Review Article - (2023) Volume 11, Issue 1
Study of COVID-19 Virus Causing Deaths in Chronic Kidney Disease Patients
B Uma Maheswara Reddy*, Swarupa Chakole and Ashok Mehendale
*Correspondence: B Uma Maheswara Reddy, Department of Community Medicine, Jawaharlal Nehru Medical University, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, India, Email:
Abstract
Coronavirus disease 2019 presents as an asymptomatic infection to severe pneumonia and respiratory failure. There is higher mortality in old age patients who are suffering from the chronic illness like hypertension, diabetes mellitus or cardiovascular diseases. When compared to the normal population, the CKD patients have been reported higher mortality due to alteration in immune system and immune suppression they are predisposed to infectious complications like COVID-19.
Chronic kidney disease patients have shown the increased higher incidence of COVID-19 and increased mortality CKD is relevant comorbidity been correlated with increased mortality when compared to the normal population. Holistic support is given to the CKD patients by the caregivers and family members whom helps in reducing the psychological impact caused due to hemodialysis. SARS-CoV-2 infection can cause mainly affects respiratory system, but it also affects other body organs where most of the complications occur due to damage to the kidney as a complication but it’s difficult to identify as its clinical manifestations are highly variable. So the patients who ever require dialysis have been considered as high risk group. In the presence of viremia, the organs like kidney, ileum and heart might be affected by SARSCoV-2. The main target of SARS-CoV-2 are ACE receptors other than respiratory cells they are also expressed on the proximal tubular epithelial cells, glomerular mesangial cells and podocytes and another target is CD147 expressed on the basolateral membrane proximal and distal tubular cells. Due to systemic inflammation and acquired immunosuppression results in alteration of immune system. There is phagocytic dysfunction of B cells and T cells and decreased neutrophil function seen in pre dialysis and dialysis patients. In this retrospective study we aim to study the cause of death among chronic kidney disease patients associated with COVID-19.
Keywords
Cardiovascular disease, Coronavirus 2019, Chronic kidney disease, Respiratory failure
Introduction
Coronavirus disease which caused a worldwide pandemic in 2020 affecting more than 170 countries chronic kidney disease can be classified under kidney improving global outcome classification of CKD (KDIGO).
The causes of CKD vary but among them, diabetes and hypertension are the most common, but in developing countries like India, factors like patients have higher risk of serious complications that includes cardiovascular disease, hyperlipidemia, anemia, metabolic bone disease. So they require adequate treatment to reduce the complications and increase the chances of survival.
Among non-communicable diseases CKD is one of the most important contributors causing death in patients but diseases like COVID-19 can further aggravate the severity in CKD patients as they are immune prone. It is very important to understand how it causes damage to the kidneys
Chronic kidney disease patients have shown the increased higher incidence of COVID-19 and increased mortality CKD is relevant comorbidity been correlated with increased mortality when compared to the normal population [1].
Literature Review
Kidney involvement in COVID-19
Failure of one organ leads to the failure of another organ, mainly cardiovascular disease is seen in the patients who had a gradual decrease in renal function. It is the main factor responsible for death in many dialysis patients.
Hypertension associated with CKD is one of the main factors playing a role in the progressive decline of kidney function so patients with high blood pressure. Need frequent monitoring modifications in lifestyle like regular exercises and dietary salt intake can help further.
In CKD, anemia is mainly due to the deficiency of the erythropoietin and also in the patients who are undergoing hemodialysis where nearly 1-3 grams/year of iron stores are lost and some of the other causes include uremia associated dysfunction of platelets and also due to repeated phlebotomy and trapping of blood inside the dialysis apparatus and many of the patients have a functional iron deficiency which includes there’s abnormal release of iron stores that are needed to fulfill the body demands [2].
Sepsis the leading cause of death in patients with CKD, hemodialysis catheters are often responsible for the hospital acquired infection. CKD play an important role in the occurrence of pulmonary hypertension. Thickening of alveolar wall is seen due to deposition of extracellular matrix in CKD patients.
The sudden cause of death in CKD is due to cardiac arrest and arrhythmias due to shift in electrolytes. Pulmonary edema may develop in CKD patients due to excessive inter dialytic more increase in weight, improper dry weight prescription.
