Research - (2025) Volume 13, Issue 2
Study of Prune Belly Syndrome: An Underreported Rare Disease
Roshni Ravindran*, Harshitha Janardhan, Anupama Suresh and Malay Jhancy
*Correspondence: Roshni Ravindran, Department of Pediatrics, RAK Medical and Health Sciences University, Ras Al Khaimah, United Arab Emirates, Email:
Abstract
Introduction and objectives: Prune belly syndrome is a rare disease with an incidence rate of 1 per 40,000 live births and has a triad of clinical features like bilateral cryptorchidism, lax abdomen and urogenital defects. A 4 month old baby with prune belly syndrome who was admitted to the government hospital with complaints of recurrent urinary tract infection led us to do a short review of this disease. The review aims to evaluates the incidence of prune belly syndrome, identifies the common clinical presentation and evaluates the outcome of this syndrome published in the literature.
Methods: A literature search was conducted using keywords in different databases. Overall, 204 articles published from January 2010 to June 2021 on prune belly syndrome were screened, out of which 89 non duplicated articles were identified. Of these, 35 relevant articles were included.
Results: Most of the cases presented with multiorgan defects, in which the majority of children had gastrointestinal and genitourinary defects. The most common complications identified were renal failure and recurrent urinary tract infections. A small percent of patients have undergone surgical procedures as a part of the management. 16 (45.71%) patients died mostly due to the associated complications.
Conclusion: It has been noticed that at the time of detection, the disease has worsened or complications have developed leading to high mortality among affected children. Therefore, spreading awareness among parents and healthcare professions that early investigation and diagnosis along with a multidisciplinary approach can improve a patient's survival is extremely vital.
Keywords
Prune belly syndrome, Eagle barrett syndrome, Clinical features, Complications, Outcomes
Introduction
Prune Belly Syndrome (PBS) is a rare congenital condition, which was first described in 1839 by Frolich. It is also known as eagle barrett syndrome or mesenchymal dysplasia syndrome. PBS is diagnosed by a triad of clinical features like congenital absence of abdominal wall musculature with a prune-like appearance, bilateral cryptorchidism and defects of the urogenital tract. It affects 1 in 40,000 births globally, with 95% of cases seen in males. The etiology and risk factors of this syndrome remain unknown, although there are several hypotheses. An underlying genetic abnormality is under investigation. Some studies indicate an increased incidence of PBS in children born to younger mothers. There are very few cases of PBS occurring in association with trisomy 13, 18 and 21 to indicate an association with these chromosomes [1].
In particular, this review aims to emphasize on the importance of reporting rare diseases to benefit the children with similar diseases and the medical fraternity. Importantly, the review evaluates the incidence of prune belly syndrome, identifies the common clinical presentation and evaluates the outcome of this syndrome published in the literature [2].
Materials and Methods
This is a short literature review on incidence, clinical features and outcomes of prune belly syndrome published between 2010-2021. All the 204 published articles on PBS from January 2010 to June 2021 were collected in a literature search using the keywords Prune Belly Syndrome (PBS) or Eagle Barrett syndrome and clinical features and complications and outcomes from databases like PubMed, Medline, Google Scholar, Scopus and ProQuest. 89 non duplicated articles were screened again. 35 articles that described the clinical features and outcomes of PBS were included in this review. Articles published in languages other than English and not relevant to this syndrome were excluded (Figure 1) [3].
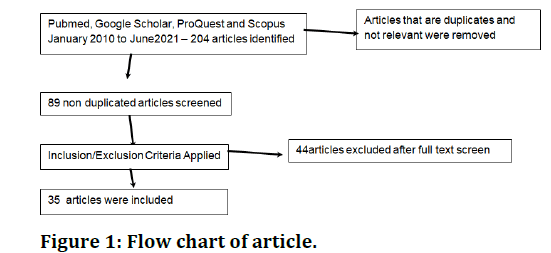
Figure 1: Flow chart of article.
