Research Article - (2025) Volume 3, Issue 3
Shear Bond Strengths of Composite Resin Used to Repair Lithium Disilicate and Feldspathic CAD/CAM Ceramics Treated by Different Lasers (A Comparative in vitro Study)
Ola Mohammed Abdul Kadhim* and Mohammed Rashid Aljuboury
*Correspondence: Ola Mohammed Abdul Kadhim, Department of Restorative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Aim: This study aimed to evaluate and compare the effect of surface treatments with HF acid, Nd:YAG and Er,Cr:YSGG lasers radiation on Shear Bond Strength (SBS) of nano-hybrid composite resin bonded to two different ceramic materials.
Materials and methods: Sixty specimens of (14*12*3 mm) were prepared from ceramic blocks and divided into two groups (n=30) depending on the type of ceramic materials: Group A: Feldspathic ceramic (cerec block CPC 14/A2C; Sirona dental, Germany) and group B: Lithium disilicate (IPS e.max CAD HT/A2; Ivoclar Vivadent, Shann, Liechtenstein). The obtained specimens were further allocated into six subgroups (n=10) according to the surface treatment methods; A1 and B1: 4.5% HF etching, A2 and B2: 3W Nd:YAG laser, A3 and B3: 3W Er,Cr:YSGG laser. Three additional specimens for each group were prepared for SEM analysis. All specimens were repaired with nano-hybrid composite resin (tetric n-ceram) and thermo cycled for 1000 cycles. SBS was measured using a universal testing machine and the failure mode was evaluated by digital microscope. The obtained data were analyzed using two way ANOVA and Bonferroni’s post-hoc tests (P ≤ 0.05).
Results: The highest SBS values were recorded in HF acid treated groups. Two way ANOVA test revealed a statistical significant difference in SBS values among surface treatment groups (p ≤ 0.05). There was a statistical difference between HF acid and both lasers type (p ≤ 0.05); whilst, no statistical difference in adhesion strength was recorded between Nd:YAG and Er,Cr:YSGG lasers (p>0.05). Statistical analysis revealed that ceramic types did not affect SBS values (p>0.05). SEM analysis revealed that HF acid creates pronounced surface alterations in both types of ceramic materials. Fracture pattern analysis showed cohesive failure only in group A1, while adhesive and mixed failures found in the other treated groups.
Conclusion: prior to repairing, 4.5% HF etching provided the more appropriate surface treatment method regarding the bond strength for both ceramic materials. Neither Nd:YAG nor Er,Cr:YSGG lasers irradiation with the used parameters increase the SBS of composite resin to both ceramics compared to HF etching.
Keywords
Shear Bond Strength (SBS), Surface treatments, Nd:YAG and Er,Cr:YSGG lasers, Lithium disilicate, Feldspathic ceramic.
Introduction
The pleasing esthetics and biological properties of currently available all ceramic restorations explain their increasing used in recent years for tooth reconstruction with high quality restorations [1,2]. Furthermore, the improved mechanical properties of all ceramics allowed them are used in restoring single and multiunit tooth defects [3]. In spite of these positive characteristics, chipping and/or fracture are commonly frequented problems associated with ceramic restorations. Various factors such as internal stress, failure at bonding interface, trauma, parafunctional habits, inadequate occlusal adjustment, and internal porosities formed during the production make ceramics fracture unavoidable [4].
The principle to replace or repair the fractured ceramic restoration is influenced by many factors such as fracture type, material properties and cost [5]. The repair of ceramic restorations is divided into direct (intraoral) repair and indirect (extra oral) repair. Indirect repair is not preferred because of additional trauma to the restoration and soft tissue while direct repair is a minimally invasive approach involves addition of a new restorative material to the fracture site [6]. Replacement of the fractured restoration may damage the sound tooth structure and result in increased preparation and restoration size; therefore, intraoral repair serves as a suitable alternative to the restoration replacement [7].
Surface treatments play an important role in repairing process to achieve an optimal bonding between ceramic restoration and resin composite. Surface treatments methods could be chemical (acid etching, silanization) or mechanical (laser irradiation, sandblasting, tribochemical and pyro chemical silica coating) [8]. HF acid etching of ceramic surfaces has been evaluated in several previous studies that are clinically valuable in creating a rough surface and enhancing micromechanical retention via reaction with the silica phase and exposure of crystalline phase. The application of silane coupling agent will increase the surface energy and wettability of etched surfaces and enhance the quality of covalent bonds formation between resin and ceramic materials [9-11]. However, HF acid is highly corrosive, very toxic material that may destroy soft tissues like skin, eyes and weaken the ceramics structure [12,13].
A more biocompatible, convenient, safe and easy method for mechanical surface treatment can be provided by laser irradiation [14]. Nd:YAG laser emits at 1064 nm wavelengths that is well absorbed by water and pigmented tissue, also it can be absorbed by hard tissue and alter surface characteristics. Nd:YAG laser promotes surface roughness by melting and random crystallization that improves bonding between resin and ceramic materials [15]. On the other hand, Er,Cr:YSGG laser operates at 2780 nm wavelengths which is well absorbed by water and hard tissue with least thermal effect on surrounding tissue [16]. Er,Cr:YSGG laser work on a principle of micro explosions during tissue ablation and result in formation of craters and pores which contribute to micromechanical retention.
The purpose of fracture repair is to restore the function and aesthetic of restoration with repair material. Different repairing systems with various conditioning protocols are available in market; however, information about the repair protocol with ceramic repair N system kit is limited. Although many studies exist in the literature related to different surface treatments that are applicable to lithium disilicate [17-19], the evidence of surface conditioning of lithium disilicate by lasers still controversial. In addition, the information about the repair protocols of CEREC blocs CPC remains scarce.
