Research - (2021) Volume 9, Issue 5
Study on Maternal Complications and Outcomes in GDM to Identify Neonatal Morbidity in Gestational Diabetes Mellitus Patients
Abinaya Vijayan, V Kalavathy and K Vani*
*Correspondence: K Vani, Department of Obstetrics and Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
The Present study focuses on to evaluate the maternal and fetal outcome depending on Glycaemic variability in Gestational Diabetes Mellitus patients. A prospective, randomized study was designed to list maternal complications and outcomes in GDM, and to identify neonatal morbidity associated with this condition.
Keywords
Glycaemic, Diabetes, GDM, Fetal outcome, Maternal complications
Introduction
Diabetes is the most common pre-existing medical condition complicating 2 to 3% of pregnancies; 90% of these cases present with GDM.Gestational diabetes mellitus (GDM) is a condition of pregnant woman where glucose intolerance is found during pregnancy. GDM usually develops during pregnancy and ends after pregnancy. GDM is the mild form of diabetes mellitus and can be controlled by exercise and carbohydrate diet having low glycemic index the majority of women with histories of gestational diabetes are obese; having sedentary life styles vegetables and fruits. Glucose is not properly regulated in 3-10% of all pregnancies. GDM is the glucose intolerance of variable degree with onset or first recognition during pregnancy. It is affecting 90% of cases of diabetes mellitus during pregnancy. Annually 21 million people of the world (7% of the population) are reported with some form of diagnosed diabetes; another 6 million people are reported with undiagnosed type2 diabetes among women of childbearing age. Currently, type 2 diabetes mellitus are affecting 8 % of cases of diabetes mellitus in pregnancy, and preexisting diabetes mellitus accounts for 1 % of all pregnancies. The various factors that will predict the pregnant woman to become diabetic in future are early diagnosis of GDM in pregnancy, need for insulin treatment during pregnancy, high blood glucose levels at diagnosis, preterm delivery, macrosomic babies and an abnormal oral glucose tolerance test after two months of delivery. During GDM pregnancy, the fetus is exposed to high level of glucose which results in excess fetal growth, impaired insulin secretion and decreased insulin sensitivity. The short term complications of excess infant birth weight are shoulder dystocia and infant hypoglycemia. The altered fetal metabolism may result in impaired glucose tolerance during early youth and adolescence. The risks associated with GDM are well established, however its impact on health of mothers and the neonates are less clear. The factors that have already reported to influence the risk of GDM among mothers are previous history of GDM, family history of diabetes, obesity, recurrent urinary tract infections, infertility treatment, unexplained neonatal death , macrosom1c babies , pre mat urit y, pre-eclampsia and advanced maternal age. Poorly controlled GDM consequences are evident, but still no proper consensus exists on either diagnostic criteria or metabolic aims in controlling GDM. Traditionally GDM is taken as a disorder of carbohydrate metabolism; thus, blood glucose levels have become the main key player for controlling and directing treatment during pregnancy mothers should be examined and diagnosed during early pregnancy and they should have regular postpartum checkup for recognition and management of any other complications. GDM is a disorder which can be effectively controlled by decreasing the associated high-risk factors and thus leading to healthy infant delivery. Thus, accurate monitoring and proper management of GDM women will results in improved maternal and neonatal consequences.
Gestational diabetes does recur in about 60% of subsequent pregnancies and 40% of these will develop non-insulin dependent diabetes within 15 years after delivery which was the background for the original diagnostic criteria. It is important to identify pregnant women with gestational diabetes because it is associated with significant metabolic alterations, increased perinatal morbidity and mortality, maternal morbidity and exaggerated long-term morbidity among the mothers and their off springs. If GDM is not properly treated, there is an increased risk of adverse maternal (preeclampsia, pregnancy induced hypertension, recurrent vulva-vaginal infections, operative deliveries, obstructed labor and development of diabetes mellitus later m life), fetal (macrosomia, polyhydromnios, preterm labour, respiratory distress unexplained intrauterine fetal death, traumatic delivery) and neonatal complications (hypoglycemia, jaundice, polycythemia, tetany, hypocalcemia, hypomagnesaemia). GDM is fast becoming a major health problem in developing countries undergoing rapid changes in lifestyle, dietary habits and body mass index. Both maternal and neonatal mortality and morbidity resulting from GDM can be prevented by proper antenatal supervision and institutional care, facilities that exist in our tertiary care units and even 1n most of the primary health centers. The major hurdles to crossed in our country include lack of education and socio-cultural taboos leading failure of screening of high-risk pregnancies and their referral to the appropriate health facilities at the proper time.