Results
Table 1 illustrates the common clinical presentation and outcomes of PBS. Among the 35 articles that were reviewed, the main clinical features of this syndrome are absence of abdominal wall muscles, which was seen in 13 (37.14% of cases), bilateral cryptorchidism and hydronephrosis that were present in 26 (74.28% of cases) and 17 (48.57% of cases) respectively. Some of the common anomalies associated with PBS are: Urogenital abnormalities, gastrointestinal tract abnormalities, musculoskeletal and respiratory abnormalities (Table 2)[4].
| Clinical features | No. (percentage) |
|---|---|
| Urogenital defects | 26 (74.29%) |
| Gastrointestinal | 20 (57.14%) |
| Respiratory abnormalities | 8 (22.86%) |
| Cardiovascular anomalies | 5 (14.29%) |
| Musculoskeletal defects | 9 (25.71%) |
| Renal failure | 5 (14.29%) |
| Recurrent UTI | 7 (20%) |
| Respiratory failure | 5 (14.29%) |
| Termination of pregnancy | 4 (11.43%) |
| Fetal deaths | 16 (45.71%) |
| Follow up | 13 (37.14%) |
| Orchidopexy | 7 (20%) |
| Abdominoplasty | 8 (22.86%) |
Table 1: The clinical presentation and outcomes of PBS.
| Musculoskeletal abnormalities | No. (Percentage) |
|---|---|
| Scoliosis | 3 (8.57%) |
| Deformed thoracic cage | 3 (8.57%) |
| Hip dysplasia | 1 (2.86%) |
| Bilateral club feet | 8 (22.86%) |
| Potter’s facies | 2 (5.71%) |
| Other musculoskeletal anomalies | 2 (5.71%) |
| Tricuspid regurgitation | 2 (5.71%) |
| Ventricular septal defect | 2 (5.71%) |
| Mesocardia | 1 (2.86%) |
| Hypoplastic lung | 8 (22.86%) |
| Cleft lip and cleft palate | 2 (5.71%) |
| Laxity of the abdominal skin | 20 (57.14%) |
| Distended abdomen | 11 (31.42%) |
| Absent abdominal muscles | 13 (37.14%) |
| Ascites | 3 (8.57%) |
| Imperforate anus | 6 (17.14%) |
| Other gastrointestinal tract problems | 5 (14.29%) |
| Hydronephrosis (unilateral and bilateral) | 17 (48.57%) |
| Dysplastic kidney | 1 (2.86%) |
| Renal agenesis | 2 (5.71%) |
| Hydroureter | 17 (48.57%) |
| Megacystitis | 10 (28.57%) |
| Vesicoureteric reflux | 5 (14.28%) |
| Bladder diverticulum | 2 (5.71%) |
| Hypoplastic urethra | 1 (2.86%) |
| Ambiguous genitalia | 2 (5.71%) |
| Penile aplasia | 1 (2.86%) |
| Patent urachus | 3 (8.57%) |
| Bilateral cryptorchidism | 26 (74.26%) |
| Rare urogenital defects | 10 (28.57%) |
Table 2: The clinical presentations of PBS .
According to our analysis, genitourinary abnormalities were found in 26 (74.29%). The most common urogenital anomaly associated with PBS is bilateral cryptorchidism. Bilateral hydronephrosis was reported in 17 (48.57% of cases). 17 (48.57% of cases) were found to have hydroureter. Megacystitis was seen in 10 (28.57%) of patients and 3 (8.57% of patients) had patent urachus. Other findings like ambiguous genitalia were reported in 2 (5.71%) (Figure 2) [5].
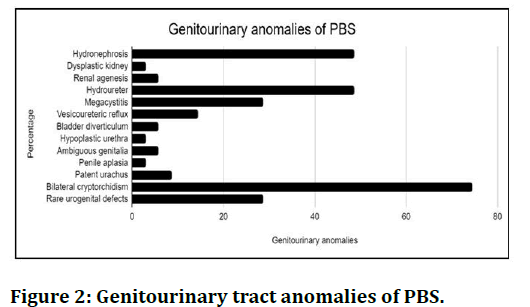
Figure 2: Genitourinary tract anomalies of PBS.