Kidney plays a major role in balancing body minerals like calcium and phosphorous it is mainly due to abnormality in activation of vitamin D3 and failure to excrete phosphorous in urine which results in hyper phosphatemia these patients are more prone to left ventricular hypertrophy.
Magnesium plays an important role in calcification of vessels, as higher levels of magnesium can prevent hydroxyapatite crystal formation which plays a prominent role in vascular calcification.
In CKD there is electrolyte imbalances like hypo magnesemia therefore serum magnesium levels are carefully monitored. Monitoring of potassium levels in blood is very essential life threatening hyperkalemia is developed due to over administration or leakage from intracellular pools or reduced excretion conversely during RRT hypokalemia may develop. The inability of kidneys to eliminate free water load may develop hypotonic hypo natremia.
Retention of salt and water causes concentric left ventricular hypertrophy because of low levels of calcium in blood. There is a release of parathyroid hormone which increases blood calcium levels by resorption of bone [3].
Being returned in to the body, mainly hemodialysis done 3 times a week. Each session lasts for about 4-5 hours.
Whenever there’s an increased level of urea in blood many of the patients suffer from variety of symptoms like fatigue, anorexia sleep disturbances, nausea and pruritus. The quality of life is affected because of pruritus.
There is nearly 10 times increased risk in CKD patients to develop AKI particularly in patients admitted in ICU due to COVID-19 the patients get admitted in the ICU to undergo mechanical ventilation it increases the chance of developing AKI and it leads to worsening of CKD reliability of serum creatinine may be affected because of fluid overload and wasting of muscles, intermittent HD or continuous renal replacement therapy is given in the patients by using temporary vascular access catheter.
In stage 4-5 chronic kidney disease, acid base disorder is seen when GF decreases less than 25% of normal patients it happens because of the inability of the kidneys to reabsorb bicarbonate and to excrete ammonia in more severe disease conjugate anions of acids cannot be excreted as a result high anion gap acidosis is seen [4].
Uremic acidosis which happens in advanced CKD disease depends upon the endogenous acid production and also from exogenous sources like ingestion of fruits, vegetables. Calcification is mainly due to the increased calcium phosphate product which resulted in heart failure intervention is required mainly when there is calcification of cardiac valves like aortic valve.
Good control of blood pressure is vital for the protection of the kidneys, drugs like ACE inhibitors should be taken properly and high cholesterol should be controlled by using statins swelling in the hands, ankles, face should be reduced by using medications like furosemide and proper maintenance of fluid input and output, most of the patients with anemia should be treated with intravenous iron preparations as well as with injection erythropoietin which is deficient due to damage of kidneys, if the patients have lower calcium levels and higher phosphate levels then they had given phosphate binders like calcium acetate [5].
It is possible to continue living with severe kidney disease for many years or even decades with the help of dialysis. A quite difficult which is not always possible for people with severe kidney disease is kidney transplantation, in that case while waiting for a donor kidney, its necessary to RRT with dialysis. If there is any worsening of kidney function despite giving all the medications, then the patient undergo dialysis which includes hemodialysis and peritoneal dialysis, in hemodialysis blood is transported into an external machine and it gets filtered before entering into body.
Home HD is possible only if the family member has been trained at dialysis center and it also needs to be enough space at home for dialysis machine [6].
Small procedure is done before initiation of several weeks of dialysis; it involves connecting a vein and an artery in the forearm, it leads to formation of larger blood vessel through which dialysis cannula can be inserted. There is another method called peritoneal dialysis where blood is not taken outside the body, but it is filtered in the peritoneal space with the help of dialysate fluid. About 2 liters of fluid transported into the abdominal cavity with the help of an abdominal catheter, after some time dialysis fluid is replaced with new dialysis fluid it happens at home [7].
