Research - (2022) Volume 10, Issue 3
SEM Mediational Model of Traumatic Stress Symptomatology in Covid-19 Fear and Insomnia in University Students
*Correspondence: Cristian Ramos-Vera, Universidad Cesar Vallejo. Lima, Peru, Email:
Abstract
During the COVID-19 pandemic, sleep patterns may be altered in the absence of clear routines, due to the threat of latent risk of infection, symptoms of fear and stress that affect sleep quality and favor the development of sleep disorders are strengthened. The aim of this study was to evaluate the mediating role of traumatic stress between fear of COVID-19 and insomnia during the COVID-19 pandemic in university students in the Peruvian city of Metropolitan Lima. Observational, quantitative and predictive study. The research sample consisted of 469 university health students, of whom 244 (52%) were women aged 18 to 26 years (median age=23.36). Structural Equation Modeling (SEM) was applied as a statistical technique for mediation analysis. The results show adequate fit indices of the SEM mediational model, where the relationships between the study variables were significant. The indirect pathway of traumatic stress between fear of COVID-19 and insomnia presented practically significant indirect effects for clinical research (
Keywords
Traumatic stress, Fear, Insomnia, COVID-19, Mental health, College students, Structural equation modeling
Introduction
In the current pandemic context, young university students are more exposed to high levels of stress that affect their physical and mental health [1], and a greater threat to their lives due to the risk of infection by COVID-19. The World Health Organization considers that any sudden and catastrophic event that affects people's health is considered a disaster [2]. As referred to, the COVID-19 pandemic is a disaster for many given the great risk of constant threat of mortality and morbidity, where the consequent measures of social distancing and self-isolation reinforce negative symptoms in mental health [3].
Studies report that the consequences of social restraint health measures can alter cognitive, cardiovascular, and neuroendocrine function, leading to sleep problems and negative traumatic symptoms [4,5]. There has been an increase in recent research reporting sleep disorders because of the current pandemic [6,7]. Also, there is an increased prevalence of comorbidity in the symptomatology of psychological distress, stress, and fear due to COVID-19 [3,5]. Affecting many vulnerable groups including college students [8,9]. University students face new challenges in coping and adapting to a new lifestyle given the change in academic responsibilities due to the closure of universities and online teaching, added to the limitation of personal and social life management due to the alteration of daily activities and insecurity about personal and family health.
Fear is one of the most natural emotions that are produced when faced with a real or perceived threat and present physiological symptoms such as muscle stiffness or accelerated breathing [10]. This emotional concept is one of the most common psychological phenomena in the current pandemic associated with the presence of anxious, depressive and stressful symptoms [5], which reinforces the development of emotional problems in people with greater psychological vulnerability.
Greater manifestations of fear have been reported in people given the perception of the prevalence of latent threat of infection, which can alter mood, physiological arousal, and reactivity to external stimuli, generated by the abundant and saturated information related to COVID-19 disseminated by social networks, which reinforces greater uncertainty and fear of infection by COVID-19 [11]. The combined effect of misinformation and fear generates a growing mistrust that can lead to the development of COVID-19 stress disorder [12].
Stress is a type of negative emotional experience linked to other physiological, biochemical, behavioral and cognitive responses, stress is consequent to various reactions of a physical, social or psychological nature [13]. The risk of stress is greater in the face of unpredictable and uncontrollable events; given the current threat to physical health from the pandemic, higher levels of perceived stress have been reported in conjunction with anxiety and depression [5,12].
Unpredictable stressors tend to alter sleep quality [13], previous studies report that a higher degree of perceived stress results in poorer sleep quality [14,15], therefore, stress can be considered as an essential component in the development of sleep disorders [16]. Students of health sciences usually present rumination or excessive worry before the completion of tasks and exams that affect sleep deprivation and are more vulnerable to develop chronic insomnia [17].
Insomnia is referred to as the unsatisfied experience given the quality or duration of sleep that impacts the person's daily activities [18], this phenomenon is more concurrent in subjects with an excessive level of stress, who present a destabilization in physical functioning and mental state with alterations in the rhythm and duration of sleep [19].
Currently, many university students present concerns about the complications of graduation and job search given the job instability generated by the COVID-19 pandemic, which leads to a greater psychological burden and vulnerability that in turn leads to decreased sleep [20]. This reduces the ability to cope with personal and social needs, and also produces variations in the emotional state and affects bodily responses such as sleep duration [21]. Therefore, the present study seeks to evaluate the mediating role of stress between COVID-19 fear and insomnia in Peruvian university students of health sciences.
