Research - (2020) Advances in Dental Surgery
Study of Below the Knee BTK Intervention at Medical City Hospital 2018 to 2020
Ahmed Abdulsalam Khaleel, Abdulameer Mohsin Hussein* and Sabah N Jaber
*Correspondence: Abdulameer Mohsin Hussein, Department of Surgery, College of Medicine, University of Baghdad, Iraq, Email:
Abstract
Objective: To analyze the risk factors and to evaluate the technical outcome of patients who underwent endovascular treatment for below the knee arteries.
Methods: Retrospective descriptive study with analytic component. We had researched from 2018 to 2020 in the Endovascular Surgical Department at Medical City Hospital (Baghdad/ Iraq). It included 70 patients having BTK arterial disease and treated by endovascular intervention during 2018-2020. The cases were reviewed by using TASC classification. Clinical examination and ABI calculations were performed for the patients. Then under the local anesthesia either antegrade or retrograde approach by means of sheath, wire, catheter and self- expandable balloon were used.
Results: In this study, the results of intervention (Category B) were good in 64% of patients. Prevalence of poor results of intervention were mainly noticed in patients with more than two risk factors and in patients with severe disease. Regarding complication of intervention, 22% of patients were developed complication and the most common complication was amputation (8%).
Conclusions: The endovascular treatment of atrial disease of the lower limbs is a safe, effective and less invasive method with short hospital stays and fast recovery of the patients. Short-term results show a good success rate.
Keywords
Arterial occlusion, below the knee, endovascular therapy, Iraq
Introduction
Chronic limb ischemia (CLI) is the most important clinical indication for a below the knee intervention [1]. It is defined as inadequate blood supply and considered a daily problem in vascular department [2]. Over 202 million persons worldwide are affected by peripheral arterial disease (PAD) [3]. More than 20% of people over the age of 65 have PAD, in which the prevalence of the symptomatic manifestations in males is over 8%. A PAD is the end outcome of a process that gradually narrows the lumen of the arteries through which the blood flows. In general, this vasoconstriction is a sign of atherosclerotic changes that occurs in the walls of the vessels [4]. The prevalence of CLI depends on age as well, with about 20% of the adults aged 70 years and older are diagnosed with critical limb ischemia. The effect of this disease on health care will be increased as the population ages [5]. Variations in the clinical presentation of CLI occur from free symptoms to intermittent claudication, rest pain, ischemic ulcers, and gangrenes. The typical risk factors involve old age, smoking, diabetes mellitus, hypercholesterolemia, and hypertension [6]. The diagnosis of CLI is clinical; and the Ankle-Brachial Index (ABI) is a simple test that is used to confirm the diagnosis and quantify the severity of chronic limb ischemia. The ABI calculation is achieved by dividing the ankle pressure by the highest brachial pressure. An ABI of 0.7 to 0.9 is considered a mild disease, from 0.5 to 0.69 is a moderate disease, and <0.5 is a severe disease [7]. The main goal of the therapy is to preserve limb function. Revascularization is a fundamental strategy to limb preservation, but in some patients, this does not improve limb function and mobility. When revascularization is considered, arterial imaging identifies the targets and mode of revascularization [8]. In many centers, endovascular intervention is the favored approach to CLI, because of lower morbidity and mortality as compared with the open surgery. The optimal treatment strategy (endovascular versus open surgery) will depend on anatomical factors, comorbidities, patient preference and operator experience and skill [9]. The primary indications for arterial disease intervention are limb salvage to avoid amputations [10]. The aim of this study is to analyze the risk factors and to evaluate the technical outcome of patients who underwent endovascular treatment for belowthe- knee arteries.
Patients and Methods
Study design, setting: This was a retrospective review that was conducted in the Endovascular Surgical Department at Medical City Hospital during the period of one year from 1st of Jan. 2018 till end of Dec. 2020.
Study population and sample size: The study included 70 patients had BTK arterial disease treatment by endovascular interventions during 2018-2020. The cases were reviewed by using TASC classification in Figure 1 [11].