This study aimed to assess and compare the effect of surface treatments by HF acid, Nd:YAG and Er,Cr:YSGG lasers radiation on SBS between nano-hybrid composite resin (Tetric N-Ceram) and two ceramic materials (feldspathic and lithium disilicate glass ceramic). This study tested the null hypothesis as follows:
• SBS between composite resins and ceramics will not
be affected by different surface treatments.
• Type of ceramic material will not affect SBS to
composite resins.
Materials and Methods
Specimen preparation
The manufacturers and compositions of the tested materials used in the present study are summarized in Table 1. A total of 20 ceramic blocks were utilized for specimen preparation using a full diamond disc bur (40 mm diameter and 1mm thickness) that attached to a slow speed hand piece under water cooling. Sixty specimens were obtained (14*12*3 mm) 30 specimens for each ceramic type [20]. Lithium disilicate specimens were crystallized with a VITA VACUMAT 6000M furnace (VITA Zahnfabrik, Germany) following the manufacturer’s recommendations.
| Product | Material | Composition | Group | Block sizes | Manufacturer |
|---|---|---|---|---|---|
| CEREC blocs C PC A2C/14 | Feldspath ceramic CAD/CAM blocks | SiO2 56-64%, Al2O3 20-23%, K2O 6-8%, CaO 0.3-0.8%, TiO2 0.0-0.1% | Group A | 12 × 14 × 18 mm | Sirona dental, Germany |
| IPS e.max CAD HT A2/C14 | Lithium disilicate glass ceramic CAD/CAM blocks | SiO2 57-80%, Li2O 11-19%, K2O 0-13%, P2O5 0-11%, ZrO2 0-8%, ZnO 0-8%, others and coloring oxides 0-12% | Group B | 12 × 14 × 18 mm | Ivoclar Vivadent, Schann, Liechtenstein |
| IPS ceramic etching gel | 4.5% hydrofluoric acid | Ivoclar ivadent; schaan, Liechtenstein | |||
| Ceramic repair N system kit | Mono bond N | Primer; alcohol solution of silane methacrylate, phosphoric acid methacrylate and sulphide methacrylate | Ivoclar ivadent, Schaan, Liechtenstein | ||
| IPS empress direct opaque | Light curing opaque; dimethacrylates, barium glass, ytterbium trifluoride, Ba-Al-fluorosilicate glass and spheroid mixed oxide, initiators, stabilizers and pigments | ||||
| Helio bond | Light curing bonding agent; Bis-GMA, triethylene glycol dimethacrylate, initiators and stabilizers | ||||
| Tetric N-ceram | Light polymerizing nano-hybrid composite; dimethacrylates, barium glass, ytterbium trifluoride, mixed oxide, prepolymer, additives, initiators, stabilizers and pigments | ||||
Table 1: Detailed information of the materials used in this study.
The specimens were then embedded within auto-polymerizing acrylic resin using a custom made cubic silicone mold with internal dimensions of (20*20*15 mm) and round point angles, leaving only one surface uncovered for bonding procedures. Both pre-polishing and high shine burs of EVE rotary grind and polishing instruments (Diasynt Plus and Diapro, Eve Ernst Vetter Zahnfabrik, Germany) were used consequently to obtain a standardized smooth and flat specimen surface under water cooling for 6 minutes.
Surface treatments: The whole surface of each specimen was covered with a white polyethylene tape that has a central hole of 3 mm diameter to control the repairing site after surface treatment [21,22]. The specimens were divided into two groups: Group A (feldspathic ceramic) and group B (lithium disilicate). Accordingly, the specimens within each ceramic group were further assigned into three subgroups (n=10) depending on the applied surface treatments.
Subgroup 1: The specimens were conditioned with 4.5% HF acid (Ivoclar Vivadent, Schaan, Liechtenstein). The etching gel was applied on the demarcated site of the specimen via a disposable brush for 20’s according to the previous investigations [23]. Subsequently, HF acid was rinsed off with distilled water for 2 minutes and thoroughly air dried.
Subgroup 2: The specimens were treated with Nd:YAG laser. The laser beams that were used for surface conditioning is an industrial ytterbium fibre laser with 1046 nm wavelength. The specimen surface was irradiated with 3W output power, 20 Hz repetition rate and 40 μm pulse width [24,25]. The laser beams were delivered perpendicular to the target area at a focal length of 20 cm with circular and horizontal movements and the whole surface was scanned for 10 minutes.
Subgroup 3: The specimens were irradiated with pulsed Er,Cr:YSGG laser (biolase, waterlase, iplus, CA, USA). The laser irradiation was applied at 2780 nm wavelength, 60 μs pulse duration, 10 Hz repetition rate, and 3W output power. A glass tip (MZ6) of 600 μm diameter and 9 μm lengths was fixed to a waterlase iplus/md gold hand piece and held manually by trained practitioner to be perpendicular to the specimen surface. The specimens surfaces were scanned on hard tissue mode at a distance of approximately 10 mm away from the specimen under air/water cooling (65% air and 55% water) for 20’s. After surface treatment, all the specimens were rinsed under distilled water to remove surface residuals water and air dried.
SEM: For SEM analysis, six additional specimens were prepared, one for each surface treatment subgroup. The specimens were gold sputter and scanned under scanning electron microscope (FEI Nova NanoSEM 450, Lincoln). The surface topography of the specimens were observed at 5000X and 20,000X magnification [26]. All examinations on digital SEM images were performed by one blind calibrated examiner.