Materials and Method
The present study is observational, quantitative, and predictive. The research sample consisted of 469 Peruvian university students, of whom 244 (52%) were women aged 18 to 26 years (Median=23.36, SD= 2.26). Those who studied health science careers such as nursing, nutrition, psychology, etc. were included. The sample data meet the requirements given the a priori power analysis with the consideration of anticipating a median effect size of 0.20 due to indirect effects being smaller than direct effects in mediation models, with a power level set at 0.95 and a significant alpha of 0.05. The minimum required size needed to detect a significant effect was 460 participants for the model proposed using structural equation modeling (SEM) [22].
Instruments
A standardized measure for the assessment of traumatic stress was considered using the Impact of Event Scale with Modifications for COVID-19 (IES-COVID19) measure [23]. This measure includes feelings of stress related to the pandemic event composed of 15 items and two dimensions: intrusion and avoidance, a Cronbach's alpha reliability of 0.80 was reported for the general scale, which is based on a Likert option response from 1 to 4 (never to very often).
The variable of fear of COVID-19 was measured with the Fear of COVID-19 Scale (FCV-19S) which refers to seven most common reactions of pandemic fear, grouped in two factors of emotional and somatic reaction, this measure has adequate reliability values in the Peruvian sample composed of five Likert response alternatives [24].
The insomnia variable was evaluated with the Insomnia Severity Index (ISI), a seven-item scale rated by a five-point Likert-type scaling (score from 0 to 4), the Spanish-adapted version with adequate internal consistency values was considered [25].
Statistical analysis and procedures
Questionnaires and age and sex data were administered online given the respective governmental measures of distance and mobility restriction. Participants were recruited using a snowball sampling technique through social networks such as WhatsApp groups, Facebook and Google groups and were encouraged to invite their family and friends to participate in the survey during the months of January and February 2021. It was developed and administered using Google forms, likewise, the participants provided their consent to participate in this research and publish the results. The research was designed in accordance with the ethical principles of the Declaration of Helsinki and was approved by the ethics committee of the Universidad Cesar Vallejo.
The statistical process first considered descriptive statistics, Pearson correlations, confirmatory factor analysis (CFA) for the factorial and correlational validity of the study variables at the latent level, alpha and omega coefficient of the instruments used. The mediation analysis was performed using the SEM multivariate methodology, the mediating models consider a third variable that intervenes in the relationship of the independent and dependent variable (direct effect), this mediating variable allows another causal passage (indirect) that goes from the independent variable to the mediator and from the mediator to the dependent variable. The following criteria were considered: the diagonally weighted least squares estimation technique (DWLS) and fit indices such as SRMR (≤ 0.08), RMSEA (≤ 0.08), CFI and TLI (≥ 0. 90) and the fit measure Chi-square statistic/ degrees of freedom relationship (χ2/gl) where values <3 are optimal in SEM model verification, which have been used in previous research [26]. The open access statistical program JAMOVI was used for the respective statistical analyses.
Results
Descriptive data, reliability and correlation analysis
For the three variables the respective descriptive data of mean and standard deviation were obtained where it highlights higher levels of fear of COVID-19 (Table 1). Likewise, the reliability evidence is adequate ≥ 0.70. Finally, to perform the mediation analysis, it is necessary that the three variables present an adequate correlation (Table 2).
| α | ω | Mean | Standard Deviation | |
|---|---|---|---|---|
| Fear | 0.9 | 0.91 | 3.75 | 0.45 |
| Stress | 0.8 | 0.81 | 2.83 | 0.31 |
| Insomnia | 0.91 | 0.92 | 2.35 | 0.43 |
| Notes: α=alpha coefficient, ω=omega coefficient. | ||||
Table 1: Descriptive data and reliability analysis of the study variables.
| 1 | 2 | 3 | |
|---|---|---|---|
| Fear | - | ||
| Stress | 0.32** | - | |
| Insomnia | 0.24** | 0.42** | - |
| **p< 0.001 | |||
Table 2: Pearson correlations.
