Research Article - (2022) Volume 10, Issue 9
SOFA Score on Presentation to Emergency Department in Predicting in-Hospital Mortality of Patients with Sepsis
Gudithi Bhuvaneswari1, Sethu Babu1*, Susan Tharian1 and Mathew Pulicken2
*Correspondence: Dr. Sethu Babu, Department of Critical Care Medicine, Pushpagiri Institute of Medical Sciences, Thiruvalla, Kerala, India, Email:
Abstract
Background: Sequential Organ Failure Assessment score (SOFA) is an objective tool to describe individual and aggregate organ dysfunction in critically ill patients. The aim of the study was to determine the diagnostic utility of Admission time SOFA score calculated at the Emergency Department (ED) in predicting in-hospital mortality of patients with suspected sepsis.
Materials and methods: Patients aged 18 years or above with clinical features of infection and satisfying two or more q SOFA criteria were enrolled into the study. On arrival to the emergency department, patients were assessed and resuscitated as per the institutional sepsis protocol. Clinical and laboratory parameters required to calculate the SOFA score were collected and documented at the ED. Patients are then followed up to the clinical end point as defined as Survival to hospital discharge or Death. Receiver Operating Curve (ROC) analysis was done to determine the discriminative ability of admission time SOFA score to predict in-hospital mortality.
Results: A total of 182 patients were included in the study. Of this 111 patients (61%) died and 71 patients (39%) survived to hospital discharge. The mean SOFA score of patients who died during the hospital stay was 12.9 (SD=2.8) and that of patients who survived to hospital discharge was 9.2 (SD=3%) and the difference was statistically significant with a p-value of <0.01. ROC analysis revealed that at the optimal cut off value of 10.5, SOFA score on admission carried a sensitivity of 85.6%, Specificity of 62% and accuracy of 76.4% in predicting in-hospital mortality.
Conclusions: SOFA score calculated on admission at the Emergency department is a useful tool to predict in-hospital mortality of patients with sepsis.
Keywords
SOFA score, Sepsis, In-hospital mortality
Introduction
Sepsis is an important cause of emergency department visits and carries high hospital mortality. Sepsis syndrome is characterised by organ dysfunction due to dysregulated host immune response to infection [1]. The degree and extent of organ dysfunction can be objectively assessed using Sequential Organ Failure Assessment (SOFA) score [2] which is widely used in Intensive Care Units (ICU). SOFA is simple to calculate based on bedside clinical assessment and laboratory tests which are easily available in the Emergency Department (ED) also. So far the evidence regarding the clinical utility of SOFA score in the Emergency department is scarce. In this context, the main objective of the study was to evaluate the diagnostic utility of SOFA score as calculated on admission at the ED in predicting in-hospital mortality of patients with presumed sepsis.
Materials and Methods
Study design: The study was conducted as a prospective observational study at the Department of Emergency Medicine, Pushpagiri Institute of Medical Sciences, Thiruvalla, and Kerala, India. The study protocol was approved by the Institutional Ethics committee (PIMSRC/ E1/388A/13/2018). The study was conducted for a period of 18 months from May 2018. Patients aged 18 years or more with presumed infection on clinical examination and also satisfying 2 or more q SOFA criteria (Table 1) were enrolled into the study. Patients who had not consented or those with absent clinical evidence of focus of infection or who did not satisfy q SOFA criteria were excluded from the study. On arrival of the patient to the ED, the emergency physician on duty performed patient assessment and resuscitation as per the institutional sepsis protocol. Arterial blood gas was drawn for analysis. Venous blood was drawn for complete hemogram, coagulation studies, renal function tests and liver function tests. SOFA score is calculated based on the parameters as shown in Table 2. Patients were then disposed to ICU or Ward based on their clinical status. They were followed up to the study end point as defined as Survival to hospital discharge or Death.
| q SOFA (Quick SOFA) Criteria |
|---|
| Respiratory rate>or=22/min |
| Altered mental status |
| Systolic blood pressure>or=100 mmHg |
Table 1: q SOFA Criteria.
| Organ system | SOFA score | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Respiratory, PO2/FiO2, mmHg (kPa) | ≥400 | <400 | <300 | <200 with respiratory support | <100 with respiratory support |
| Coagulation, Platelets, ×103/mm3 |
≥150 | <150 | <100 | <50 | <20 |
| Liver, Bilirubin, mg/dL |
<1.2 | 1.2–1.9 | 2.0–5.9 | 6.0–11.9 | >12.0 |
| Cardiovascular Hypotension |
MAP ≥70 mm Hg | MAP <70 mmHg | Dopamine <5 or Dobutamine (any dose) | Dopamine 5.1–15 or Epinephrine ≤0.1 or Norepinephrine ≤0.1 | Dopamine >15 or Epinephrine >0.1 or Norepinephrine >0.1 |
| Central nervous system, Glasgow Coma Scale |
15 | 13–14 | 10–12 | 6–9 | <6 |
| Renal, Creatinine, mg/dL. | <1.2 | 1.2–1.9 | 2.0–3.4 | 3.5–4.9 | >5.0 |
| Urine output, mL/day | <500 | <200 | |||
Table 2: Sequential Organ Failure Assessment (SOFA) score.