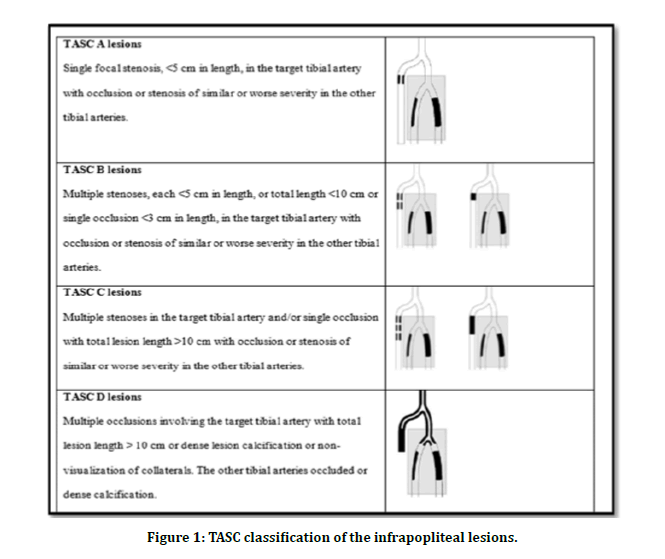
Figure 1: TASC classification of the infrapopliteal lesions.
Procedure
As Patients were lying on bed in supine position, we examined the right and left femoral pulse by palpation and Doppler ultrasound. Clinical examination and ABI calculations were performed for the patients. Then under the local anesthesia either antegrade or retrograde approach by means of sheath, wire, catheter, and self- expandable balloon were used. Seventy patients of both genders with peripheral vascular diseases were involved in this study, fifty of them underwent the endovascular intervention. The presence of blood flow and its continuity, and the disappearance of the lesion which were revealed by angiography were considered as good results.
Statistical analysis
Data analysis had been accomplished by the SPSS version 25. The data presented as means, standard deviations and ranges. Categorical data presented by frequencies and percentages. Chi square test was used to assess the association between intervention results and certain characteristics, while fisher exact test was used instead when the expected frequency was less than 5. A level of P–value less than 0.05 was considered significant.
Results
70 patients were involved in this research, aged from 29 to 70 years with a mean of 52.17 ± 10.4 years. About two thirds of them were males (65.7%); 38.6% had two risk factors; 58.6% were graded with moderate severity of disease; 41.4% were in TASC B; and 28.6% of the cases (category A) were diagnosed by angiography and treated by medication such as antilipid, antiplatelet, analgesia and focus on exercise; while the majority (71.4%) were treated by selfexpandable balloon angiography intervention (category B) via antegrade or retrograde approach as shown in Table 1. We noticed that the results of intervention (Category B) were good in 64% of patients as shown in Figure 2.
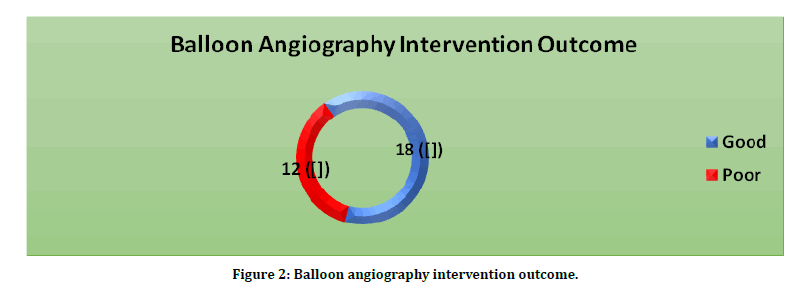
Figure 2: Balloon angiography intervention outcome.
| Variable | No. (n= 70) | Percentage (%) |
|---|---|---|
| Age (Years) | ||
| <40 | 9 | 12.9 |
| 40-59 | 44 | 62.9 |
| ≥ 60 | 17 | 24.2 |
| Gender | ||
| Male | 46 | 65.7 |
| Female | 24 | 34.3 |
| Risk Factor | ||
| One | 14 | 20 |
| Two | 27 | 38.6 |
| More than two | 29 | 41.4 |
| Severity of disease (ABI) | ||
| Mild | 15 | 21.4 |
| Moderate | 41 | 58.6 |
| Severe | 14 | 20 |
| TASC | ||
| A | 20 | 28.6 |
| B | 29 | 41.4 |
| C | 17 | 24.3 |
| D | 4 | 5.7 |
| Type of treatment | ||
| Diagnostic (Category A) | 20 | 28.6 |
| Intervention (Category B) | 50 | 71.4 |
Table 1: Distribution of study patients by general information.
