Case Report - (2019) Volume 7, Issue 5
Spontaneous Isolated Dissection of the Celiac Artery and Superior Mesenteric Artery: A Case Report
Atul Dwivedi, Xiao Ming Qiu*, Shweta Shukla Dwivedi, Muhammad Raheel Tariq, Su Zhenhong and Yu Xin
*Correspondence: Xiao Ming Qiu, Department of radiology, Huangshi Central hospital, Affiliated hospital of Hubei polytechnic University, Edong health care group, China, Email:
Abstract
Simultaneous occurrence of spontaneous isolated dissection of the celiac artery (CA) and superior mesenteric artery (SMA) is rare. Here, we report the clinical course of a 50-year-old man who presented with severe, acute upper abdominal pain. Computed tomographic angiography (CTA) revealed segmental small intestinal ischemia and dissection of the CA and SMA. The patient was discharged after conservative treatment, but mild abdominal pain recurred subsequently. Several repeated CTAs showed small bowel wall thickening. These findings show that symptoms of SMA dissection along with intestinal ischemia can be alleviated with conservative treatment, but abdominal pain and chronic bowel wall thickening can persist for a long time.
Keywords
Celiac artery, Superior mesenteric artery, Spontaneous dissection, Isolated dissection
Introduction
A true isolated SMA dissection is a rare condition. This was first described in 1947 by Bauersfeld Arterial dissection is defined as the cleavage of the arterial wall by an intramural hematoma. Dissection of superior mesenteric is often seen with a continuation of of aortic dissection [1]. The superior mesenteric artery is the second of the three major anterior branches of the abdominal aorta and takes origin from anterior surface of the abdominal aorta, just inferior to origin of the celiac trunk at the level of L1 vertebra. It supplies blood to the midgut organs, intestine, abdominal viscera (including pancreas) etc. [2]. Dyspepsia with mild, stabbing epigastric pain without trauma history is a very common condition that handled in emergency department. Vascular emergencies like aortic aneurysm and dissection are always defined in the differential diagnosis with these mentioned symptoms [3]. Isolated spontaneous celiac artery dissection is uncommon and this rare diagnosis is made in patient with acute abdominal pain. After an extensive search on Medline database, Mauricio et al. found 33 reported cases of coeliac artery dissection (CAD) [4]. Among spontaneous dissection of splanchnic artery including the superior mesenteric artery (SMA) and inferior mesenteric artery (IMA) and coeliac artery, the isolated coeliac artery dissection is least commonly reported [5]. Depending on the case, physicians may apply several management methods like endovascular repair, interventional radiological approach. But conservative treatment options with anticoagulant, anti-platelet along with antihypertensive can also use [6]. Isolated dissection of a splanchnic artery is defined as dissection of a single splanchnic artery without any aortic dissection; this condition is rare. Simultaneous isolated dissection of the celiac artery (CA) and superior mesenteric artery (SMA) is extremely rare. On reviewing the literature, we found only 2 reported cases of this condition [7,8].
Case Report
A 50-year-old male patient presented with an acute, severe, persistent, tearing upper abdominal pain without any apparent cause. He was admitted 2 hours after the pain radiated to his back. The patient did not have any nausea, vomiting, injury, and surgical history. He had a 20- year history of smoking and a 10-year history of hypertension, denied alcohol or illicit drug abuse. Physical examination revealed soft abdomen, subxiphoid tenderness, no rebound tenderness, and a blood pressure of 140/110 mmHg. Other vital signs were normal. Results of electrocardiography and blood workup were normal, and the patient showed normal laboratory test like, erythrocyte sedimentation rate, coagulation time, blood and urine test amylase, lipase, lactic acid, liver function test and renal function. Computed tomographic angiography (CTA) revealed isolated CA dissection along with isolated SMA dissection. The patient was administered conservative treatment, and his symptoms were alleviated. The patient was discharged from the hospital and prescribed to continue Aspirin therapy. Subsequently, mild upper abdominal pain recurred and was relieved after bed rest. The following CTA images were obtained on admission and 2 weeks, 6 months, and 10 months after admission (Figures 1-5).
