Research - (2022) Volume 10, Issue 8
Study Protocol: Evaluation of Echocardiography in Sick Neonates in Neonatal Intensive Care Unit (NICU)
Kushal Desai*, Amar Taksande, Revat Meshram, Amol Lohakare and Rajendra Borkar
*Correspondence: Kushal Desai, Department of Pediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed University), India, Email:
Abstract
Background: Echocardiography plays an increasing role in NICU’s, and neonatologists increasingly use it to make clinical decisions. It is the utilization of cardiac ultrasound at the bedside to assess longitudinal changes in both functional and hemodynamic parameters. Information that reflects cardiac capacity and systemic and pulmonary blood flow in preterm and term neonates can be observed. Analyzing hemodynamics via echocardiography at the bedside can be considered an addition to the clinical examination to assess cardiac function in sick neonates. Our primary goal in this study is to determine whether sick neonates have heart structural or functional abnormalities via echocardiography. Objectives: To determine the correlation between echocardiographic indications and intervention in sick newborns. Material & Methods: This prospective cross-sectional study will be conducted in the Neonatology Department, JNMC, Sawangi, Wardha. Each sick newborn will be asked for demographic information, including age, gender, and gestational age (GA), and birth weight. All sick neonates admitted to NICU will be selected as per the inclusion criteria in a non-randomized manner and will be subjected to echocardiography. If echocardiography reveals any abnormal findings, they will be followed up for any sequelae. The indications for echocardiography, the echocardiographic results and any changes in clinical management will be decided. Result: After completing the study, we will know the indication of echocardiography in sick neonates. We will come to see the prevalence of prevalence of cardiac structural or functional abnormality in sick neonates. Conclusion: This study will provide a cardiac structural or functional abnormality in the sick newborns.
Keywords
Cardiac function, Sick newborn, Echocardiography, Neonatology
Introduction
A late diagnosis of critical congenital heart disease (CCHD) can lead to cardiac failure, cardiovascular collapse, and increased mortality rate if not diagnosed early. CCHD in the newborn may have low SpO2 unrecognized clinically. Over the past decade, the role of echocardiography in neonatal intensive care units (NICU’s) has changed. Neonatologists are adopting echocardiography more and more to diagnose sick newborns, and its use in neonatal intensive care units is growing quickly. Functional echocardiography uses cardiac ultrasonography at the bedside to track longitudinal functional and hemodynamic changes. In preterm and term neonates, information that measures cardiovascular capability and systemic and pulmonary blood flow can be seen. In critically ill infants, echocardiography provides direct assessment of hemodynamics at the bedside and can be considered an extension of the clinical examination to assess cardiovascular well-being [1,2]. The physiological information may target specific interventions based on the underlying pathophysiology. Echocardiography is utilized in neonatal critical care units to identify pericardial effusion, cardiac tamponade, patent ductus arteriosus, pulmonary hypertension, hemodynamic evaluation, and patent ductus arteriosus [3,4]. When making a differential diagnosis for a newborn who displays cyanosis, cardio respiratory distress, and a shock like appearance, the neonatologist must take congenital heart disease, other causes of heart disease like myocarditis, and pulmonary, central nervous system, hematologic, infectious, and metabolic diseases into account.. Congenital heart disease patients may not always be recognized in the first few days of life by physical examination, electrocardiogram, and chest X-ray data. Contrarily, because echocardiography visualizes the anatomy of the heart, it can provide the information needed to quickly separate the majority of patients with significant congenital heart disease from the others.. In patients with pericardial effusion, cardiac tamponade, and cardiac anomalies such congenital heart defects or valve issues, echocardiography is the gold standard diagnostic procedure to assess hemodynamic stability [4-6]. Echocardiographic findings can be diagnostic in some cardiac defects [5-7]. In a rural setting, use of echocardiography and its use in sick neonates in nicu is not well studied.
Research question
Do sick neonates in NICU have cardiac structural or functional abnormalities?
Our hypothesis
Our hypothesis is that sick neonates have cardiac abnormalities which correlate with the neonatal outcome.
Aim
To find out the prevalence of cardiac structural or functional abnormality in sick neonates by echocardiography.
Objectives
To know the association between echocardiography indications and intervention.
To know the association between echocardiography indication and neonatal outcome.
To find out the correlation of cardiac abnormality with neonatal outcome.