A factor analysis of latent variables was applied to determine the factorial and correlational validity of the study measures, whose indicators reported coefficients greater than 0.30 with optimal measures of absolute and parsimonious fit given the study data (Table 3). Subsequently, the mediational model was evaluated, the results refer fit indices of x2/gl=1.73, SRMR= 0.03, RMSEA= 0.03, CFI= 0.98 and TLI= 0.98 that validate the proposed SEM model according to the data.
| Modelo | X2/gl | CFI | TLI | SRMR | RMSEA |
|---|---|---|---|---|---|
| M1 | 1.7 | 0.97 | 0,97 | 0.04 | 0.04 |
| M2 | 1.73 | 0.98 | 0,98 | 0.03 | 0.03 |
| Note: X2/gl=Chi-square on Degree of Freedom, CFI=Comparative Goodness of Fit Index, TLI=Tucker-Lewis Index RMSEA=Root mean square error of approximation, SRMR=Standardized root mean square residual, M1=factorial and correlational model of the 3 variables, M2=mediational model. | |||||
Table 3: Structural equation fit indices of the discriminant and mediational model (n=469).
Figure 1 shows the standardized coefficients that show the significant indirect influence of fear of COVID-19 on perceived stress by COVID-19 (β=0.32), as well as the significant indirect effect of stress on insomnia (β=0.56). While a direct effect was reported between fear of COVID-19 and insomnia (β=0.25) determining the mediating adjustment of perceived stress with a total indirect effect of (β= 0.18) representing in proportion a mediating effect of 42.08% of the overall effect between such variables (β=0.42).
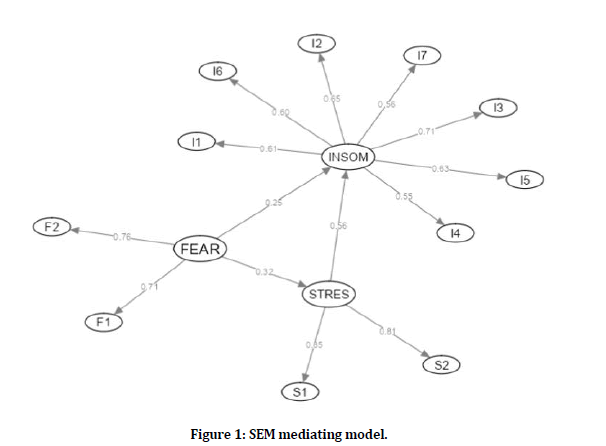
Figure 1: SEM mediating model.
Discussion
Recent research reports an epidemic of insomnia with high prevalence rates worldwide during the COVID-19 pandemic that exacerbate distress and stress symptomatology [27] which may also affect cardio metabolic health [28]. In accordance with the reported antecedents that consider the relationships between variables of negative psychological impact linked to COVID-19 and insomnia were carried out mostly in the Asian continent, according to the literature consulted to date there are no studies in the Latin American context that evaluate relationships between variables related to COVID-19 and insomnia through the methodological rigor of multivariate analysis of SEM. Therefore, stress was considered as a mediating variable in the association between fear of COVID-19 and insomnia. Such a mediating measure is simultaneously positively associated with the other variables. That is, perceived stress was not only an outcome of pandemic fear, but also a catalyst for insomnia, whose measure of effect through the indirect route is of greater magnitude than the direct relationship between fear of COVID-19 and insomnia.
College students may be concerned about the impact of the pandemic on their studies or job search to support their expenses, who may feel disadvantaged by the current situation and may be more vulnerable to developing symptoms of fear and stress [8]. Negative emotions related to distress, perceived threat, and insecurity about the academic and work future produce greater hyperactivity in the brain that makes it difficult to sleep [29]. Such reactions may alter cognition as they produce greater negative appraisal and stress related to sleep problems as referred to in Harvey's cognitive model of insomnia [30].
The literature reviewed indicates that in the pandemic context college students may present difficulties in adaptive coping responses to deal with new situations [8]. Such evidence is demonstrated in recent research that considers the COVID-19 pandemic as a stressful event [1] that can produce sleep disorders such as insomnia in this university group [4,20].