In this study, prevalence of poor results of intervention were mainly noticed in patients with more than two risk factors (54.5%, P=0.048) and in patients with severe disease (70%, P=0.025) with significant associations between the severity of the disease, risk factors with the intervention results as shown in Table 2.
| Variable | Intervention Result | Total (%) | P–Value | |
|---|---|---|---|---|
| Poor (%) n=18 | Good (%) n=32 | n= 50 | ||
| Age (Years) | ||||
| < 40 | 2 (33.3) | 4 (66.7) | 6 (12.0) | 0.109 |
| 40 - 59 | 9 (29.0) | 22 (71.0) | 31 (62.0) | |
| ≥ 60 | 7 (53.8) | 6 (46.2) | 13 (26.0) | |
| Gender | ||||
| Male | 14 (43.8) | 18 (56.3) | 32 (64.0) | 0.128 |
| Female | 4 (22.2) | 14 (77.8) | 18 (36.0) | |
| Risk Factor | ||||
| One | 1 (14.3) | 6 (85.7) | 7 (14.0) | 0.048 |
| Two | 5 (23.8) | 16 (76.2) | 21 (42.0) | |
| More than two | 12 (54.5) | 10 (45.5) | 22 (44.0) | |
| Severity of disease | ||||
| Mild | 0 (0) | 3 (100.0) | 3 (6.0) | 0.025 |
| Moderate | 11 (29.7) | 26 (70.3) | 37 (74.0) | |
| Severe | 7 (70.0) | 3 (30.0) | 10 (20.0) | |
| TASC | ||||
| A | 4 (28.6) | 10 (71.4) | 14 (28.0) | 0.207 |
| B | 8 (30.8) | 18 (69.2) | 26 (52.0) | |
| C | 6 (60.0) | 4 (40.0) | 10 (20.0) | |
Table 2: Association between intervention results and certain characteristics.
Regarding complication of intervention, 22% of patients were developed complication and the most common complication was amputation (8%) as shown in Table 3.
| Complication | No. (n=50) | Percentage (%) |
|---|---|---|
| No complication | 39 | 78 |
| Amputation | 4 | 8 |
| Occlusion | 2 | 4 |
| Hematoma | 3 | 6 |
| Dissection | 2 | 4 |
Table 3: Complication of intervention.
Discussion
In the current research, a high proportion of men than women were found. Most of the cases had more than two risk factors (diabetes, hyperlipidemia, hypertension, old age and nicotine abuse. etc.).
The present study revealed that the patients with more than two risk factors show poor prognosis. This is agree with other documents [12,13] that found smoking and hypercholesterolemia were factors that accelerate the process of pathological blood vessels, increase the disease severity and had significant impact on the CLI of the lower extremities.
Also, the results illustrate that the diseased vessels (ABI <5) show poor prognosis. This can be due to the ABI has an important role in patients with PAD, not just as a diagnostic tool, but rather as a negative predictor; since it is considered a generali¬zed atherosclerotic predictor (atherosclerosis plays a critical role in blood flow obstruction), in addition the ABI detect the patients at high risk for developing PAD [14].
However, no significant association between the different age groups, gender and TASC classifications with the outcome. This is may be attributed to the fact that the PAD is a multifactorial disease, and its pathophysiology is complex [15]. Nevertheless, the efficacy of therapeutic interventions is affected by good technique and equipment, medical treatment, control of risk factors in addition to the physical exercise.
The total complication of our study was 22%; mainly hematoma and amputation that account 14%, in comparison with 22% in Le et al. [16]. However, the dissection was 4% while it was 7% in Černevičiūtė [17].