Glucose is produced because of maternal metabolism principally from carbohydrate in the diet and from the gluconeogenic amino acids. The hormone insulin, in turn, regulates glucose. Pedersen hypothesized that in maternal diabetes, high concentrations of glucose give rise to increased nutrient transfer to the fetus. To prevent fetal hyperglycemia, fetal insulin secretion and fetal growth increase. This relation is supported by observations of gestational and pregestational diabetes that higher maternal glucose concentrations, generate controversy in part because glucose is the primary focus, and there is little control for factors that potentially confound the relation between glucose and fetal growth. There is another underlying issue. While higher maternal glucose concentrations may lead to increased fetal growth, they also are associated with pregnancy complications when the mother has diabetes. A smaller literature also suggests that among nondiabetic gravidas, higher glucose concentrations are associated with increased operative delivery as well as pregnancy-induced hypertension. We wanted to determine whether these relations were present in our data and whether a higher glucose concentration also was associated with chorioamnionitis. Chorioamnionitis. 1s a manifestation of subclinical infection(s) associated with preterm delivery. Gestational diabetes mellitus (GDM) and maternal obesity are independently associated with adverse maternal and neonatal outcomes. Both share common metabolic characteristics such as increased insulin resistance, hyperglycemia, and hyperinsulinemia, and GDM may impart distinct effects on clinical outcomes independent of obesity alone. The same is true for maternal ob esit y, although differences in metabolism may also exist among certain ethnic groups. Therefore, examination of the combined association of these common metabolic problems with pregnancy outcomes is an important question. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study offers a unique opportunity to examine the independent associations of GDM and obesity alone and in combination with adverse pregnancy outcomes [1-19].
Materials and Methods
This prospective study was carried out in Sree Balaji Medical College & Hospital, Chrompet, Chennai m Department of Obstetrics & Gynaecology.
This study was spread over a period of 18 months from December 2013 - May 2015.The study population consisted of 100 GDM patients.
Inclusion criteria
Diagnosis of GDM.
Exclusion criteria
✓ Diabetic before pregnancy.
✓ Pre gestational BMI > 35kg/m2.
✓ HbAlC > 8%.
✓ Asthma.
✓ Epilepsy.
✓ Known hypertension heart problems those who received blood, plasma or immunoglobulin within the last 3 months of participation those diagnosed with malignancy or immunodeficiency diseases.
✓ Patients with severe medical or psychological co morbidity.
Screening of maternal complication and neonatal outcome
As part of GDM investigations, all the patients were provided dietary counselling, Ultrasound follow, and maternal complication & fetal outcome was recorded in this study, Maternal: Hypertension, Preclampsia, Uterine growth restriction, Antepartun Hemorage, UTis, Premature raptures of membranes, Preterm Labour, Mode of deliveries, ligohydramnios, stillbirths, Miscarriageand Polyhydramnios were observed. Fetal: Birth weight, Hypoglycemic neonates, Hypocalcemic neonates, Phototherapy required, Neonates with RDS, Ma crosomia , Birth trauma, Jaundice and Congenital anomalies were recorded.
Measurement glycemic varibility
During the study, all antenatal women who attended the OP were screened for GDM by determining both fasting and postprandial blood glucose level in each trimester by continuous blood glucose monitoring. If the fasting blood glucose level was > 100 mg /dL and postprandial blood glucose level was > 140mg/dL, the pregnant women were identified for GDM along with HbAlc levels 2: 5.5 % in first trimester. The identified GDM women then underwent.for 75g two hours ora l glucose challenge test and six-point profile test (SPPT) for the confirmation of GDM in second trimester and third trimester respectively.