Restorative procedures: After surface treatments, all specimens were restored using ceramic repair N system kit (Ivoclar Vivadent, Schaan, Liechtenstein). The detailed information of ceramic repair kit is listed on Table 1. A thin coat of Monobond N (Ivoclar Vivadent, Schaan, Liechtenstein) was applied with a brush to the exposed site, allowed it to react for 60’s and then air dried according to instructions [27]. Subsequently, heliobond (Ivoclar Vivadent, Schaan, Liechtenstein) was applied in a thin layer to the entire repairing area using a brush and any excess material was gently removed with compressed air. The adhesives were light polymerized using maxcure curing light unit (maxcure9, guilin refine medical instrument co., China) at 1 mm distance for 10’s according to the manufacturer's instruction. The light intensity of curing unit was tested before use via LED light meter (model LM-1, guilin woodpecker medical instrument Co., ltd, China).The light intensity was set by selecting the normal mode that gives an illumination between 1000-1200 mW/cm2.
The composite restoration (Tetric N-Ceram/A2, Ivoclar Vivadent, Schaan, Liechtenstein) was packed in a single increment (2 mm) and condensed via a suitable instrument to the center of the specimen surface using a custom made teflon mold that held the composite resin over the ceramic specimen in 2 mm height and 3 mm diameter. The central hole of Teflon mold was painted with heytec-moli (Heydent GmbH, Viktor Frankl Str.20, Kaufering, Germany) before fixation of each specimen to prevent the composite resin from sticking to the mold. The composite material then light polymerized for 10’s and the maxcure curing light unit (1000-1200 mW/cm2) was kept in an intimate contact with the with overlying celluloid strips [28].
Afterward, the specimens were stored in deionized distilled water for 24 h at 37°C. Then, all specimens were thermocycled in 5°C and 55°C distilled water baths for 1000 cycles with 30’s dwell time and 5’s transfer time [29].
SBS testing: A computerized universal testing machine (Zwick Roell, Germany) was used for SBS testing. Each repaired specimen was subjected to a shearing force by a stainless steel shearing blade which has knife shape edge (Figure 1). The blade moved as close as possible to the ceramic composite interface with 0.5 mm/mint crosshead speed of until the composite resin delaminated. Then, the shear bond stress was determined by dividing the maximum load (Newton) to the area of bonding surface (mm2) and the final results were expressed in Megapascals (MPa).
Figure 1: Application of shear force to ceramic specimen.
Failure mode analysis: After SBS test, all the fractured specimens were observed under digital microscope (USP digital microscope, model X4, China) to determine the failure types [30]. Failure mode categorizes as follows: Adhesive failure: At ceramic repair material interface where the composite resin is totally removed from specimen surface, cohesive failure: The fracture line was confined either within the ceramics or repairing composite or both and mixed failure: When adhesive and cohesive failures occur simultaneously.
Statistical analysis: Data were evaluated using SPSS version 22 (Chicago, Illionis, USA). Levene test used to evaluate homogeneity of variances. Data distribution was checked using the Shapiro Wilk tests. The effects of surface treatments and ceramic type on SBS were analysed using Two-way (ANOVA) test. Multiple pairwise comparison test was performed using Bonferroni post-hoc test to identify the significant differences among the results. Level of significance was accepted as P ≤ 0.05.
Results
SBS: The mean SBS values and standard deviations of composite resin bonded to ceramic materials treated with different methods are provided in Table 2. In the current study, SBS was evaluated statistically according to ceramic type and surface treatment. In these analyses, generally, there were statistically significant differences among the tested groups in terms of surface treatments (P ≤ 0.05) (Table 3). However, ceramic types had no statistical significant effect on SBS values (P>0.05). Further multiple pairwise comparison test was applied using Bonferroni post-hoc test to identify the significant differences among surface treatments methods for each ceramic group (Table 4). In group A and B, HF etching represented the higher SBS values than the other tested groups. However, generally, in both A and B groups, there were no statistical significant differences in adhesion strength between Nd:YAG and Er,Cr:YSGG lasers treatment (P>0.05). Additionally, SBS values of Nd:YAG and Er,Cr:YSGG lasers etching were statistically lower than those of HF etching (P ≤ 0.05) (Table 5). The lowest SBS value in group A was noted in Nd:YAG laser treatment (11.2 ± 4.3 MPa); while Er,Cr:YSGG laser provide the lowest SBS value for group B (11.7 ± 2.7 MPa).
| Ceramic materials | Surface treatment | Minimum | Maximum | Mean | ± SD |
|---|---|---|---|---|---|
| Group A | A1 | 20.7 | 29.7 | 24.2 | 2.8 |
| A2 | 7 | 17.3 | 11.2 | 4.3 | |
| A3 | 9.7 | 16.7 | 12.9 | 2.6 | |
| Group B | B1 | 18 | 28.1 | 23.2 | 3.3 |
| B2 | 10.6 | 17 | 13.4 | 2.6 | |
| B3 | 8.9 | 15.9 | 11.7 | 2.7 |
Table 2: Descriptive statistics of SBS among surface treatment methods for each ceramic group.
| Ceramic material | Sum of squares | Df | Mean square | F | P value | Partial ETA squared |
|---|---|---|---|---|---|---|
| Group A | 1007.619 | 2 | 503.809 | 51.581 | 0 | 0.656 |
| 527.435 | 54 | 9.767 | ||||
| Group B | 771.349 | 2 | 385.674 | 39.486 | 0 | 0.594 |
| 527.435 | 54 | 9.767 |
Table 3: Two way ANOVA test among surface treatment methods for each ceramic group.
| Ceramic substrate | (I) Surface treatment | (J) Surface treatment | Mean difference (I-J) | P value | |
|---|---|---|---|---|---|
| Group A | A1 | A2 | 13.05 | 0 | Sig. |
| A3 | 11.364 | 0 | |||
| A2 | A3 | -1.686 | 0.233 | NS | |
| Group B | B1 | B2 | 9.83 | 0 | Sig. |
| B3 | 11.49 | 0 | |||
| B2 | B3 | 1.66 | 0.24 | NS | |
Table 4: Multiple pairwise comparisons of SBS among surface treatment methods for each ceramic group.
| Surface treatment | Sum of squares | Df | Mean square | F | P value | Partial ETA squared | |
|---|---|---|---|---|---|---|---|
| HF | Contrast | 5.305 | 1 | 5.305 | 0.543 | 0.464 | 0.01 |
| Error | 527.435 | 54 | 9.767 | ||||
| Nd:YAG | Contrast | 23.981 | 1 | 23.981 | 2.455 | 0.123 | 0.043 |
| Error | 527.435 | 54 | 9.767 | ||||
| Er,Cr:YSGG | Contrast | 6.682 | 1 | 6.682 | 0.684 | 0.412 | 0.013 |
| Error | 527.435 | 54 | 9.767 | ||||
Table 5: Two way ANOVA test among ceramic groups within each surface treatment method.