Statistical analysis: Categorical and quantitative variables were expressed as frequency (Percentage) and mean with SD respectively. Independent t test was used to compare quantitative parameters between categories. Receiver Operating Characteristic (ROC) curve technique was used to find the diagnostic accuracy of SOFA scores in predicting mortality. Standard diagnostic characteristics like Sensitivity, Specificity, Positive predictive value, negative predictive value and accuracy were calculated at the optimal power of the SOFA score to predict mortality. For all statistical interpretations, p<0.05 was considered as threshold for statistical significance. Statistical analysis was done by using SPSS version 20.0.
Results
Baseline demographics and co-morbidities
The study sample included 182 patients who met the inclusion criteria. The mean age of the study sample was 60.9 years with SD of 16.8 years. Minimum age was 18 years and the maximum age was 94 years. 130 patients (71.4%) were males. The baseline demographics and the distribution of co-morbidities of the study population are given in Table 3.
| Characteristics | Distribution |
|---|---|
| Age | |
| Mean Age (Mean, SD) | 60.9 (SD=16.8) Years |
| Lowest age (Years) | 18 Years |
| Highest age (Years) | 94 Years |
| Gender | |
| Male (N, %) | 130 (71.4%) |
| Female (N, %) | 52 (28.6%) |
| Co-morbidities | |
| Hypertension | 73 (40.1%) |
| T2 Diabetes Mellitus | 108 (59.3%) |
| Chronic Kidney Disease | 22 (12.1%) |
| Chronic Liver Disease | 26 (12.6%) |
| qSOFA score | |
| 3 | 54 (29.7%) |
| 2 | 128 (70.3%) |
Table 3: Baseline demographics and co-morbidities.
Distribution of the study population according to the clinical outcome
In the total study sample of 182 patients, 111 patients died and 71 patients survived constituting 61% and 39% respectively.
Comparison of SOFA score based on outcome
The mean SOFA score among the patients who died during the hospital stay was 12.9 (SD=2.8). The mean SOFA score among the survived patients was 9.2 (SD=3%). The difference was statistically significant with a p-value of <0.01. This is given in Table 4.
| Mean | SD | N | t | p | |
|---|---|---|---|---|---|
| Death | 12.9 | 2.8 | 111 | 8.29 | p<0.01 |
| Survived | 9.2 | 3.1 | 71 |
Table 4: Comparison of SOFA score based on final outcome.
Diagnostic accuracy of SOFA score on admission in predicting in-hospital mortality
The ROC curve analysis is shown in Figure 1. The area under the curve was 0.811 (0.748 to 0.874) suggesting good diagnostic accuracy of admission time SOFA score in predicting mortality. At the optimal cut off value of 10.5, SOFA score carried a sensitivity of 85.6%, specificity of 62% and diagnostic accuracy of 76.4% in predicting in-hospital mortality. This is given in Table 5.
| Sensitivity | 85.6 |
| Specificity | 62.0 |
| False Negative | 14.4 |
| False positive | 38.0 |
| Positive Predictive value | 77.9 |
| Negative Predictive value | 73.3 |
| Positive Likelihood ratio | 2.3 |
| Negative Likelihood ratio | 0.2 |
| Accuracy | 76.4 |
Table 5: Standard test characteristics of SOFA score on admission in predicting hospital mortality.
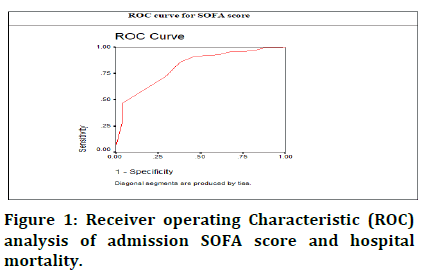
Figure 1: Receiver operating Characteristic (ROC) analysis of admission SOFA score and hospital mortality.