Variability measures from glycemic excursions
The most used index to evaluate the glycemic excursion is the MAGE, defined as MAGE. The MAGE index is highly correlated with SD, so it is sometimes used as a substitute for SD. Moreover, the choice of the index parameters is made by the investigator, making it hard to compare results obtained on different datasets from different researchers. Also consider excursions happening on a change of day are not con red , and, most importa nt, there is not a clear definition for the definition of what should be considered an excursion. Day-to-Day Variability A popular tool used to quantify the variability on two consecutive days 1s the Mean of Daily Differences (MODD), The peculiarity of MODD is that it was originally defined from sta nd ard ized conditions, i.e. the patient was monitored for m days (typically 2) in the same conditions with invasive sampling of blood drawn at the same time of day to allow a comparison between the m days. The advent of CGM devices renders the use of MODD easier, since it is possible to compare several days monitored with frequent measurements.
Short-term variability
An index called Continuous Overlapping Net Glycemic Action (CONGA), proposed by Nathan et al. m, evaluates - a within day variability. In practice, SD 1s evaluated for a time-series composed by the differences between the glycemic value and the glycemic value collected m hours later. The quality of glucose control is high if a patient can correctly tune the carbohydrate ingestion and insulin dosing in such a way that the glycemic range stays within the safety zone with few counteractions and corrections.
The most used parameter for the evaluation of quality of glucose control is the relative time spent by the subject in different regions of the whole glycemic scale. For the clinician it is important to understand the percentage of time spent on target relative to the whole monitoring session, but also to distinguish cases where the percentage out of target is spent above or below the target zone. Of course, a subject who spends 0st time in hyperglycemia needs to refine the therapy with more intensive insulin dosing, while a subject who tends to stay in hypoglycemia for prolonged time probably needs to reduce the insulin dosing.
Results
After collection of data from 100 pregnant women with GDM, analysis was done on the following: Glycemic variability values were classified into four categories such as, mild variability (SD=1 to 5), moderate variability (SD=6 to 10) , High variability (SD=11 to 15) and extreme high variability (SD=16 to 20). Glycemic variability was determined by comparison of standard deviation of individual's each trimester blood glucose level. The percentages of mild variability, moderate variability, High variability, and extreme high variability were 42%, 31%, 18% and 9% respectively. The glycemic variability also calculated by mean of six-point profile test and it was compared with mean of fasting and postprandial blood glucose in first and sec6 trimester. The variability was higher when compared to the first trimester and less when compared to second trimester. The percentages of mild variability, moderate variability, High variability, and extreme high variability were 51%, 28%, 13% and8%respectively Gestational diabetes mellitus (GDM) is a condition of pregnant woman where glucose intolerance is found during pregnancy, and it is associated with increased risk of serious perinatal morbidities and mortalities, as well maternal morbidities. With this notion our study was aimed to calculate the glycemic variability and to compare the maternal and fetal outcome of gestational disabetes mellitus. An informed consent, proforma and human ethical clearance for sample collection was obtained.
GDM women were more prone to pregnancy induced hypertension (32%), preeclampsia (21%), Uterine growth restriction (15%), Antepartun Hemorage (28%), UTis (35%), premature raptures of membranes (18%), preterm labor (34%), Normal delivery (69%), ceasarean delivery (31%), Oligohydramnios (6%), Polyhydramnios (16%), stillbirths (1%) and Miscarriage (2%) (Table 1 and Figure 1).

Figure 1: Indicates maternal complications in GDM.
Table 1: Maternal outcomes in GDM.
| Complications | Percentage of patient frequency |
|---|---|
| Hypertension | 32 |
| Preeclampsia | 21 |
| Uterine growth restriction | 15 |
| Antepartun Hemorage | 28 |
| UTis | 35 |
| Premature raptures of membranes | 18 |
| Preterm Labour | 34 |
| Oligohydramnios | 6 |
| Polyhydramnios | 16 |
| Miscarriage | 2 |
| Stillbirths | 1 |
Table 2 and Figure 2 indicates fetal complications of Macrosomia (21%), Hypoglycemic neonates (5 %), Hypocalcemic neonates (1%), Phototherapy required (12%), Neonates with RDS (3 %), Birth trauma (29%), Jaundice (12%) and Congenital anomalies (6%). Table 3 and Figure - 3 showing Vaginal delivery (69%), ceasarean delivery (31%).