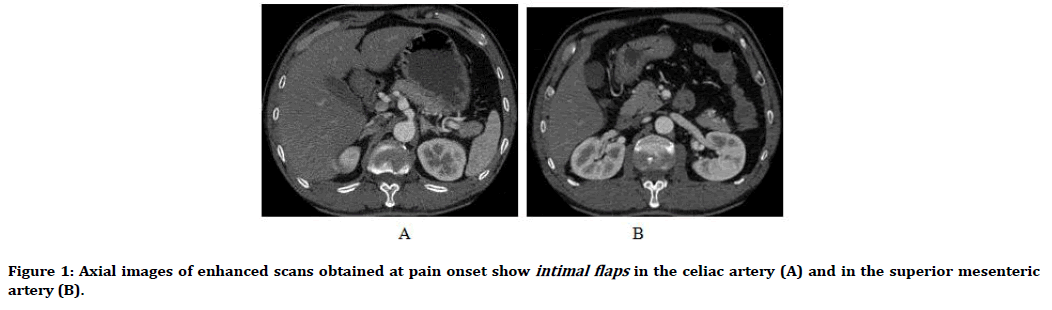
Figure 1. Axial images of enhanced scans obtained at pain onset show intimal flaps in the celiac artery (A) and in the superior mesenteric artery (B).
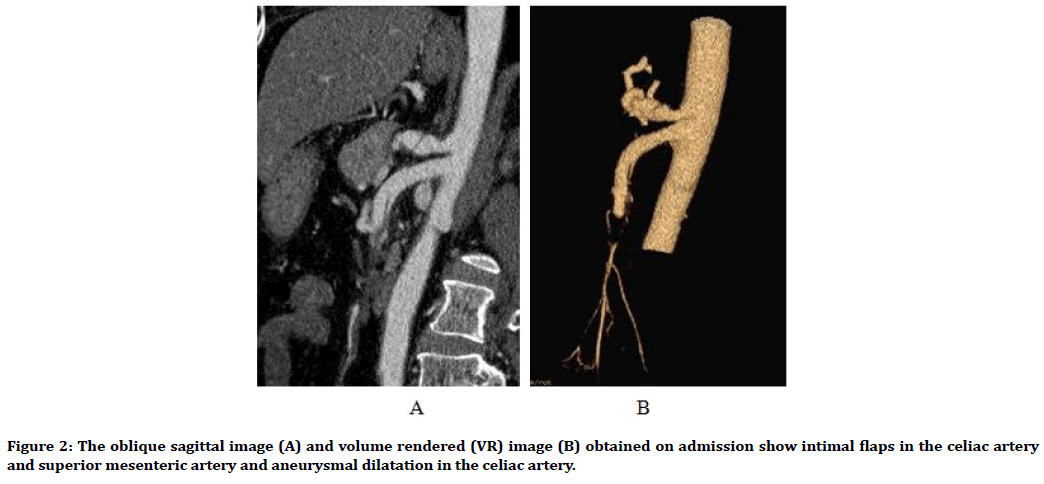
Figure 2. The oblique sagittal image (A) and volume rendered (VR) image (B) obtained on admission show intimal flaps in the celiac artery and superior mesenteric artery and aneurysmal dilatation in the celiac artery.