Materials and Methods
Study setting
This study will be conducted in the Neonatology unit, “Department of Pediatrics, in Jawaharlal Nehru Medical College & AVBR Hospital, Sawangi, Wardha”.
Sources of data
Study members: All members in this study will be critically ill sick neonates who will be admitted to the NICU. All sick neonates admitted to NICU will be selected as per the inclusion criteria in a non-randomized manner and will be subjected to echocardiography on selected days. If echocardiography reveals any abnormal findings, they will be followed up for any sequelae.
Follow-up echocardiography will be done in the case of the presence of any findings. Morphology of conclusions will be studied and recorded, and clinical correlation with various findings on echocardiography will be done. Neonates will be followed till recovery and discharge from NICU. Information about all echocardiograms performed on the neonatal unit will be collected prospectively. Indications for echocardiography, echocardiographic findings, and any changes in clinical management will be determined.
Inclusion criteria
Sick neonates in NICU.
Written informed consent given by the parents.
Exclusion criteria
Full term healthy neonates maintaining oxygen saturation.
Neonates in NICU with hyperbilirubinemia only for phototherapy.
Newborns after exchange transfusion.
Congenital malformation.
Study design
Cross-sectional study.
Time frame/duration
3 years.
Study flow chart (Figure 1)
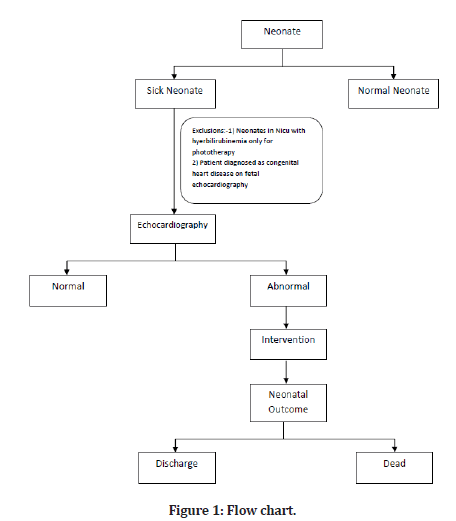
Figure 1: Flow chart.
Methodology
A detailed information sheet will be given to the newborn parents in which the methodology of treatment will explain in their local language. Due permission of the ethics committee of the institute will be taken before starting the study.
Assessments
Demographic information will be collected for all sick neonates (study cases), including age, gender, gestational age(GA), and birth weight. For all study cases, perinatal history and clinical examination were made. Laboratory examinations will be included a complete blood picture, blood grouping, and a peripheral smear(ps) test will also be done in all study cases.
Definition of Sick Neonates includes high-risk neonates with any of the following: Neonatal convulsions, birth asphyxia and hypoxic-ischemic encephalopathy(HIE), respiratory distress, neonatal sepsis, preterm neonates, neonates born out of traumatic/instrumental labour, metabolic disturbances with convulsions, congenital malformation of the central nervous system, and neural tube defects.
Factors identifying the neonate as a “sick neonate” will be assessed by taking detailed maternal history and looking into perinatal and antenatal records.
All sick neonates admitted to NICU will be selected as per the inclusion criteria in a non-randomized manner and will be subjected to echocardiography on selected days. If echocardiography reveals any abnormal findings, they will be followed up for any sequelae.
Follow-up echocardiography will be done in the case of the presence of any findings. Morphology of conclusions will be studied and recorded, and clinical correlation with various findings on echocardiography will be done. Neonates will be followed till recovery and discharge from NICU. Information about all echocardiograms performed on the neonatal unit will be collected prospectively. Indications for echocardiography, echocardiographic findings, and any changes in clinical management will be determined.
Echocardiography examination
We will be used M-mode and 2D-Echo to measure the LV diameter during systole and diastole and also to measures the thickness of IVS during diastole and also thickness of LV posterior wall. The fractional shortening and ejection fraction will be measured by the m-mode and simpson methods. All echocardiographic data will be taken as per American Society of Echocardiography [8,9].
Variables
We will do the following important variable.
Cause of sick neonates.
Gestational age.
Birth weight.
Intervention (Medical or Surgical).
Congenital heart disease.
M Mode (FS & EF for the systolic function of the heart).
Pulse-Doppler (Diastolic function of the ventricle).