Bond failure types: The percentages of failure modes analysis of specimens were presented in Table 6 and Figure 2. According to the results, cohesive failures were only observed in A1 group (80%), (Figure 3A and B). B1 and A3 groups showed predominantly mixed failure type (70%), (Figure 3C and D). The failure pattern in A2 and B3 groups was adhesive in nature (70%), (Figure 3E and F). B2 group showed equal percentage of mixed and adhesive failure (50%).
| Group | Subgroup | Adhesive | Cohesive | Mixed |
|---|---|---|---|---|
| Group A | A1 | 10% | 80% | 10% |
| A2 | 70% | 0 | 30% | |
| A3 | 30% | 0 | 70% | |
| Group B | B1 | 30% | 0 | 70% |
| B2 | 50% | 0 | 50% | |
| B3 | 70% | 0 | 30% |
Table 6: Percentages of failure modes occurred with SBS test that determined via digital microscope.
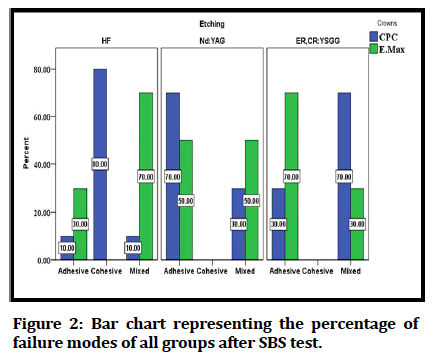
Figure 2: Bar chart representing the percentage of failure modes of all groups after SBS test.
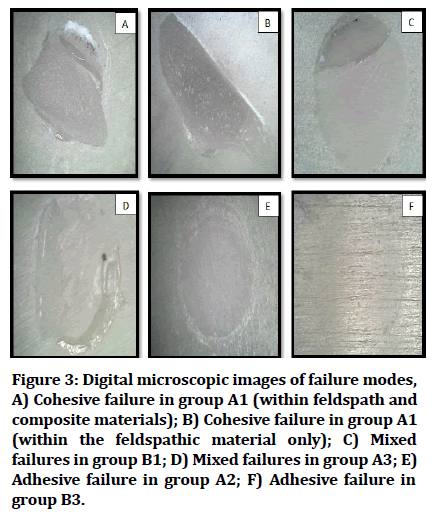
Figure 3: Digital microscopic images of failure modes, A) Cohesive failure in group A1 (within feldspath and composite materials); B) Cohesive failure in group A1 (within the feldspathic material only); C) Mixed failures in group B1; D) Mixed failures in group A3; E) Adhesive failure in group A2; F) Adhesive failure in group B3.
SEM analysis: The representative images of SEM analysis of treated ceramic specimens revealed different surface topography. SEM images are shown in Figures 4 and 5. HF acid produced generalized surface irregularities with formation of micro retentive regions like pits and craters for both ceramic materials; Figures 4 and 5 (A and B). Er,Cr:YSGG laser resulted in minimal pores formation on lithium disilicate surfaces, (Figure 5C and D), whereas Nd:YAG laser create rougher surface with small depressions, (Figure 5E and F). SEM images of E,Cr:YSGG treated feldspathic specimens, (Figure 4C and D), display a surface pattern comparable to Nd:YAG treated specimens, (Figure 4E and F), which shows irregular surface with profound grooves.
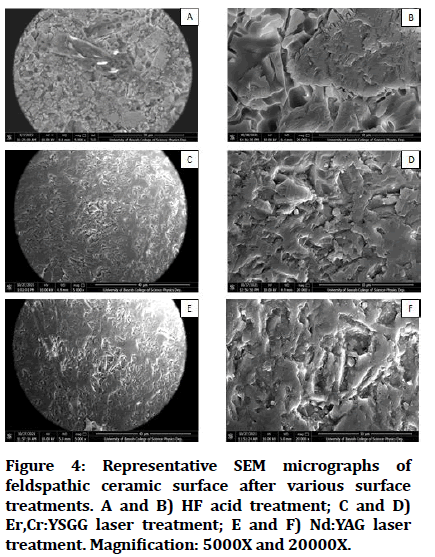
Figure 4: Representative SEM micrographs of feldspathic ceramic surface after various surface treatments. A and B) HF acid treatment; C and D) Er,Cr:YSGG laser treatment; E and F) Nd:YAG laser treatment. Magnification: 5000X and 20000X.
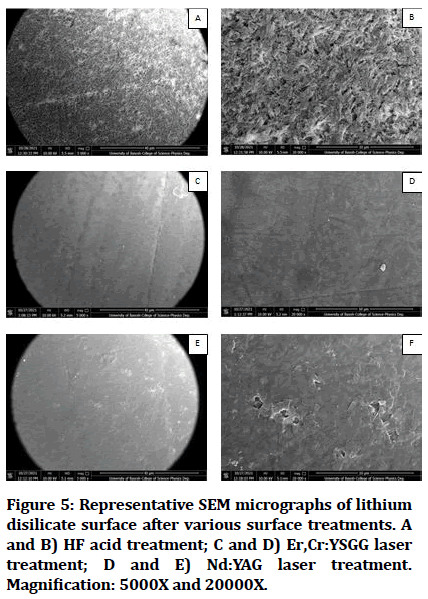
Figure 5: Representative SEM micrographs of lithium disilicate surface after various surface treatments. A and B) HF acid treatment; C and D) Er,Cr:YSGG laser treatment; D and E) Nd:YAG laser treatment. Magnification: 5000X and 20000X.