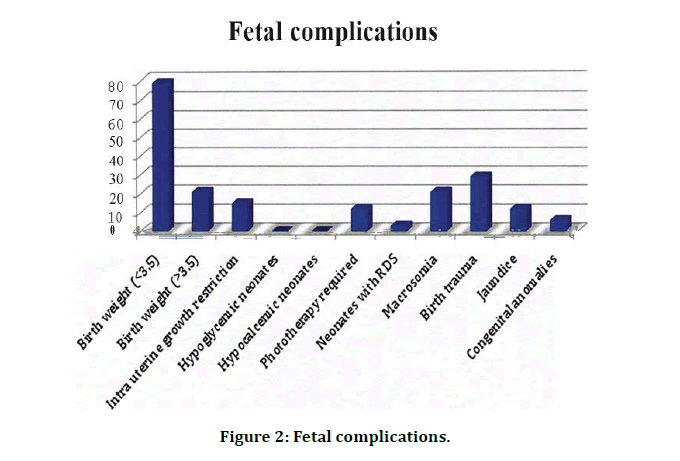
Figure 2: Fetal complications.
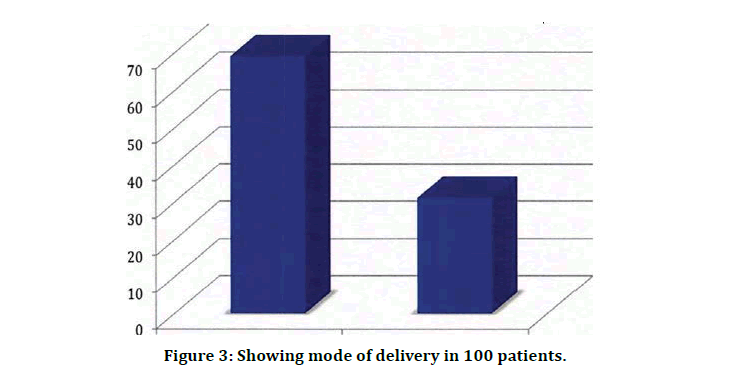
Figure 3: Showing mode of delivery in 100 patients.
Table 2: Fetal outcomes in GDM.
| Complications | Percentage of frequency |
|---|---|
| Birth weight (<4) | 79 |
| Birth weight (>4) | 21 |
| Hypoglycemic neonates | 5 |
| Hypocalcemic neonates | 1 |
| Phototherapy required | -12 |
| Neonates with RDS | 3 |
| Macrosomia | 21 |
| Birth trauma | 29 |
| Jaundice | 12 |
| Congenital anomalies | 6 |
Table 3: Showing mode of delivery in 100 patients.
| Vaginal delivery | Caesarean section |
|---|---|
| 69 | 31 |
Several obstetric problems occur 1n diabetic pregnancy, their frequency being causally related to the quality of the diabetic control achieved [1]. In this connection, the present study evaluated the glycemic variability in each trimester. There was significant difference in Glycemic variability when it was compared with between the categories of variability (p < 0.0095).
An increased risk of pregnancy induced hypertension, pre-eclampsia, antepartum hemorrhage, premature rapture of membranes, preterm labors, caesarean sections and Instrumental deliveries. Same kinds of result were obtained in our study, with slight mcrease m numbers. Several studies have demonstrated that macrosomia correlate with glycemic control in pregnancy complicated by diabetes. To prevent fetal hyperglycemia, fetal insulin secretion and fetal growth increase. Cesarean deliveries are common among women with and without GDM and many studies have documented the cesarean delivery is a successful intervention used to decrease complications associated with gestational diabetes. It was reported that women with treated gestational diabetes had low rate of macrosomia, while untreated gestational diabetes had two¬ fold increased risk of cesarean delivery evaluated outcomes of women with increased incidence of cesarean section but no differences in neonatal outcome compared with women with normal OGTT. Contrary to the conclusion by Naylor, et al. [20] that it could be the diagnosis per se that led to intervention. Where as in our study the cesarean delivery was 31%, remaining 69% were normal deliveries and it was achieved by continuous monitoring of glycemic control.