Methods
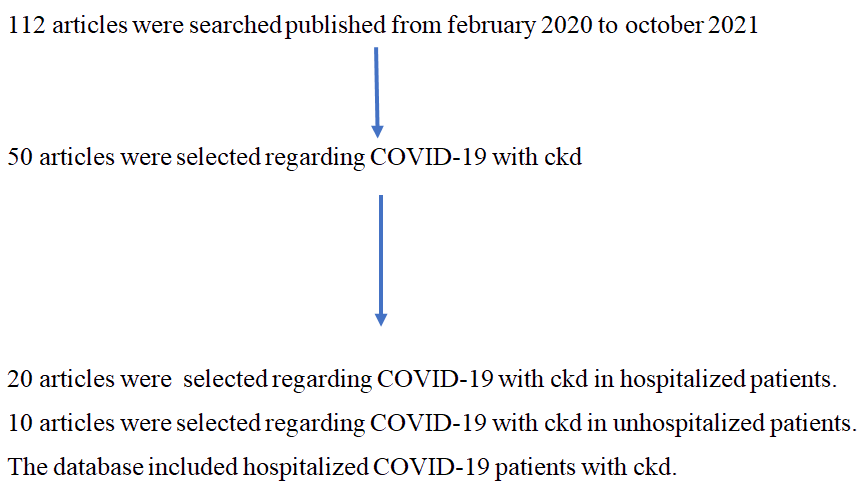
We searched Google scholar, Scopus, Research gate, Medline, PubMed and WHO and NTEP sites to understand the reasons for death in COVID-19 patients associated with chronic kidney disease we limited our search to relevant English language publications from recent years.
Discussion
CKD patients have a more vulnerable to infection mainly due to an impaired immune response, chronic inflammation and endothelial dysfunction lymphopenia.
We study the cause of deaths in COVID-19 patients associated with chronic kidney disease:
• Cause of deaths in COVID-19 patients associated with CKD in un-hospitalized patients.
• Cause of deaths in COVID-19 patients associated with CKD in hospitalized patients.
• Importance of dialysis in chronic kidney disease patients how it plays a role in preventing the death of patients in COVID-19 patients.
• Role of acute kidney injury in COVID-19 patients associated with chronic kidney disease.
• Role of drugs in COVID-19 patients associated with CKD.
Cause of deaths in COVID-19 patients with CKD in unhospitalized patients
In un-hospitalized patients, disruption in access to dialysis care due to lock down as most of the patients are unable to reach their hospital due to travel barriers. Some of the people faced increased charges and the remaining people are refused to treatment due to presence of COVID-19. Complications accompanying CKD are some of the reasons for bad prognosis in patients with COVID-19. Cardiovascular diseases like heart failure and aortic valve calcification, anemia and hypertension, are the most important complications of CKD [8].
Cause of deaths in COVID-19 patients associated with CKD in hospitalized patients
In the hospitalized patients, who are on severe critical disease, age, thrombocytopenia high AST levels, any previous history of cardiovascular disease during admission. Hemodialysis, lymphopenia and high serum LDH levels are associated with increased risk of infection leading to death [9].
Importance of dialysis in chronic kidney disease patients how it plays a role in preventing death of patients in COVID-19 patients
There are very limited capacities for accommodation of patients on maintenance hemodialysis, as most of them are occupied by acute kidney injury patients and critically sick patients. Due to low public spending on health care, most of the dialysis service is predominantly private sector’s most of the population nearly 2/3rd lives in rural areas where there is limited hemodialysis and they need to travel nearly more than 50 kms to access hemodialysis. Due to the shortage of surgeons, radiologists and intervention nephrologist, care of vascular access is another care of concern that leads to poor vessel protection [10].
There are high chances of mortality that are undergoing maintenance hemodialysis. They are the most vulnerable population as they are having other associated diseases diabetes mellitus, hypertension and other cardiovascular diseases they need to travel 3 times a week to hemodialysis center. It was difficult to maintain social isolation rules for the prevention of exposure an early diagnosis and timely start of treatment is necessary in this patient to prevent mortality.
In Spain mortality was high in more elderly population a study from New York, 419 patients who had undergone hemodialysis and peritoneal dialysis hospitalized with COVID-19, nearly all 133 patients had death and mechanical ventilation is required by 89 patients [11]. Recent study from us includes 567 maintenance hemodialysis patients, nearly 91 patient’s required mechanical ventilation and 134 patients required ICU admission. Most of the patients who died has age above 63 years and have cardiovascular disease and chronic obstructive pulmonary disease.