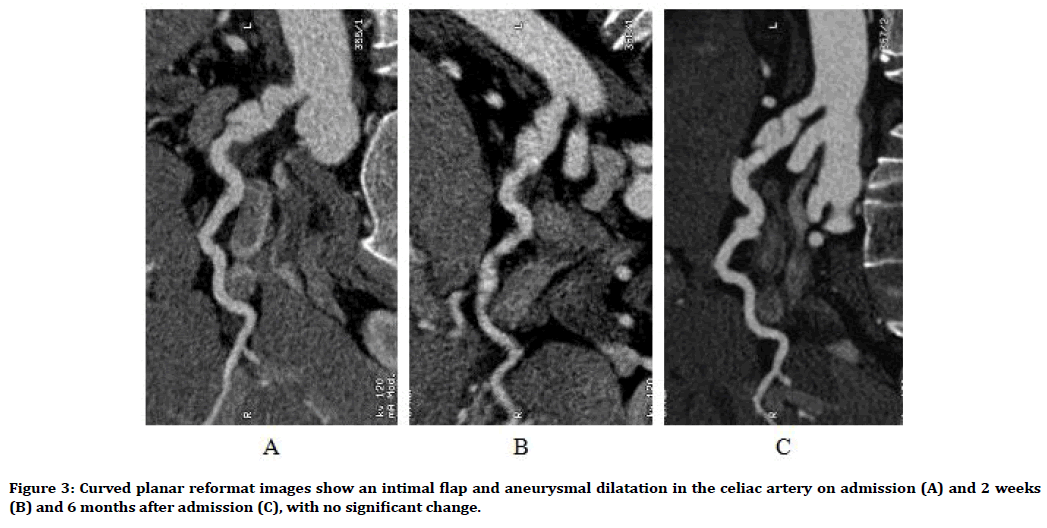
Figure 3. Curved planar reformat images show an intimal flap and aneurysmal dilatation in the celiac artery on admission (A) and 2 weeks (B) and 6 months after admission (C), with no significant change.
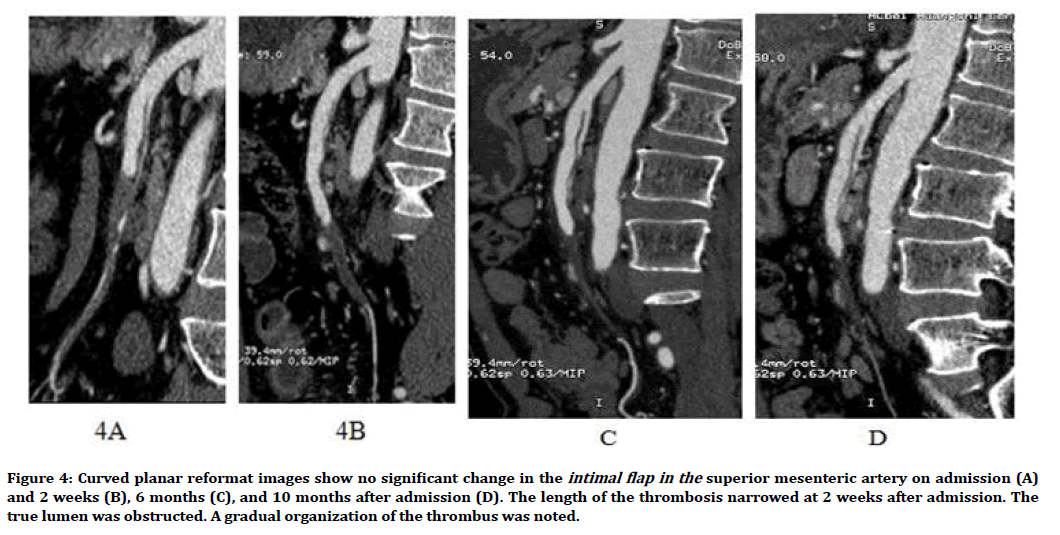
Figure 4. Curved planar reformat images show no significant change in the intimal flap in the superior mesenteric artery on admission (A) and 2 weeks (B), 6 months (C), and 10 months after admission (D). The length of the thrombosis narrowed at 2 weeks after admission. The true lumen was obstructed. A gradual organization of the thrombus was noted.