The second most common abnormality is the involvement of the gastrointestinal tract seen in 20 (57.14%) reports. The laxity of the abdominal skin was seen in the majority of cases 20 (57.14%), whereas distended abdomen was seen in 11 (31.42%) cases. Other gastrointestinal defects like cleft lip and cleft palate were found in 2 (5.71% cases), ascites in 3 (8.57%) and an imperforate anus on physical examination was found in 6 (17.14%) of patients (Figures 3 and 4) [6].
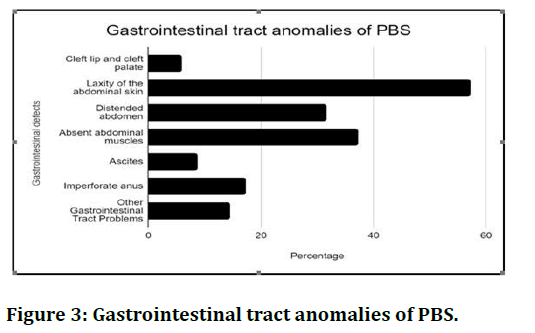
Figure 3: Gastrointestinal tract anomalies of PBS.
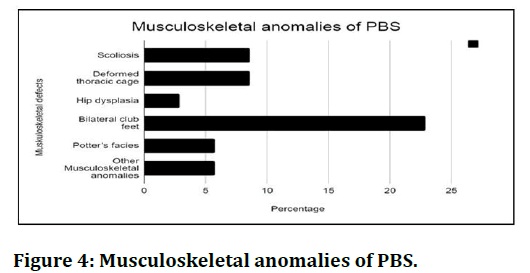
Figure 4: Musculoskeletal anomalies of PBS.
Musculoskeletal and pulmonary abnormalities
Some of the musculoskeletal abnormalities found were scoliosis 3 (8.57%) of cases, lower limb anomalies like club foot 8 (22.86%), thoracic anomalies such as a deformed thoracic cage 3 (8.57%). Potter’s facies was observed in 2 (5.71%) of patients only. Pulmonary hypoplasia due to oligohydramnios during pregnancy was seen only in complicated cases. On reviewing the radiological scans, 8 (22.85%) cases had lung hypoplasia and 1 (2.86%) patient was found to have hip dysplasia (Figure 3) [7].
Lastly, cardiovascular abnormalities are rarely seen in PBS. Only 5 (14.29%) were noted to have these anomalies. Other less common CVS anomalies to list are ventricular septal defect, mesocardia and tricuspid regurgitation [8]. After the data collection, the complications of this syndrome were renal failure, which was present in 5 (14.29%) of cases, respiratory failure in 5 (14.29%) cases and recurrent urinary tract infection, which was seen in 7 (20%) of cases. Some studies have suggested that cases with respiratory infection improved on treatment while other cases deteriorated, resulting in death.
Majority of patients were treated with multiple surgical procedures, mostly abdominoplasty 8 (22.86%). On the other hand, 7 (20%) of them underwent orchidopexy. From the collected data, 4 (11.43%) of pregnancies were terminated. 16 (45.71%) of patients died immediately after birth. A multidisciplinary approach was implemented to manage the children who survived after birth due to the complexity of this syndrome. Surgical interventions were associated with excellent outcomes in the patients affected with PBS. 13 (37.14%) children were followed over a long term period. Some children died as their parents had refused treatment [9].
Discussions
Prune Belly Syndrome (PBS) is identified by a triad of cardinal features that include abdominal wall muscle defect, bilateral undescended testes and renal system abnormalities. Other associated features include respiratory (e.g. pulmonary hypoplasia), cardiac (e.g. Tetralogy of Fallot, VSD), gastrointestinal (e.g. intestinal malrotation) and skeletal anomalies (e.g. club foot). The absence or mild presentation of any one of the given three cardinal features will lead to the diagnosis of pseudo prune syndrome (incomplete type of PBS), which is mainly seen in female patients. The etiology and pathogenesis for PBS remain unknown till date. There are many hypotheses postulated regarding the development of PBS, out of which two hypotheses are taken into consideration. According to the first theory, mesenchymal developmental defects occurring between the 6th and 10th week of gestation result in maldevelopment of the abdominal wall musculature and urinary tract. According to the second theory, an abnormal development of the urinary tract causes obstruction which decreases the urine outflow, ultimately leading to hydronephrosis, hydroureters and megacystis followed by poor development of the muscles of the abdominal wall and urinary tract [10].