It is important that people can sleep well during the pandemic because those who sleep the necessary hours according to their age are characterized by a higher immunity and defense against viruses and diseases [31], since the circadian system and sleep influence the regulation of immune functions. However, the results obtained reinforce the cross-sectional and longitudinal findings on the relationship of negative psychological reactions to COVID-19 and its effect on sleep quality and duration [32- 35]. These investigations present significant effects of mediating models with respect to the associations of fear and stress by COVID-19 [13,32]. According to a previous study in Pakistani university students that evaluated the relationship of both variables where anxiety and depression measures were included, it was reported that stress unlike anxiety has a greater mediating effect on the relationship of COVID-19 fear and depression [32]. While another research conducted in Bangladesh reported two sexmediated analyses with significant effects in both adult males and females considering stress as a mediator in the relationship of fear of COVID-19 and sleep quality, the results refer that female predict higher ratios of negative psychological impact during the pandemic context [33].
Lin et al. [36] presented a mediation model in Iranian young adults with significant relationships of fear of COVID-19 and insomnia, the latter measure was jointly predicted with the indirect effects of problematic social network use and misinterpretation of COVID-19 information, fear of COVID-19 had a mediating role with higher effect size on insomnia. Another research conducted in Iran evaluated the mediating role of fear of COVID-19 between perceived health status and insomnia whose direct and indirect effects were significant [37]. Such findings refer higher risk of people with fear symptomatology to suffer from insomnia, which has been evidenced by Al Mamun et al. [38] in a nationally representative sample with more than ten thousand Asian participants.
The complex relationship of stress and sleep is reinforced by emotional and somatic symptoms produced by fear, this association produces dysregulation of stress levels that generates stressful chronicity or chronic stress disorder [39,40]. The comorbid finding of stress and insomnia has been demonstrated in thousands of Iranian participants during the pandemic [41]. Even a recent article by Meaklim et al. [27] composed of 2724 adults from 67 countries with the largest number of participants from the United Kingdom, South Africa, Australia, India, and Ireland, showed a stronger relationship of stress with insomnia before and after COVID-19 quarantine. Which noted that the group evaluated without a diagnosis of insomnia after quarantine reported higher levels of stress than those previously diagnosed with insomnia. This comorbid manifestation (stress and insomnia) has been reported in various groups such as adolescents [39], physicians [29], adults [27] and university students [42]. The consequences of stress and fear of COVID-19 may affect the state of well-being, as referred by another quantitative clinical research referring the mediating role of stress between fear of COVID-19 and psychological well-being in 625 Indian university students [43].
It is important to consider other variables that may reduce high levels of such psychological measures during a pandemic. For example, in the study by Casagrande et al. [44], anxiety, traumatic stress, psychological distress and well-being were presented as mediators in the relationship between being infected and having knowledge of people infected by COVID-19 and sleep quality in Italian adults, because despite a greater indirect effect of well-being, it was simultaneously found that traumatic stress had a greater negative role in sleep.
The inclusion of moderating variables may explain the modulation of such symptoms and their association with other measures of negative psychological impact by COVID-19, even in indirect relationships. An example of this is the work done by Zhao et al. [14] on 1630 Chinese adults during the pandemic, who proposed a moderating mediation model, whose results refer a direct effect of stress on sleep quality that was mediated by anxiety, where self-esteem moderates the association between stress and sleep quality, i.e. this association depends on the levels of self-esteem (high or low).
Another recent article refers that Chinese university students present a higher level of stress directly related to high levels of insomnia; such measures reinforce a lower state of security [41]. The negative relationship between perceived security and stress is modulated by family cohesion, where those university students with higher stress and lower security have a lower degree of connection and social support with their family. While students who are more connected with the family present lower stress and higher security status.
According to another moderated mediation study in Nigerian adults, a greater mediating effect of stress symptomatology in contrast to psychological distress was determined in the association of fear and COVID-19 preventive behavior, which included moderating effects of sex that refer to higher relationships of fear and COVID-19 preventive behavior in males [5]. Similarly, another study in Pakistani adults evidenced a total mediating effect of psychological distress between fear of COVID-19 and insomnia [45], where a significant moderate mediation index of mindfulness was reported, where lower mindfulness increases the relationship of fear with distress and insomnia.
Concluding the proposed SEM mediational analysis reports a practically significant indirect effect of traumatic stress on insomnia, and fear of COVID-19 also predicts it directly [46,47] this research is essential for further studies focused on exploring the mechanisms of the development of sleep disorders such as insomnia.
References
- Bridgland VME, Moeck EK, Green DM, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS One 2021; 16:e0240146.
- https://www.who.int/hac/about/definitions/en/.