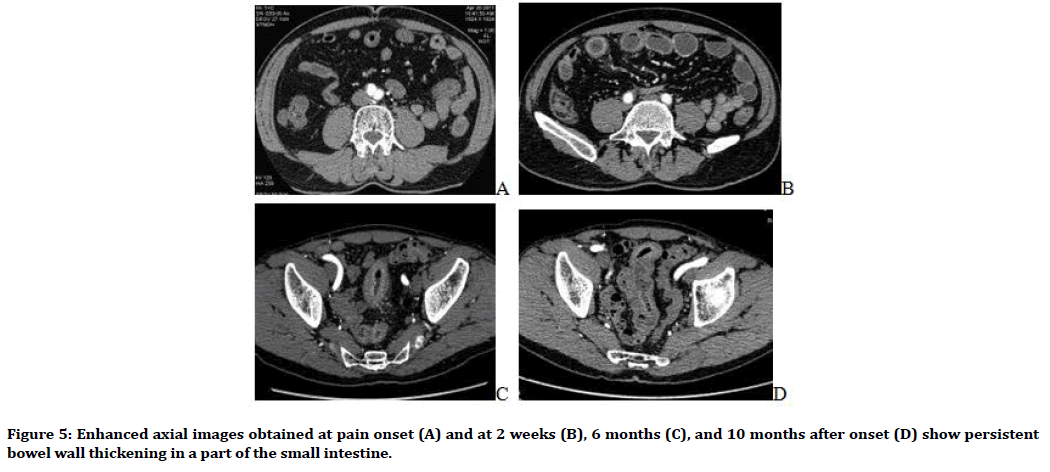
Figure 5. Enhanced axial images obtained at pain onset (A) and at 2 weeks (B), 6 months (C), and 10 months after onset (D) show persistent bowel wall thickening in a part of the small intestine.
Discussion
Isolated splanchnic dissection is rare. The increasing use of CT and other diagnostic imaging techniques has significantly increased the number of reported cases of this condition [9-12]. Of the peripheral artery dissections, dissection of the SMA is the second most common after internal carotid artery dissection. Almost two-thirds of all splanchnic dissections involve the SMA, and less than one-third involve the CA. The ratio of the incidence of splanchnic dissections in men and in women is 5:1. The average age of splanchnic dissection patients at presentation is around 55 years [7-9,13-15].
The etiologies of dissection are unclear. Risk factors include hypertension, connective tissue disorders, vasculitis, atherosclerotic disease, cystic medial necrosis, fibromuscular dysplasia, trauma, and pregnancy [7,12,13,16].
Clinical presentation varies, but the patient usually present with upper abdominal pain and complications like nausea, vomiting, and abdominal distention. Patients with SMA dissection are more often symptomatic than those with CA dissection [13,17]. Some patients may be asymptomatic and be detected incidentally [13,15].
The typical CTA image of splanchnic dissection shows intraluminal filling defect and low-density intimal flap in the true lumen. Aneurysmal dilatation may be observed. Attenuation of the surrounding fat is observed in unenhanced CT and may be associated with acute dissection [13]. The underlying mechanism may be peripheral inflammation caused by dissection. Thrombus in the celiac trunk or SMA is indicative of SMA dissection [13,16,18].
Choosing an appropriate management strategy for splanchnic dissections is still controversial [7,8,10,11,15]. The asymptomatic patients detected incidentally can be provisionally kept under observation. The majority of symptomatic patients without obvious intestinal necrosis and arterial rupture can be successfully managed with conservative treatment. Percutaneous intervention is reserved for patients who fail to respond to conservative treatment. Surgery is performed for patients with intestinal necrosis, threatened rupture of artery, and progressive development of aneurysmal dilatation. In our study, the patient’s symptoms were alleviated with conservative treatment. However, mild abdominal pain recurred after discharge. CTA images revealed long-term persistence of small bowel wall thickening. This shows that segmental intestinal wall thickening can persist for a long time in patients with SMA dissection and intestinal ischemia. The underlying mechanism needs to be further investigated to determine whether chronic intestinal inflammation causes intestinal wall thickening in addition to chronic intestinal ischemia.
Conclusion
Spontaneous isolated dissection of the CA and SMA is extremely rare. SMA dissection with intestinal ischemia, but without obvious intestinal necrosis, can be treated with conservative treatment. However, abdominal pain and the CTA finding of chronic intestinal wall thickening may persist.
Large series of cases and prospective studies are warranted For a definitive way of treatment.
References
- Bauersfeld SR. Dissecting aneurysm of the aorta: A presentation of 15 cases and a review of the recent literature. Ann Intern Med 1947; 26:873-889.
