive summary of the GINA dissemination committee report. Allergy 2004; 59:469–478.
- Moorman JE, Gwynn C, Redd SC. Surveillance for asthma–United States, 1980–1999. Surveill Summ 2002; 51:1–3.
- Davila I, Valero A, Entrenas LM, et al. SIGE Study Group. Relationship between serum total IgE and disease severity in patients with allergic asthma in Spain. J Investig Allergol Clin Immunol 2015; 25:120–127
- Sharma SK, Banga A. Prevalence, and risk factors for wheezing in children from rural areas of North India. Allergy Asthma Proc 2007; 28:647-653.
- Litonjua AA, Weiss ST, Is vitamin D deficiency to blame for the asthma epidemic? J Allergy Clin Immunol 2007; 120:1031–1035.
- Bener A, Kamal A. Growth patterns of Qatar school children and adolescents aged 6–18 years. J Health Pop Nutr 2005; 23:250–258.
- Barday L. Vitamin D insufficiency linked to asthma severity. Am J Respir Crit Care Med 2009; 179:739–742.24
- Sandhu MS, Casale TB. The role of vitamin D in asthma. Ann Allergy Immunol 2010; 105:191–199.
- Freishtat RJ, Iqbal SF, Pillai DK, et al. High prevalence of vitamin D deficiency among inner city African American youth with asthma in Washington, DC. J Pediatr 2010; 156:948-952.
- Li F, Peng M, Jiang L, et al. Vitamin D deficiency is associated with decreased lung function in Chinese adults with asthma. Respiration 2011; 81:469–475.
- Shaaban MM, Hashem M. Serum 25 hydroxy vitamin D levels in adult asthmatic patients. Egypt J Hosp Med 2012; 49:946–952.
- Mora JR, Iwata M, von Andriano UH. Vitamin effect on the immune system: Vitamin A and D centre stage. Nat Rew Immunol 2008; 8:685–698.
- Hansdottir S, Monick MM, Hinde SL, et al. Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. J Immunol 2008; 181:7090–7099.
- Thirunavukkarasu S, Mysore S, Chickballapur R, et al. Evaluation of serum immunoglobulin E levels in bronchial asthma. Lung India 2010; 27:138–140.
Author Info
Manjit Kumar Dhrubprasad1, Rakhi Sanyal1, Sagnik Dutta Sarma2, Uma Mohan3, Goutam Dutta Sarma4* and Ratneswar Bhattacharyya1
1Department of General Medicine, ICARE Institute of Medical Sciences and Research, Haldia, Purba Medinipur, West Bengal, India2Resident Medical Officer, Critical Care Medicine, AMRI Hospitals – Saltlake, KB 24, KB Block, Sector III, Salt Lake City, Kolkata, West Bengal, India
3Resident Medical Officer, Bindubasini Nursing Home, 76, Madhusudan Banerjee Road, Pratiraksha Nagar, Birati, Kolkata, West Bengal, India
4Department of Obstetrics & Gynaecology, ICARE Institute of Medical Sciences and Research, Haldia, Purba Medinipur, West Bengal, India
Citation: Manjit Kumar Dhrubprasad, Rakhi Sanyal, Sagnik Dutta Sarma, Uma Mohan, Goutam Dutta Sarma, Ratneswar Bhattacharyya, Role of Vitamin D in Bronchial Asthma in Eastern India: A Case Control Study, J Res Med Dent Sci, 2020, 8 (7): 318-321.
Received: 09-Oct-2020 Accepted: 29-Oct-2020 Published: 05-Nov-2020