- Olapegba PO, Chovwen CO, Ayandele O, et al. Fear of COVID-19 and preventive health behavior: Mediating role of post-traumatic stress symptomology and psychological distress. Int J Ment Health Addict 2021; 1-12.
- Martínez-Lezaun I, Santamaría-Vázquez M, Del Líbano M. Influence of Confinement by COVID-19 on the quality of sleep and the interests of university students. Nat Sci Sleep 2020; 12:1075-81.
- Ayandele O, Ramos-Vera CA, Iorfa SK, et al. Exploring the complex pathways between the fear of COVID-19 and preventive health behavior among Nigerians: Mediation and moderation analyses. Am J Trop Med Hyg 2021; 105:701.
- Beck F, Léger D, Fressard L, et al. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res 2021; 30:e13119.
- Jahrami H, BaHammam AS, Bragazzi NL, et al. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J Clin Sleep Med 2021; 17:299-313.
- Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): Impact on education and mental health of students and academic staff. Cureus 2020; 12:e7541.
- Ramos-Vera CA. Las relaciones dinámicas de red de la obsesión y la ansiedad ante la muerte por COVID-19 durante la segunda cuarentena en universitarios peruanos. Rev Colomb Psiquiatr 2021.
- Pappas G, Kiriaze IJ, Giannakis P, et al. Psychosocial consequences of infectious diseases. Clin Microb Inf 2009; 15:743–7.
- Porcelli P. Fear, anxiety and health-related consequences after the COVID-19 epidemic. Clin Neuropsychiatr 2020; 17:103–11.
- Taylor S, Landry CA, Paluszek MM, et al. COVID stress syndrome: Concept, structure, and correlates. Depress Anxiety 2020; 37:706-714.
- Karnatovskaia LV, Johnson MM, Varga K, et al. Stress and fear: Clinical implications for providers and patients (in the time of COVID-19 and beyond). Mayo Clin Proc 2020; 95:2487-2498.
- Zhao X, Lan M, Li H, et al. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Med 2021; 77:339-345.
- Sweetman A, Lovato N, Micic G, et al. Do symptoms of depression, anxiety or stress impair the effectiveness of cognitive behavioural therapy for insomnia? A chart-review of 455 patients with chronic insomnia. Sleep Med 2020; 75:401-410.
- Kalmbach DA, Anderson JR, Drake CL. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res 2018; 27:e12710.
- Azad MC, Fraser K, Rumana N, et al. Sleep disturbances among medical students: A global perspective. J Clin Sleep Med 2015; 11:69-74.
- Morin CM, Drake CL, Harvey AG, et al. Insomnia disorder. Nat Rev Dis Primers 2015; 1:15026.
- Sterling P, Eyer J. Allostasis: A new paradigm to explain arousal pathology. In: Fisher S, Reason J. Handbook of life stress, cognition, and health. John Wiley & Sons; New York 1988; 629–649.
- Marelli S, Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol 2021; 268:8-15.
- Epel ES, Crosswell AD, Mayer SE, et al. More than a feeling: A unified view of stress measurement for population science. Front Neuroendocrinol 2018; 49:146-169.
- Ramos-Vera CA. Beyond sample size estimation in clinical univariate analysis. An online calculator for structural equation modeling and network analysis on latent and observable variables. Nutr Hosp 2021; 38:1310.
- Vanaken L, Scheveneels S, Belmans E, et al. Validation of the Impact of event scale with modifications for COVID-19 (IES-COVID19). Front Psychiatr 2020; 11:e738.
- Ramos-Vera C. Relaciones de red del complejo estigma-discriminación y el miedo a la COVID-19 durante la segunda ola pandémica en adultos peruanos. Rev Colomb Psiquiatr 2021.
- Fernandez-Mendoza J, Rodriguez-Muñoz A, Vela-Bueno A, et al. The Spanish version of the insomnia severity index: A confirmatory factor analysis. Sleep Med 2012; 13:207-210.
- Ramos-Vera C, Serpa Barrientos A, Calizaya-Milla YE, et al. Consumption of alcoholic beverages associated with physical health status in adults: secondary analysis of the health information national trends survey data. J Prim Care Community Health 2022; 13.
- Meaklim H, Junge MF, Varma P, et al. Pre-existing and post-pandemic insomnia symptoms are associated with high levels of stress, anxiety and depression globally during the COVID-19 pandemic. J Clin Sleep Med 2021; 17:2085-97.