- Gray H, Lewis WH. Anatomy of human body. 20th Edn. Philadelphia. 1918.
- Tintinalli J, Stapczynski J, Stapczynski O, et al. Tintinalli's Emergency Medicine: A comprehensive study guide. 7th Edn. 2011.
- Mauricio OD, Bahaeddin S, Kathryn G D, et al. Spontaneous celiac artery dissection: Case report and literature review. Texas Heart Ins J 2012; 39:703-706.
- Nordanstig J, Gerdes H, Kocys E. Spontaneous isolated dissection of the celiac trunk with rupture of the proximal splenic artery: A case report. Eur J Vasc Endovasc Surg 2009; 37:194-197.
- Fenoglio L, Allione A, Scalabrino E, et al. Spontaneous dissection of the celiac artery: A pitfall in the diagnosis of acute abdominal pain. Presentation of two cases. Dig Dis Sci 2004; 49:1223-1227.
- Kang TL, Teich DL, Mc Gillicuddy DC. Isolated, spontaneous superior mesenteric and celiac artery dissection: Case report and review of literature. J Emerg Med 2008; 40:21-25.
- Mousa AY, Coyle BW, Affuso J, et al. Nonoperative management of isolated celiac and mesenteric artery dissection: Case report and review of literature. Vascular 2009; 17:359-364.
- Carter R, O'Keeffe S, Minion DJ, et al. Spontaneous superior mesenteric artery dissection: Report of 2 patients and review of management recommendation. Vasc Endovascular Surg 2011; 45:295-298.
- Wu XM, Wang TD, Chen MF. Percutaneous endovascular treatment for isolated superior mesenteric artery dissection: Report of two case and literature review. Catheter Cardiovasc Interv 2009; 73:145-151.
- Choa BS, Lee MS, Lee MK, et al. Treatment guideline for isolated dissection of the superior mesenteric artery based on follow- up CT findings. Eur J Vasc Endovasc Surg 2011; 41:780-785.
- Okada M, Ishiguchi T, Iton H. Management of spontaneous dissection of the superior mesenteric artery: Case report and literature review. Intern Med 2004; 43:451-452.
- D'Ambrosio N, Friedman B, Siegel D, et al. Spontaneous isolated dissection of the celiac artery: CT findings in adults. Am J Roentgenology 2007; 188:506-511.
- Leung DA, Schneider E, Kubik-Huch R, et al. Acute mesenteric ischemia caused by spontaneous isolated dissection of the superior mesenteric artery: Treatment by percutaneous stent placement. Eur Radiol 2000; 10:1916-1919.
- Takayama T, Miyata T, Shirakawa M, et al. Isolated spontaneous dissection of the splanchnic arteries. J Vasc Surg 2008; 48:329-333.
- Yun WS, Kim YW, Park KB, et al. Clinical and angiographic follow -up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg 2009; 37:572-577.
- Park YJ, Park CW, Park KB, et al. Interference from clinical and fluid dynamic studies about underlying cause of spontaneous isolated superior mesenteric artery. J Vasc Surg 2011; 53:80-86.
- Furukawa H, Moriyama N. Spontaneous dissection of the mesenteric artery diagnosed on multi detector helical CT. J Computer Assist Tomogr 2002; 26:143-144.
Author Info
Atul Dwivedi, Xiao Ming Qiu*, Shweta Shukla Dwivedi, Muhammad Raheel Tariq, Su Zhenhong and Yu Xin
Department of radiology, Huangshi Central hospital, Affiliated hospital of Hubei polytechnic University, Edong health care group, Huangshi , Hubei, ChinaCitation: Atul Dwivedi, Xiao Ming Qiu, Shweta Shukla Dwivedi, Muhammad Raheel Tariq, Su Zhenhong, Yu XinSpontaneous Isolated Dissection of the Celiac Artery and Superior Mesenteric Artery: A Case Report, J Res Med Dent Sci, 2019, 7(5): 94-97
Received: 11-Jul-2019 Accepted: 08-Oct-2019