Discussion
In current in vitro study, the SBS of composite resin to feldspath and lithium disilicate was tested after application of HF acid, Nd:YAG and Er,Cr:YSGG lasers to enhance the reparability of the defective ceramic restoration intra orally using nano-hybrid composite resin. The diverse surface treatments of ceramic materials significantly affect their bonding to composites resin (P ≤ 0.05); thus, the first null hypothesis is rejected. However; the analysed ceramic materials had no significant effect on SBS (P>0.05); therefore the second null hypothesis is accepted.
In the current study, the differences in the SBS values were not statistically significant among the tested ceramic materials (p>0.05). There was no statistical difference in SBS for both HF applied materials although SEM images of them exhibited various characterizations. Several studies suggested that the type of ceramic material and laser energy settings can affect the surface modifications of restorative materials [31]. In contrast, the results of this study showed that different ceramic materials do not affect SBS following Nd:YAG or Er,Cr:YSGG laser surface treatments.
Regarding CEREC blocs C PC investigated in current study; the highest SBS value was recorded in group A1 (24.2 ± 2.8 MPa). This probably due to the fact that HF acid interacts with silica in the glass matrix of feldspathic ceramic and forming hexafluorosilicate [32]. HF acid dissolves the silica phase and causes surface degradation; therefore, bonding agents penetrate into these micro porosities and provide mechanical retention [33].The specimens were etched for 20’s according to a previous study by da Cunha, et al. who used to etch the feldspathic blocks with 5% HF acid for 20, 40, and 60’s and found that the two shorter etching periods may be as effective as the traditional 60’s with regard to the irregularities formation and surface roughness. In addition, Liu, et al. proved that increasing the etching time will reduce the micro hardness, decrease the reliability of resin to ceramic materials, and increase surface roughness due to the dissolution of more silica contents [34].
With the respect to Nd:YAG laser treated feldspathic specimens, the mean SBS was significantly lower than HF treated ones (24.2 ± 2.8 MPa) (11.2 ± 4.3 MPa) respectively. This is in agreement with Bayraktar, et al. study who recorded that HF acid stilled the best surface treatment method for repairing feldspathic ceramic whereas 3 W Nd:YAG and erbium lasers were not recommended. Nevertheless; changing laser parameter may affect SBS. Hosseini, et al. reported that 1.5 and 2W Nd:YAG laser was efficient for feldspathic etching and the level of effect was equalled to or even higher than HF acid [35]. Kara, et al. concluded that low fusing porcelain is affected by 2W Nd:YAG laser to the same level of 5% HF acid [36]. However, Akpinar, et al. concluded that 4W Nd:YAG laser achieved lower bond strength compared with HF and sandblasting [37].
The use of Er,Cr:YSGG laser with the chosen parameters had no significant effect on SBS of composite resin to feldspathic ceramic (p>0.05). This laser produced significantly lower SBS values than HF etchant. These results were in line with Mirhashemi, et al. who reports that erbium lasers are not a suitable alternative to HF etching [38]. However, a study by Kilinc, et al. confirm that 2W Er,Cr:YSGG Laser could be recommended as an alternative method to HF etching for feldspathic ceramics. Another study by Ghavam, et al. concluded that Er,Cr:YSGG laser with 4W power and 140 μs pulse duration has no significant effect on bond strength and produced same results of HF for feldspathic ceramics [39]. In another study, Tokar, et al. concluded Er,Cr:YSGG laser were not enhanced repair bond strength of porcelain regardless of laser pulse rates. According to the above reviewed studies, the effect of laser surface treatment will be a function of pulse energy, output power, irradiation time, the type of adhesive and hand piece movement pattern during irradiation.
The present study also verified the effect of HF acid on lithium disilicate and found that HF applied specimens presented highest SBS values compared to laser surface treatments. Consistent with this result, previous studies concluded that HF etching enhances the bond strength of ceramic materials. However, HF acid could weaken lithium disilicate ceramic by decreasing flexural strength [40]. In the current study, the 4.5% HF acid etchant was applied for 20’s as recommended by previous studies. Puppin-Rontani, et al. found that the adequate surface treatment for lithium disilicate is achieved with the 5% HF for 20’s therefore it is not necessary to use higher HF concentrations and/or increased etching times. By increasing the etching time, roughness values are often increased and the flexural strength significantly reduced [41].
On other hand, the surfaces of lithium disilicate specimens were treated with Nd:YAG laser at 3W energy setting. The results show that Nd:YAG laser produced lower and significantly different bond strength from HF acid (p>0.05). In agreement with this result, Huang, et al. concluded that HF acid stilled the most effective treatment for lithium disilicate and Nd:YAG laser was effective but not a more appropriate method than HF etching. Many studies measured and evaluated different laser parameters and the results were various. Hosseini, et al. measured various output power setting of Nd:YAG laser and concluded that 1.5 and 2W powers can be used appropriately for ceramics surface etching. Alavi, et al. found that 2W Nd:YAG laser beams provided adequate surface treatment for bonding effectiveness for lithium disilicate. Ozdemir and Aladag confirm that 2W Nd:YAG laser was not an effective alternative method for lithium disilicate [42].