- Vgontzas AN, Fernandez-Mendoza J, Liao D, et al. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med Rev 2013; 17:241-254.
- Abdulah DM, Musa DH. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med 2020; 2:e100017.
- Harvey AG. A cognitive model of insomnia. Behav Res Ther 2002; 40:869-893.
- Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch 2012; 463:121-137.
- Kausar N, Ishaq A, Qurban H, et al. Fear of Covid-19 and depression: Mediating role of anxiety and stress among university students. J Bioresource Manage 2021; 8:81-90.
- Siddique RF, Ahmed O, Hossain KN. Relationship between the fear of COVID-19 disease and sleep quality: The mediating role of stress. Heliyon 2021; 7:e07033.
- Zou P, Wang X, Sun L, et al. Poorer sleep quality correlated with mental health problems in college students: A longitudinal observational study among 686 males. J Psychosom Res 2020; 136:e110177.
- De Los Santos JAA, Labrague LJ, Falguera CC. Fear of COVID-19, poor quality of sleep, irritability, and intention to quit school among nursing students: A cross-sectional study. Perspect Psychiatr Care 2021.
- Lin CY, Broström A, Griffiths MD, et al. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interv 2020; 21:e100345.
- Ahorsu DK, Lin CY, Pakpour AH. The association between health status and insomnia, mental health, and preventive behaviors: The mediating role of fear of COVID-19. Gerontol Geriatr Med 2020; 6:e2333721420966081.
- Al Mamun F, Gozal D, Hosen I, et al. Predictive factors of insomnia during the COVID-19 pandemic in Bangladesh: A GIS-based nationwide distribution. Sleep Med 2021;
- Pillai V, Roth T, Mullins HM, et al. Moderators and mediators of the relationship between stress and insomnia: Stressor chronicity, cognitive intrusion, and coping. Sleep 2014; 37:1199-208.
- Fazeli S, Mohammadi Zeidi I, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep 2020; 12: e100307.
- Luo Y, Fei S, Gong B, et al. Understanding the mediating role of anxiety and depression on the relationship between perceived stress and sleep quality among health care workers in the COVID-19 response. Nat Sci Sleep 2021; 13:1747-1758.
- Ye B, Hu J, Im H, et al. Perceived stress and insomnia under the period of COVID-19: The mediating role of sense of security and the moderating role of family cohesion. Psy Ar Xiv 2020.
- Lathabhavan R, Vispute S. Examining the mediating effects of stress on fear of COVID-19 and well-being using structural equation modeling. Int J Ment Health Addict 2021; 1-9.
- Casagrande M, Forte G, Tambelli R, et al. The coronavirus pandemic: A possible model of the direct and indirect impact of the pandemic on sleep quality in Italians. Nat Sci Sleep 2021; 13:191-199.
- De Clercq D, Haq IU, Azeem MU, et al. The link between fear about COVID-19 and insomnia: mediated by economic concerns and psychological distress, moderated by mindfulness. J Manage Org 2021; 1–19. doi: 10.1017/jmo.2021.3. PMCID: PMC7900663.
- Rijnhart JJM, Twisk JWR, Chinapaw MJM, et al. Comparison of methods for the analysis of relatively simple mediation models. Contemp Clin Trials Commun 2017; 7:130-135.
- Igartua JJ, Hayes AF. Mediation, moderation, and conditional process analysis: concepts, computations, and some common confusions. Spanish J Psychol 2021; 49:1–23.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
1Universidad Cesar Vallejo. Lima, Peru2Sociedad Peruana de Psicometria, Lima, Peru
3Universidad Nacional Mayor de San Marcos, Lima, Peru
Citation: Cristian Ramos-Vera, SEM Mediational Model of Traumatic Stress Symptomatology in Covid-19 Fear and Insomnia in University Students, J Res Med Dent Sci, 2022, 10 (3):49-55.
Received: 10-Feb-2022, Manuscript No. JRMDS-22-54104; , Pre QC No. JRMDS-22-54104 (PQ); Editor assigned: 14-Feb-2022, Pre QC No. JRMDS-22-54104 (PQ); Reviewed: 24-Feb-2022, QC No. JRMDS-22-54104; Revised: 28-Feb-2022, Manuscript No. JRMDS-22-54104 (R); Published: 07-Mar-2022