PBS is common in both monozygotic and dizygotic twin pregnancies. The pathogenesis of the sporadic form of PBS can be explained by the presence of an abnormal hepatocyte nuclear factor 1b (HNF1b) expressed on chromosome 17 and this factor is also found in the derivatives of the mesonephric duct and the renal tubules of the metanephros. A fetus with PBS can be diagnosed using an antenatal ultrasound scan in the first and second trimester of pregnancy by mainly looking for fetal ascites, oligohydramnios, dysplastic kidneys or hydronephrosis, hydroureters and distended bladder. However, if it is not detected during pregnancy, it can also be diagnosed at birth by identifying the clinical features during newborn examination [11].
In addition to the newborn examination, complete blood count, electrolytes, urinalysis, renal function test, urinalysis and measurement of creatinine levels are performed as a part of the investigation. Renal and bladder ultrasound is performed to detect the urinary tract abnormalities and its related complications. Also, kidney, ureter and bladder x-rays can be used to confirm the presence of renal malformations. Ascending urinary tract infections can also be ruled out with the help of an intravenous pyelogram. An early diagnosis and a multidisciplinary approach to the management is crucial to improve the quality of life and survival rate in patients with PBS. Patients with hydronephrosis have complaints of recurrent urinary tract infections as in our index case and these children are managed conservatively with antibiotics. More importantly, a child's parents should be instructed to perform a clean intermittent catheterisation at home. Scheduling monthly follow up visits to monitor fluids and electrolytes, renal function and serum creatinine levels is vital [12].
Surgical interventions like orchidopexy, urinary tract reconstruction and abdominoplasty are the mainstay of treatment. This review confirms the same that 18.5% of patients underwent abdominoplasty and 14.81% of patients underwent orchidopexy. Multiple surgeries can be done in one sitting, to limit the number of general anesthetics which may benefit children with pulmonary problems. Abdominal wall reconstruction can be performed for cosmetic reasons, as well as for improving the bowel and bladder function. According to the recent guidelines, orchidopexy should not be delayed until the adolescent age except in the presence of any cardiopulmonary issues. Kidney transplantation is the treatment of choice in patients with end stage renal disease, as it provides an improved survival rate over dialysis. The differential diagnosis of PBS are pseudoprune belly syndrome, prune belly-like variant, megacystis microcolon intestinal hypoperistalsis syndrome, ureterocele, urethral atresia and posterior urethral valve. Posterior urethral valve has a keyhole sign and this sign is not an indication of cryptorchidism. In megacystis microcolon intestinal hypoperistalsis syndrome, polyhydramnios is present and females are more commonly affected [13].
The untreated prune-belly syndrome patients subsequently develop complications such as intrauterine fetal death, respiratory failure and chronic renal failure. Infertility and testicular malignancy are reported due to the delayed correction of bilateral cryptorchidism [14]. Generally, the prognosis of PBS is often indicated by the presence of respiratory failure and kidney failure. Respiratory failure is one of the major causes of mortality. In terms of renal function, patients with a normal renal function are at a low risk of developing renal complications and have a mild clinical presentation and good outcome. 25% of patients who suffer from renal failure have a poor outcome [15].
Conclusion
Prune belly syndrome is a rare genetic and underreported disorder with a high morbidity rate. For a favourable outcome, PBS should be diagnosed as early as possible. As it is a condition with variable severity and multisystemic manifestations, patients are best managed by a multidisciplinary approach. Even though the survival rate for PBS has improved with earlier diagnosis and intervention, the mortality rate still remains high with the majority of deaths occurring in the perinatal period due to renal and respiratory failure.
Acknowledgement
We thank Dr. Malay Jhancy and Dr. Anshad Ummer for guiding us.
Funding Source
No funds were used or taken for this research.
Conflicts of Interest
No conflicts of interest.
References
- Sarhan OM, Al-Ghanbar MS, Nakshabandi ZM. Prune belly syndrome with urethral hypoplasia and vesico-cutaneous fistula: A case report and review of literature. Urol Annals 2013; 5:296.