Previous studies evaluated erbium lasers in terms of bond strength of lithium disilicate to repairing composites and to resin cement. The results were inconsistent, due to the effect of laser power settings and irradiated materials [43]. In current study, Er,Cr:YSGG laser was applied to the surface of lithium disilicate at an energy level of 3W with 55% water cooling. This laser modifies the surfaces via ablation mechanism. The laser energy absorbed by the water causes vaporization and micro explosions, resulting in formation of surface irregularities [44]. Er,Cr:YSGG laser uses not only endogenous water for ablation but also exogenous water [45]. The results showed that Er,Cr:YSGG laser produced significantly lower bond strength than HF acid (P>0.05). Similarly, a study by Ataol and Ergun confirm that application of 3W laser revealed statistically significant lower bond strength than HF acid for lithium disilicate.
On other hand, previous studies evaluated the efficiency of Er,Cr:YSGG laser with different energy parameters on the lithium disilicate and the results were different. Cengiz-Yanardag, et al. reported that 3W Er, Cr:YSGG laser can be recommended for lithium disilicate while 2W laser treatment had no positive effect on bond strength. Another study by Barutcigil and Kirmali found that HF and 3W Er,Cr:YSGG laser produced an appropriate bond strength for ceramic surface; also, laser irradiation at 1W and 2W promoted surface topography alterations. Kurtulmus-Yilmaz, et al. concluded that Er,Cr:YSGG laser with 2W energy level may be used as an alternative surface treatment method for lithium disilicate. It has been reported that higher power of Er,Cr:YSGG laser irradiation conversely, resulted in weakening and over destruction of the lithium disilicate that decreased the bond strength.
The SEM analysis of HF acid treated feldspath and lithium disilicate revealed formation of grooves, pits and fissures on the specimens surfaces that would improve micromechanical retention with the light polymerized material due to the fact that HF enhances surface roughness that could increase the wettability for an adhesive agent. The SEM images of Nd:YAG lasers treated lithium disilicate showed rather moderate irregularities with mostly a smooth surface; whilst images of Er,Cr:YSGG laser showed a smooth, non-retentive surface with minimal pores formation which may be attributed to the lower bond strength of these groups. These results may be due to the laser irradiation power settings, since only a 3W power setting was used in the present study. On the other hand, the SEM images of group A generally indicated that the effect of laser etching was less effective than HF acid. The surface topography of Nd:YAG treated specimens was comparable to Er,Cr:YSGG treated one. The surface roughness of laser treated groups containing some non-retentive area which may negatively impact bonding.
SBS test used most commonly for measurement of repair bond strength due to the ease of specimen preparation and simplicity of test protocol. Besides, most of stresses related to bond fractures are shear stresses [46]. However; the reliability of shear test is questionable because of non-uniform stress distribution that results in cracks formation and fracture initiation at the interface or the bulk of the material [47]. An adhesion area of 3 mm between composite resin and ceramic material was selected in this study to ensure direct shear load application on the bonded interface since increasing bonding surface area will decrease SBS values [48]. For more clinically relevant results, all the bonded specimens. were aged through a thermo cycling process for 1000 cycles to simulate the thermal changes inside the oral cavity and the other worsening factors that may affect bond strength throughout clinical service.
In the current study, cohesive failure type was the least frequent and detected only within group A1. This is because bond strength between resin and ceramics was greater than the cohesive strength of the ceramics. The adhesive bond failure in A2 and B3 groups occurred at resin ceramic interface, indicating a lack of adequate bond strength between ceramic and repairing composite. B1 and A3 groups exhibited mixed failure at the bonding interface, denoting strong micromechanical bond formation. These results indicated that the laser etching created weaker SBS than HF surface treatments. Usually, cohesive failures were corresponded with improved SBS, whereas adhesive failures were associated with decreased SBS.
This study evaluated only one laser parameter, different concentrations and etching times of HF acid were not used, in addition, the findings of current study presented only on two types of glass matrix ceramic restorations; all considers as limitations of this in vitro study. Further studies are required to evaluate of optical and mechanical properties of ceramics restoration after different surface treatment. As well comparison between different bond strength tests is necessary because the repaired ceramic restorations are subjected to various forces intra orally.
Conclusion
Based on the results obtained and within the limitation of the current study, following conclusions were obtained:
• Prior to bonding, HF acid etchant still the most
effective surface treatment method that provide a
satisfactory repair bond strengths for both tested
ceramics.
• Although Nd:YAG and Er,Cr:YSGG lasers can be used
easily and simply intra orally, the selected laser
parameters in this study could not regarded as an
effective surface treatment method for feldspathic and
lithium disilicate ceramics to establish better repair
bond strength with composite resin.
• The SEM analysis of both ceramic materials provides
images corresponding with SBS values. HF acid
produces more surface irregularities than both laser
types that enhance the SBS.
• Within a specific type of repairing system used in this
study, the type of ceramic materials has no influence
on the repairing bonding strength.
References
- Ozcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater 2003; 19:725-731.
[Crossref] [Google Scholar] [PubMed]
- Borges GA, de Goes MF, Platt JA, et al. Extrusion shear strength between an alumina based ceramic and three different cements. J Prosthet Dent 2007; 98:208-215.
[Crossref] [Google Scholar] [PubMed]
- Kiyan VH, Saraceni CH, Silveira BL, et al. The influence of internal surface treatments on tensile bond strength for two ceramic systems. Oper Dent 2007; 32:457-465.
[Crossref] [Google Scholar] [PubMed]
- Rekow E, Silva N, Coelho P, et al. Performance of dental ceramics: Challenges for improvements. J Dent Res 2011; 90:937-952.
[Crossref] [Google Scholar] [PubMed]
- Gordan VV, Garvan CW, Blaser PK, et al. A long term evaluation of alternative treatments to replacement of resin based composite restorations: Results of a seven year study. J Am Dent Assoc 2009; 140:1476-1484.
[Crossref] [Google Scholar] [PubMed]
- Hickel R, Brushaver K, Ilie N. Repair of restorations criteria for decision making and clinical recommendations. Dent Mater 2013; 29:28-50.