A recent study from the UK nearly 36% of patients who are on maintenance hemodialysis were managed as outpatients where dialysis was done in hospital isolation facilities and following clinical improvement in satellite units. 64% needed hospital admission. Among the patients whoever receiving hemodialysis nearly 22.8% had undergone death and where age is a significant factor under 50 years of age mortality rate is 11% and above 80 years mortality rate is 32.2% which is significantly higher as compared [12].
In a recent study from India by Trivedi M 38% of the patient on MHD got expired. Recently collected data from four institutes of India shows nearly 12.5 percent of dialysis patients got COVID-19 infection.
Role of acute kidney injury in COVID-19 patients associated with chronic kidney disease
One of them mentioned that there is higher mortality in patients with COVID-19 with chronic kidney disease with acute kidney injury when compared to patients with COVID-19 with chronic kidney disease.
Even the in hospital mortality rate was higher in CKD patients with AKI patients with stage 2 or more but earlier acute kidney injury diagnosis in CKD patients associated with COVID-19 results in favorable outcome. By comparing studies, people with CKD along with COVID-19 had higher mortality rate and requirements of mechanical ventilation. We are higher than the study with a mortality rate of COVID-19 with heart disease patients [12].
Role of drugs in COVID-19 patients associated with chronic kidney disease
Patients with severe renal disease are more susceptible to the development of severe Coronavirus disease remedesivir which is a nucleotide analog that inhibits viral RNA dependent RNA polymerase the active metabolite of this drug namely sulfobutylether–β- cyclodextrin is mainly excreted by the kidneys; it is accumulated in patients who are having reduced GFR.
It has been suggested close monitoring is required for the patient‘s with renal impairment for the usage of remdesivir, in some of the studies t was found that remdesivir is well tolerated in patients with AKI and CKD patients including those who were on dialysis. Many of the patients showed a mild increase of alt levels but they are not clinically significant.
In many of the studies, it was mentioned that remdesivir helps in faster recovery of the patient but it doesn‘t show any benefit in reducing mortality [13].
Favipiravir: Favipiravir an RNA dependent RNA polymerase inhibitor that is converted into an active substrate active phosphor ribosylated forms in cells which is recognized as a substrate by viral RNA polymerase and thus it inhibits RNA polymerase activity
Many of the patients with respiratory symptoms including those on ventilators got recovered.
Mild and reversible elevation of alp and γ-GTP s seen I is one of the most effective drugs for treating COVID-19 in severe renal disease careful monitoring of concentrations of favipiravir or its metabolites is required [14].
Corticosteroids: Corticosteroids are not recommended as it leads to an increase in the risk of super infection; it is beneficial in patients who had developed ARDS on progression [15].
Monoclonal antibody: Interleukin 6 is main pro inflammatory factors in uremic patients, mainly it is present as a mediator of acute phase response it increases the mortality and cardiovascular disease.
Tocilizumab a monoclonal antibody against the interleukin receptor is given as a single dose which is well tolerated and it has been found that it is one of the efficacious drugs [16].
Conclusion
The most important clinical application of this study is that patients with CKD of varying stages should require special care and vaccination by physicians and health care providers. Proper precautions should be taken at the dialysis center patients should be made aware regarding their body temperature and they should be keep track of his/her health daily the physician should be able to diagnosis COVID-19 and he should inform to COVID-19 center if suspected patient should be instructed to wear a mask and not to use public transportation when he/she is suspected of having COVID-19 until RT-PCR test comes patient should maintain certain distance from other distance until he reaches dialysis center private room isolation is recommended but when it is not available, there should be proper distance in between 2 beds when dialysis is performed the dialysis staff should PPE kit including disposable gowns, surgical asks goggles and face shields as the staff are more prone for infection and PPE kit should be properly disinfected proper change of bed sheets and pillowcase should be ensured for each patient and the equipment should be properly disinfected by using sodium hypochlorite 0.1% or alcohol 70% at dialysis station dialysis station should be properly ventilated.
Patients should maintain a proper diet as well as fluid balance regarding input and output the comorbidities like hypertension, diabetes and in this patient should be carefully treated.
References
- World Health Organization (WHO). Naming the Coronavirus disease (COVID-19) and the virus that causes it. Braz J Implantol Health Sci 2020; 2.