[Crossref] [Google Scholar] [PubMed]
- Giuliani S, Vendryes C, Malhotra A, et al. Prune belly syndrome associated with cloacal anomaly, patent urachal remnant and omphalocele in a female infant. J Pediatr Surg 2010; 45:e39-e42.
[Crossref] [Google Scholar] [PubMed]
- Ngwanou DH, Ngantchet E, Moyo GP. Prune-Belly syndrome, a rare case presentation in neonatology: About one case in Yaounde, Cameroon. Pan African Med J 2020; 36:102.
[Crossref] [Google Scholar] [PubMed]
- Baydilli N, Selvi I, Akınsal EC. A rare case: Congenital megalourethra in prune belly syndrome. Arch Case Rep 2018; 2:001-003.
- Singh AP, Mathur V, Tanger R, et al. Partial prune belly syndrome: A rare case report. Med J Dr DY Patil Univ 2017; 10:470.
- Hakimi T, Ibrahimi MA. A rare case report of prune belly syndrome with malnutrition. Oxford Med Case Rep 2021; 2021:omab017.
[Crossref] [Google Scholar] [PubMed]
- Fette A. Associated rare anomalies in prune belly syndrome: A case report. J Pediatr Surg Case Rep 2015; 3:65-71.
- Bacha R, Gilani SA, Manzoor I, et al. The mechanism of prune belly syndrome development: A sonographic sequential assessment. J Diagn Med Sonogr 2020; 36:594-603.
- Haeri S, Devers PL, Kaiser-Rogers KA, et al. Deletion of hepatocyte nuclear factor-1-beta in an infant with prune belly syndrome. Amer J Perinatol 2010; 27:559-563.
[Crossref] [Google Scholar] [PubMed]
- Kayinda F, Sekimwanyi G. Prune belly syndrome: A rare congenital malformation in a 6-year-old Ugandan male. East Central Afr J Surg 2019; 24:150-153.
- Gupta MK, Chaudhary G, Yhoshu E. A novel technique of abdominoplasty for prune belly syndrome. Afr J Paediatr Surg 2020; 17:108.
[Crossref] [Google Scholar] [PubMed]
- Demisse AG, Berhanu A, Tadesse T. Unusual presentation of prune belly syndrome: A case report. J Med Case Rep 2017; 11:1-4.
[Crossref] [Google Scholar] [PubMed]
- Byon M, Kim GJ. Prune-belly syndrome detected by ultrasound in the first trimester and the usefulness of vesicocentesis as a modality of treatment. Obste Gynecol Sci 2013; 56:265-268.
[Crossref] [Google Scholar] [PubMed]
- Levin TL, Soghier L, Blitman NM, et al. Megacystis-microcolon-intestinal hypoperistalsis and prune belly: Overlapping syndromes. Pediatr Radiol 2004; 34:995-998.
[Crossref] [Google Scholar] [PubMed]
- Satar M, Ozlu F, Yapicioglu H, et al. Corset usage for gastrointestinal and respiratory problems in a newborn with prune belly syndrome. Indian J Pediatr 2016; 83:717-719.
[Crossref] [Google Scholar] [PubMed]
Author Info
Roshni Ravindran*, Harshitha Janardhan, Anupama Suresh and Malay Jhancy
Department of Pediatrics, RAK Medical and Health Sciences University, Ras Al Khaimah, United Arab EmiratesCitation: Roshni Ravindran, Harshitha Janardhan, Anupama Suresh, Malay Jhancy, Review of Prune Belly Syndrome: An Underreported Rare Disease, J Res Med Dent Sci, 2023, 11 (08): 018-022.
Received: 01-Nov-2021, Manuscript No. JRMDS-23-46193; , Pre QC No. JRMDS-23-46193 (PQ); Editor assigned: 04-Nov-2021, Pre QC No. JRMDS-23-46193 (PQ); Reviewed: 18-Nov-2021, QC No. JRMDS-23-46193; Revised: 19-Jul-2023, Manuscript No. JRMDS-23-46193 (R); Published: 16-Aug-2023, DOI: -