[Crossref] [Google Scholar] [PubMed]
- Kimmich M, Stappert CF. Intraoral treatment of veneering porcelain chipping of fixed dental restorations: A review and clinical application. J Am Denta Assoc 2013; 144:31-44.
[Crossref] [Google Scholar] [PubMed]
- Tian T, Tsoi JK-H, Matinlinna JP, et al. Aspects of bonding between resin luting cements and glass ceramic materials. Dent Mater 2014; 30:e147-e162.
[Crossref] [Google Scholar] [PubMed]
- Grewal Bach GK, Torrealba Y, Lagravere MO. Orthodontic bonding to porcelain: A systematic review. Angle Orthod 2014; 84:555-560.
[Crossref] [Google Scholar] [PubMed]
- Rontani JP, Sundfeld D, Costa A, et al. Effect of hydrofluoric acid concentration and etching time on bond strength to lithium disilicate glass ceramic. Oper Dent 2017; 42:606-615.
[Crossref] [Google Scholar] [PubMed]
- Sundfeld D, Palialol ARM, Fugolin APP, et al. The effect of hydrofluoric acid and resin cement formulation on the bond strength to lithium disilicate ceramic. Braz Oral Res 2018; 32.
[Crossref] [Google Scholar] [PubMed]
- Kursoglu P, Motro PF, Yurdaguven H. Shear bond strength of resin cement to an acid etched and a laser irradiated ceramic surface. J Adv Prosthodont 2013; 5:98-103.
[Crossref] [Google Scholar] [PubMed]
- Lyann SK, Takagaki T, Nikaido T, et al. Effect of different surface treatments on the tensile bond strength to lithium disilicate glass ceramics. J Adhes Dent 2018; 20:261-268.
[Crossref] [Google Scholar] [PubMed]
- Goekce B, Ozpinar B, Dundar M, et al. Bond strengths of all-ceramics: Acid vs. laser etching. Oper Dent 2007; 32:173-178.
[Crossref] [Google Scholar] [PubMed]
- Huang S, Chen L, Liu X, et al. Shear bond strength of three CAD/CAM ceramics treated by Nd: YAG laser and HF. J Adhes Sci Technol 2020; 34:2364-2374.
- Alkhudhairy F, Naseem M, Bin-Shuwaish M, et al. Efficacy of Er Cr: YSGG laser therapy at different frequency and power levels on bond integrity of composite to bleached enamel. Photodiagnosis Photodyn Ther 2018; 22:34-38.
[Crossref] [Google Scholar] [PubMed]
- Ataol AS, Ergun G. Effects of surface treatments on repair bond strength of a new CAD/CAM ZLS glass ceramic and two different types of CAD/CAM ceramics. J Oral Sci 2018; 60:201-211.
[Crossref] [Google Scholar] [PubMed]
- Cengiz-Yanardag E, Kurtulmus Yilmaz S, Karakaya I, et al. Effect of different surface treatment methods on micro shear bond strength of CAD-CAM restorative materials to resin cement. J Adhes Sci Technol 2019; 33:110-123.
- Barutcigil K, Kirmali O. The effect of different surface treatments on repair with composite resin of ceramic. Niger J Clin Pract 2020; 23:355.
[Crossref] [Google Scholar] [PubMed]
- Mandil ST, Katamish H, Salah T. Effect of surface treatment of two ceramic materials by Er, Cr: ysgg laser irradiation on the shear bond strength to resin cement “A comparative in-vitro study”. Braz Dent Sci 2020; 23:1-12.
- Alavi S, Samie S, Raji SAH. Comparison of lithium disilicate reinforced glass ceramic surface treatment with hydrofluoric acid, Nd: YAG, and CO2 lasers on shear bond strength of metal brackets. Clin Oral Investig 2021; 25:2659-2666.
[Crossref] [Google Scholar] [PubMed]
- Kilinc H, Sanal FA, Turgut S. Shear bond strengths of aged and non-aged CAD/CAM materials after different surface treatments. J Adv Prosthodont 2020; 12:273-282.
[Crossref] [Google Scholar] [PubMed]
- Yilmaz SK, Cengiz E, Ongun S, et al. The effect of surface treatments on the mechanical and optical behaviors of CAD/CAM restorative materials. J Prosthodont 2019; 28:e496-e503.
[Crossref] [Google Scholar] [PubMed]
- da Cunha PFJS, Tavares JG, Spohr AM, et al. Examining the effects of acid etching duration on the bond strength between two CAD/CAM materials and one composite resin. Odontol 2022; 110:113-119.
[Crossref] [Google Scholar] [PubMed]
- Bayraktar Y, Arslan M, Demirtag Z. Repair bond strength and surface topography of resin ceramic and ceramic restorative blocks treated by laser and conventional surface treatments. Micros Res Tech 2021; 84:1145-1154.
[Crossref] [Google Scholar] [PubMed]
- Tokar E, Polat S, Ozturk C. Repair bond strength of composite to Er, Cr: YSGG laser irradiated zirconia and porcelain surfaces. Biomed J 2019; 42:193-199.
[Crossref] [Google Scholar] [PubMed]
- Sinaga VR, Bonifacius S, Sumarsongko T. Shear bond strength of two ceramic repair system to lithium disilicate: An in-vitro comparison. Padjadjaran J Dent 2021; 33:139-145. [Crossref]
- Stanislawczuk R, Amaral R, Zander-Grande C, et al. Chlorhexidine containing acid conditioner preserves the longevity of resin dentin bonds. Oper Dent 2009; 34:481-490.
[Crossref] [Google Scholar] [PubMed]
- Morresi AL, D'Amario M, Capogreco M, et al. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing: A literature review. J Mech Behav Biomed Mater 2014; 29:295-308.