The endovascular intervention method in this study succeeded the reperfusion of lower limb and achieved good results, with success outcome of 64%, While Le et al. and Černevičiūtė et al. achieved 88.9% and 93.7% respectively [16,17]; with significant improvement of the clinical symptoms especially for 40-59 years-old patients, with moderate medical conditions and ≤ 2 risk factors. Once again, this result confirmed the effectiveness of this intervention to the patients with BTK arterial disease. In conclusion, by endovascular interventions treatment of 50 cases with chronic below-the-knee arterial occlusive diseases, we have concluded the following:
Improvement of the clinical symptoms with moderate medical conditions and ≤ 2 risk factors.
Less duration of hospital stays and fast recovery of patients.
Endovascular treatment is a less invasive method with good outcome.
Limitations
The results obtained with other publications are quite difficult to compare due to the groups of patients’ heterogeneities, different results definitions, experience of the intervention doctor, techniques performed and means used. Besides, the peripheral artery disease, its anatomical course and the spread of lesions are very individual for each patient, depending on many concomitant factors such as comorbidities, medications used, harmful habits and physical activity.
Recommendations
Because of the difficulties of PTA and its complications using a plain angioplasty balloon, a newer endovascular device, like drug eluting balloons and highly resolution Doppler ultrasound, should be applied.
References
- Sauguet A, Leger P. Tools and techniques: Below the knee interventions. EuroIntervention 2012; 7:1120-1123.
- Simon F, Oberhuber A, Floros N, et al. Pathophysiology of chronic limb ischemia. Gefasschirurgie 2018; 23:13-18.
- Fowkes FGR, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013; 382:1329-1340.
- Kröger K, Stang A, Kondratieva J, et al. Prevalence of peripheral arterial disease–results of the Heinz Nixdorf recall study. European J Epidemiol 2006; 21:279.
- Davies MG. Criticial limb ischemia: Epidemiology. Methodist Debakey Cardiovasc J 2012; 8:10-14.
- Meijer WT, Grobbee DE, Hunink MM, et al. Determinants of peripheral arterial disease in the elderly: The rotterdam study. Archives Intern Med 2000; 160:2934-2938.
- McDermott MM, Liu K, Greenland P, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA 2004; 292:453-461.
- Oresanya L, Zhao S, Gan S, et al. Functional outcomes after lower extremity revascularization in nursing home residents: A national cohort study. JAMA Intern Med 2015; 175:951-957.
- Kinlay S. Management of critical limb ischemia. Circulation: Cardiovascular Interventions 2016; 9:e001946.
- Higashimori A. Angiography and endovascular therapy for below-the-knee artery disease. Angiography Endovascular Therapy Peripheral Artery Disease 2017:101.
- Jaff Michael R, White Christopher J, Hiatt William R, et al. An Update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: A supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II). Annals Vascular Dises 2015; 8:343-357.
- Sobieszczyk P, Eisenhauer A. Management of patients after endovascular interventions for peripheral artery disease. Circulation 2013; 128:749-757.
- Jaff MR, White CJ, Hiatt WR, et al. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: A supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II). Vascular Med 2015; 20:465-478.
- Rac-Albu M, Iliuta L, Guberna SM, et al. The role of ankle-brachial index for predicting peripheral arterial disease. Maedica 2014; 9:295-302.
- Stewart KJ, Hiatt WR, Regensteiner JG, et al. Exercise training for claudication. N Engl J Med 2002; 347:1941-1951.
- Le TD. Evaluation of endovascular intervention therapy results in chronic below-the-knee (BTK) arterial occlusive disease. Angiol 2016; 4:184.
- Černevičiūtė R. Results of endovascular treatment of calf arteries. 2018.
Author Info
Ahmed Abdulsalam Khaleel, Abdulameer Mohsin Hussein* and Sabah N Jaber
Department of Surgery, College of Medicine, University of Baghdad, IraqCitation: Sarah M Khammas, Ahlam T Mohammed, Study of Below the Knee BTK Intervention at Medical City Hospital 2018 to 2020, J Res Med Dent Sci, 2020, 8 (7): 37-41.
Received: 27-Sep-2020 Accepted: 13-Oct-2020 Published: 20-Oct-2020