Macrosomia remams an important morbidity because it is associated with increased risk for traumatic birth injury, obesity, and diabetes in later life. Although some of the variation in incidence may be related to definition, most authors agree that macrosomia is in part related to maternal glucose control. The increased proportion of macrosomic infants and morbidity is m accordance with findings already established in a group of women with borderline glucose tolerance. Fetal macrosomia is associated with delivery problems, such as shoulder dystocia and increased risk of cesarean section. According to that, the incidence of macrosomia is significantly increased in this study.
The outcome among GDM women diagnosed with diabetes is shown as a reference for obstetrical practice when GDM was diagnosed. Those women with diabetes are all treated, and the outcome despite that was quite like the outcome of other studies. The outcome in the diabetes group could be due to either difficulties to influence the outcome by treatment, or the fact that treatment could have stopped the increased complications noted in this study with greater deterioration in glucose tolerance. This underlines the need for randomized studies of the effects of treatment in women.
First trimester diagnosed, 100 GDM patients were recruited over a period of 18 months. Systematic clinical and laboratory diagnostic test included fasting, postprandial blood glucose, HbA1c levels, two-hour oral glucose challenge test and six point profile test analysis for all GDM cases. Glycemic variability was calculated by standard deviation of fasting, postprandial blood glucose and six-point profile test. Percentages of maternal and fetal outcome were calculated. Minimum, median, and maximum age was 18, 27 and 36 years respectively. Half of the subjects were above 25 years (51%). 89% were educated up to pnmary level and, 69%, 23% and 8% belonged to low, middle and upper socioeconomic status respectively. The percentages of mild, moderate, high and extreme high variability were 42%, 31%, 18% and 9% respectively, by comparison of standard deviation of individual's each trimester blood glucose level. The percentages of mild, moderate, high and extreme high were 51%, 28%, 13% a1. 8% respectively, based on six-point profile test.
There was significant difference in Glycemic variability when it was compared with between the categories of variability. GDM women were more prone to pregnancy induced hypertension (32%), preeclampsia (21%), Uterine growth restriction (15%), Antepartum Hemorage (28%), UTis (35%), premature raptures of membranes (18%), preterm labor (34%), Normal delivery (69%), ceasarean delivery (31%), Oligohydramnios (6%), Polyhydramnios (16%), stillbirths (1%) and Miscarriage (2%). Fetal complications of Macrosomia (21%), Hypoglycemic neonates (5%), Hypoglycemic neonates (1%), Phototherapy required (12%), Neonates with RDS (3%), Birth trauma (29%), Jaundice (12%) and Congenital anomalies (6%) [21-23].
Conclusion
In conclusion, glycemic variability is one of the components of glycemic disorders in patients with diabetes. Soon, the use of CGMS will need to be increased to promote better assessment and management of glycemic variability in both type 1 and type 2 diabetes.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Gillmer MDG, Hurley PA. Diabetes and endocrine disorders in pregnancy. In: Edmonds DK, editor. Dewh urst ' s Textbook of obstetrics and gynaecology for postgraduates. 6th Edn. Oxford: Blackwell Science 1999; 197-209.
- Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med 2000; 342:1500-1507.
- Goldenberg RL, Tamura T. Pre pregnancy weight and pregnancy outcome. JAMA 1996; 275:1127-1128.
- HAPO Study Cooperative Research Group: The hyperglycemia and adverse pregnancy outcome (HAPO) Study. Intl J Gyn Obstr 2002; 78:69-77.
- Hillier TA, Pedula KL, Schmidt MM, et al. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care 2007; 30:2287-2292.