- Cheng Y, Luo R, Wang K, et al. Kidney impairment is associated with in hospital death of COVID-19 patients. Medrxiv 2020. [Crossref][Googlescholar][Indexed]
- Bello Ak, Alrukhaimi M, Ashuntantang GE, et al. Complications of chronic kidney disease: Current state, knowledge gaps and strategy for action. Kidney Int Suppl 2017; 7:122-129. [Crossref][Googlescholar][Indexed]
- Henry BM, Lippi G. Chronic kidney disease is associated with severe Coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol 2020; 52:1193-1194. [Crossref][Googlescholar][Indexed]
- Kikuchi K, Nangaku M, Ryuzaki M, et al. COVID-19 of dialysis patients in Japan: current status and guidance on preventive measures. COVID-19 task force committee of the Japanese association of dialysis physicians; Japanese society for dialysis therapy; Japanese society of nephrology, Ther Apher Dial 2020; 24:361-365. [Crossref][Indexed]
- Wang B, Li R, Lu Z, et al. Does comorbidity increase the risk of patients with COVID-19: Evidence from a meta-analysis. Aging 2020; 12:6049. [Crossref][Googlescholar][Indexed]
- Abdelaziz T. Kidney diseases and COVID-19 pandemic a review article. Open access Maced J Med Sci 2020; 8:103-107. [Crossref][Googlescholar][Indexed]
- Jain R, Dupas P. The effects of India's COVID-19 lockdown on critical non COVID health care and outcomes: Evidence from a retrospective cohort analysis of dialysis patients. Medrxiv 2021; 2020-2029. [Crossref][Googlescholar][Indexed]
- Chou CY, Wang SM, Liang CC, et al. Risk of pneumonia among patients with chronic kidney disease in outpatient and inpatient settings: A nationwide population based study. Medicine 2014; 93. [Crossref][Googlescholar][Indexed]
- Wang X, Fang X, Cai Z, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: A systemic review and meta-analysis. Research 2020; 19:2020. [Crossref][Googlescholar][Indexed]
- Goicoechea M, Camara LA, Macias N, et al. COVID-19: Clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int 2020; 98:27-34. [Crossref][Googlescholar][Indexed]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395:1054-1062. [Crossref][Googlescholar][Indexed]
- Roberto P, Francesco L, Emanuela C, et al. Current treatment of COVID-19 in renal patients: Hope or hype? Intern Emerg Med 2020; 28:1-10. [Crossref][Googlescholar][Indexed]
- Koshi E, Saito S, Okazaki M, et al. Efficacy of favipiravir for an end stage renal disease patient on maintenance hemodialysis infected with novel Coronavirus disease 2019. CEN Case Rep 2021; 10:126-131. [Crossref][Googlescholar][Indexed]
- Kikuchi K, Nangaku M, Ryuzaki M, et al. Survival and predictive factors in dialysis patients with COVID-19 in Japan: A nation wide cohort study. Ren Replace Ther 2021; 7:1-9. [Crossref][Googlescholar][Indexed]
- Nourie N, Chamaa MA, Mouawad S, et al. Effective treatment with tocilizumab in a COVID-19 patient on maintenance hemodialysis: A case report. CEN Case Rep 2021; 27:1-6. [Crossref][Googlescholar][Indexed]
Author Info
B Uma Maheswara Reddy*, Swarupa Chakole and Ashok Mehendale
Department of Community Medicine, Jawaharlal Nehru Medical University, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, IndiaCitation: B Uma Maheswara Reddy, Swarupa Chakole, Ashok Mehendale,Study of COVID-19 Virus Causing Deaths in Chronic Kidney Disease Patients, J Res Med Dent Sci, 2023, 11 (01):090-094
Received: 25-Oct-2022, Manuscript No. JRMDS-22-62858; , Pre QC No. JRMDS-22-62858 (PQ); Editor assigned: 28-Oct-2022, Pre QC No. JRMDS-22-62858 (PQ); Reviewed: 11-Nov-2022, QC No. JRMDS-22-62858; Revised: 30-Dec-2022, Manuscript No. JRMDS-22-62858 (R); Published: 07-Jan-2023