Discussion
SOFA score was created with the stated objective to describe the degree of organ dysfunction in patients with sepsis [2]. It has been validated mainly in Intensive Care Units (ICU) and found to be of value in describing the degree and trend of organ dysfunction in critically ill patients of any cause over a period of time [3]. Previous studies have shown that maximum SOFA score as well as the delta SOFA score are positively correlated with the ICU mortality [4-7]. But the relevance of SOFA score outside ICU is not studied well. SOFA score possesses many desirable qualities which makes it easy to calculate at bedside by the Emergency Physician in the Emergency Department also. Previous study done by Alan E Jones, et al. in 2009 had shown that SOFA score calculated in the emergency department at the time of presentation is valuable in prognostication of patients with sepsis with regard to hospital mortality [8]. Our study is aimed to gather further evidence in this regard by evaluating the clinical utility of SOFA score at the time of presentation to the Emergency department in predicting in-hospital mortality of patients with suspected sepsis.
In this study, only patients with suspected sepsis as screened by clinical examination and positive q SOFA were enrolled. The hospital mortality was found to be 61%. The mean SOFA score (as calculated at the ED) of patients who died was significantly higher when compared to that of patients who survived to hospital discharge. This finding supports the results of Alan E Jones, et al. where they also found a similar observation [8].
The Receiver Operating Characteristic analysis (ROC) has shown that the Area under Curve (AUC) was 0.811 suggesting that SOFA score at admission as calculated in the emergency department carries good diagnostic accuracy for predicting in-hospital mortality. At the optimal cut off value of 10.5, SOFA score at presentation possess good sensitivity (85.6%) and specificity (62%) to identify patients at risk of death. This finding also is in congruence with the results of the previous study by Alan E Jones, et al. [8].
We can infer from this study that SOFA score at the time of presentation as calculated in the ED is of value in prognostication of the patients with sepsis. This will help in better decision making by the emergency physician in identifying patients with sepsis at high risk of multiorgan dysfunction and also in making proper disposition plans.
Strengths and limitations: The main strength of this study is that it adds to the evidence regarding the clinical utility of SOFA score (outside the ICU) in the Emergency Department where the existing evidence is not robust. The main limitation is that it is a single centre study. Also we had calculated and studied only a single SOFA assessment in the ED and the change in SOFA score over a period of time (delta SOFA) was not calculated.
Conclusion
SOFA score calculated on admission at the Emergency Department is a useful tool to predict in-hospital mortality of patients with sepsis.
References
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med 2017; 43:304-377.
- Lambden S, Laterre PF, Levy MM, et al. The SOFA score development, utility and challenges of accurate assessment in clinical trials. Crit Care 2019; 23:1-9.
- Vincent JL, De Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit care med 1998; 26:1793-800.
- Moreno R, Vincent JL, Matos R, et al. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multi-centre study. Intensive care med 1999; 25:686-696.
- Karakike E, Kyriazopoulou E, Tsangaris I, et al. The early change of SOFA score as a prognostic marker of 28-day sepsis mortality: analysis through a derivation and a validation cohort. Crit care 2019; 23:1-8.
- Minne L, Abu-Hanna A, de Jonge E. Evaluation of SOFA-based models for predicting mortality in the ICU: A systematic review. Crit Care 2008; 12:1-3.
- Chopra S, Pednekar S, Karnik ND, et al. A Study of the Outcome of Critically Ill Elderly Patients in a Tertiary Care Hospital Using SOFA Score. Indian j Crit Care Med 2021; 25:655.
- Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypo perfusion at the time of emergency department presentation. Crit care med 2009; 37:1649.
Author Info
Gudithi Bhuvaneswari1, Sethu Babu1*, Susan Tharian1 and Mathew Pulicken2
1Department of Emergency Medicine, Pushpagiri Institute of Medical Sciences, Thiruvalla, Kerala, India2Department of Critical Care Medicine, Pushpagiri Institute of Medical Sciences, Thiruvalla, Kerala, India
Citation: Gudithi Bhuvaneswari, Sethu Babu, Susan Tharian, Mathew Pulicken, SOFA Score on Presentation to Emergency Department in Predicting in-Hospital Mortality of Patients with Sepsis, J Res Med Dent Sci, 2022, 10 (9): 235-239.
Received: 01-Jul-2022, Manuscript No. JRMDS-22-61501; , Pre QC No. JRMDS-22-61501(PQ); Editor assigned: 04-Jul-2022, Pre QC No. JRMDS-22-61501(PQ); Reviewed: 18-Jul-2022, QC No. JRMDS-22-61501; Revised: 01-Sep-2022, Manuscript No. JRMDS-22-61501(R); Published: 08-Sep-2022