- Homko CJ, Sivan E, Reece EA, et al. Fuel metabolism during pregnancy. Semin Reprod Endocrinol 1999; 7:119-125.
- Hong JU, Rumbold AR, Wilson KJ, et al. Borderline gestational diabetes mellitus and pregnancy outcomes. BMC Pregnancy Childbirth 2008; 8:31.
- Horváth EM, Benkő R, Kiss L, et al. Rapid ‘glycaemic swings’ induce nitrosative stress, activate poly (ADP-ribose) polymerase and impair endothelial function in a rat model of diabetes mellitus. Diabetologia 2009; 52:952-961.
- International Diabetes Federation. Guideline for management of postmeal glucose. Brussels: IDF 2007; 1-27.
- Jarrett RL. Glucose tolerance and complications of pregnancy m nondiabetic women. N Engl J Med 1987; 316:1344.
- Jensen DM, Damm P, Sorensen B, et al. Clinical impact of mild carbohydrate intolerance in pregnancy: A study of 2904 nondiabetic Danish women with risk factors for gestational diabetes mellitus. Am J Obstet Gynecol 2001; 185:413-419.
- Johns K, Olynik C, Mase R, et al. Gestational diabetes mellitus outcome in 394 patients. J Obstet Gynaecol Can 2006; 28:122-7.
- Jones SC, Saunders HJ, Qi W, et al. Intermittent high glucose enhances cell growth and collagen synthesis in cultured human tubulointerstitial cells. Diabetologia 1999; 42.
- Jovanovich-Peterson L. Medical management of pregnancy complicated by dia betes. Alexandria VA: American Diabetes Association, 1993.
- Jovanovic-Peterson L, Peterson CM. Nutritional management of the obese pregnant women. Nutri 1991; 17:1.
- Jovanovic-Peterson L, Peterson CM, Reed GF , et al. Maternal postprandial glucose le vels and infant birth weight : The diabetes in early pregnancy study. Am J Obstet Gynecol 1991; 164:103-111.
- Perveen N, Saeed M. Gestational diabetes, and pregnancy outcome: Experience at shaikh zayed hospital. Mother and Child 1996; 34:83-8.
- Gillmer MDG, Hurley PA. Diabetes and endocrine disorders in pregnancy. In: Edmonds DK, editor. Dewhurst's Textbook of obstetrics and gynaecology for postgraduates. 6th Ed. Oxford: Blackwell Science 1999; 197-209.
- Kilpatrick ES, Rigby AS, Atkin SL. Mean blood glucose compared with HbA 1c m the prediction of cardiovascular disease m patients with type 1 diabetes. Diabetologia 2008; 51:365-371.
- Naylor CD, Sermer M, Chen E, et al. Cesarean delivery in relation to birth weight and gestational glucose tolerance: Pathophysiology or practice style ronto tri hospital gestational diabetes investigators. JAMA 1996; 75:1165-1170.
- Conway D, Langer 0. Elective delivery of infants with macrosomia in diabetic women: Reduced shoulder dystocia versus increased cesarean delivery. Am J Ob stet Gynecol 1998; 178:922-925.
- Aberg A, Rydhstroem H, Frid A. Impaired glucose tolerance associated with adverse pregnancy outcome: a population-based study in southern Swed en . Am J Obstet Gynecol 2001; 184:77-83.
- Jensen DM, Damm P, Sorensen B, et al. Clinical impact of mild carbohydrate intolerance in pregnancy: A stud y of 2904 nondiabetic Danish women with risk factors for gestational diabetes mellitus. Am J Obstet Gynecol 2001; 185:413-419.
Author Info
Abinaya Vijayan, V Kalavathy and K Vani*
Department of Obstetrics and Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Abinaya Vijayan, V Kalavathy, K Vani, Study on Maternal Complications and Outcomes in GDM to Identify Neonatal Morbidity in Gestational Diabetes Mellitus Patients, J Res Med Dent Sci, 2021, 9 (5):181-187.
Received: 22-Apr-2021 Accepted: 20-May-2021 Published: 31-May-2021