[Crossref] [Google Scholar] [PubMed]
- Vohra F, Labban N, Al-Hussaini A, et al. Influence of Er; Cr: YSGG laser on shear bond strength and color stability of lithium disilicate ceramics: An in vitro study. Photobiomodul Photomed Laser Surg 2019; 37:483-488.
[Crossref] [Google Scholar] [PubMed]
- Kara HB, Dilber E, Koc O, et al. Effect of different surface treatments on roughness of IPS empress 2 ceramic. Lasers Med Sci 2012; 27:267-272.
[Crossref] [Google Scholar] [PubMed]
- Soares CJ, Soares PV, Pereira JC, et al. Surface treatment protocols in the cementation process of ceramic and laboratory processed composite restorations: A literature review. J Esthet Restor Dent 2005; 17:224-235.
[Crossref] [Google Scholar] [PubMed]
- Duzyol M, Sagsoz O, Polat Sagsoz N, et al. The effect of surface treatments on the bond strength between CAD/CAM blocks and composite resin. J Prosthodont 2016; 25:466-471.
[Crossref] [Google Scholar] [PubMed]
- Liu D, Tsoi JK-H, Pow EH-N, et al. Influence of different etching protocols on the reliability of resin bonding to CAD/CAM feldspathic porcelain. Int J Adhes Adhes 2015; 62:18-24.
- Hosseini MH, Sobouti F, Etemadi A, et al. Shear bond strength of metal brackets to feldspathic porcelain treated by Nd: YAG laser and hydrofluoric acid. Lasers Med Sci 2015; 30:837-841.
[Crossref] [Google Scholar] [PubMed]
- Kara HB, Ozturk AN, Aykent F, et al. The effect of different surface treatments on roughness and bond strength in low fusing ceramics. Lasers Med Sci 2011; 26:599-604.
[Crossref] [Google Scholar] [PubMed]
- Akpinar YZ, Irgin C, Yavuz T, et al. Effect of femtosecond laser treatment on the shear bond strength of a metal bracket to prepared porcelain surface. Photomed Laser Surg 2015; 33:206-212.
[Crossref] [Google Scholar] [PubMed]
- Mirhashemi A, Chiniforush N, Jadidi H, et al. Comparative study of the effect of Er: YAG and Er: Cr; YSGG lasers on porcelain: Etching for the bonding of orthodontic brackets. Lasers Med Sci 2018; 33:1997-2005.
[Crossref] [Google Scholar] [PubMed]
- Ghavam M, Soleimanpour M, Hashemikamangar SS, et al. Micro shear bond strength of self-adhesive composite to ceramic after mechanical, chemical and laser surface treatments. Laser Ther 2017; 26:297-304.
[Crossref] [Google Scholar] [PubMed]
- Ren D, Luo X. Effect of hydrofluoric acid etching time and resin bonding on the flexural strength of lithium disilicate glass ceramic. Zhonghua Kou Qiang Yi Xue Za Zhi 2013; 48:462-466.
[Google Scholar] [PubMed]
- Zogheib LV, Bona AD, Kimpara ET, et al. Effect of hydrofluoric acid etching duration on the roughness and flexural strength of a lithium disilicate based glass ceramic. Braz Dent J 2011; 22:45-50.
[Crossref] [Google Scholar] [PubMed]
- Ozdemir H, Aladag LI. Effect of different surface treatments on bond strength of different resin cements to lithium disilicate glass ceramic: An in vitro study. Biotechnol Biotechnol Equip 2017; 31:815-820.
- Shiu P, de Souza-Zaroni WC, Eduardo CDP, et al. Effect of feldspathic ceramic surface treatments on bond strength to resin cement. Photomed Laser Surg 2007; 25:291-296.
[Crossref] [Google Scholar] [PubMed]
- Cho S, Rajitrangson P, Matis B, et al. Effect of Er, Cr: YSGG laser, air abrasion and silane application on repaired shear bond strength of composites. Oper Dent 2013; 38:E58-E66.
[Crossref] [Google Scholar] [PubMed]
- Ekworapoj P, Sidhu SK, McCabe JF. Effect of different power parameters of Er, Cr: YSGG laser on human dentine. Lasers Med Sci 2007; 22:175-182.
[Crossref] [Google Scholar] [PubMed]
- Zanjani AV, Ahmadi H, Nateghifard A, et al. Effect of different laser surface treatment on micro shear bond strength between zirconia ceramic and resin cement. J Investig Clin Dent 2015; 6:294-300.
[Crossref] [Google Scholar] [PubMed]
- Moharamzadeh K, Hooshmand T, Keshvad A, et al. Fracture toughness of a ceramic resin interface. Dent Mater 2008; 24:172-177.
[Crossref] [Google Scholar] [PubMed]
- Braga RR, Meira JB, Boaro LC, et al. Adhesion to tooth structure: A critical review of “macro” test methods. Dent Mater 2010; 26:e38-e49.
[Crossref] [Google Scholar] [PubMed]
Author Info
Ola Mohammed Abdul Kadhim* and Mohammed Rashid Aljuboury
Department of Restorative and Esthetic Dentistry, College of Dentistry, University of Baghdad, Baghdad, IraqCitation: Ola Mohammed Abdul Kadhim, Mohammed Rashid Aljuboury, Shear Bond Strengths of Composite Resin Used to Repair Lithium Disilicate and Feldspathic CAD/CAM Ceramics Treated by Different Lasers (A Comparative In Vitro Study), J Res Med Dent Sci, 2023, 11 (06): 015-024.
Received: 12-Jun-2022, Manuscript No. JRMDS-22-66431; , Pre QC No. JRMDS-22-66431 (PQ); Editor assigned: 15-Jun-2022, Pre QC No. JRMDS-22-66431 (PQ); Reviewed: 30-Jun-2022, QC No. JRMDS-22-66431; Revised: 31-May-2023, Manuscript No. JRMDS-22-66431 (R); Published: 09-Jun-2023