Sample size calculation is mentioned in Table 1.
| Population size(for finite population correction factor or fpc)(N) | 10000 |
| Hypothesized % frequency of outcome factor in the population (p) | 8%+/-5 |
| Confidence limits as % of 100(absolute +/- %)(d) | 5% |
| Design effect (for cluster surveys-DEFF) | 1 |
| Confidence level (%) | 95% |
| Sample size Required | 114 |
| Formula used for calculation of Sample size | n = [DEFF*Np(1-p)]/ [(d2/Z21-α/2*(N-1)+p*(1-p)] |
Table 1: Sample size calculation.
Statistical analysis
Data will be entered into Microsoft Excel sheet and statistical analysis will be done on statistical software STATA 12. For descriptive statistics, mean standard deviation will be used, median and interquartile range for quantitative variables, and percentage with number for categories. Relationship of various demographic, clinical characteristics and echocardiography diagnosis with outcome will be evaluated employing Chi-square test, Fischer’s exact test for categorical data and independent t test for continuous data with normal distribution. Spearman (parametric) or Pearson (non-parametric) correlations will be applied to determine the association between dependent and independent variables. P value will be considered significant if less than 0.05.
Expected Result
After completion of the study we will come to know the indication of the echocardiography in sick neonates. We will come to know the prevalence of prevalence of cardiac structural or functional abnormality in sick neonates. To find out the correlation of cardiac abnormality with neonatal outcome. We will come to know that in how many cases this investigation will changed the clinical management and neonatal outcome.
Discussion
Congenital heart defects (CHD) is one of the main cause of infant deaths in developed world. A early diagnosis of CHD was associated with a better preoperative condition. Echocardiography is being used progressively in the neonatal intensive care unit and has been proven to have high return of various cardiovascular abnormalities. Echocardiography has made the neonatologist able in providing better care to the neonate with various cardiac abnormalities like patent ductus arteriosus, neonate in shock, neonate with cyanosis with or without pulmonary hypertension, or an infant with heart murmur [9,10]. An echocardiogram in the neonatal intensive care unit is used in sick neonates to diagnose or exclude suspected congenital heart disease and assess cardiovascular function. To find the underlying case in cases of a neonate in shock, there is no better modality than echocardiography. Echocardiography can also diagnose all the causes of circulatory shock like myocardial dysfunction, hypertrophic cardiomyopathy or a sizeable duct [11,12]. Brown, et al. [11] reported that 25% of infants with CCHD were missed to be diagnosed with heart disease until after discharge from the nursery. Out of this missed cases, some children presented as critically severe and could not be saved even until some surgical intervention could be done. CCHDs are structural heart defects often associated with hypoxia among infants during the newborn period. Due to closure of ductus arteriosus in neonatal period, patients with congenital heart disease have greater morbidity and mortality early in life. Certain physiological changes in neonatal period also add up to the increased risk of morbidity and mortality in neonatal period. Kadivar M et al. performed a retrospective study on ill infants to assess the impact of echocardiographic testing on clinical care (10). Asymptomatic murmurs (45 percent) and extracardiac anomalies/dysmorphic features (45 percent) were the two most frequent clinical reasons for an echocardiography (24 percent). The echocardiographic findings included congenital structural abnormalities (33%) thermodynamically significant patent arterial duct (3%) chronic neonatal pulmonary hypertension (6%) and left ventricular dysfunction (3%). Moss, et al. [13] carried out another study on the evaluation of echocardiography in the neonatal unit. By using echocardiography, he reported finding 17 children with a minor defect and 44 infants with a structural cardiac problem. In 64 (78%) infants, echocardiography led to a specific modification in clinical care.. In their study, Du, et al. [14] found that only 16 percent of neonatal heart murmurs were caused by benign conditions, with 84 percent being caused by heart disorders. The cardiac murmur (22 instances) and cyanosis were listed as the primary indicators of an echocardiography by Chioukh, et al. [15]. (6 patients). Either a chromosomal aberration or a link to a deformity has been identified in 36% of cases. A different study by Arshad, et al. [16] evaluating the cardiac health of newborns found that 1523 (55.8%) of them had structurally and functionally normal hearts, while 866 (31.7%) had congenital heart disease, 69 (2.5%) had duct dependent lesions, 248 (9.1%) had persistent pulmonary hypertension, and 23 (0.8%) had left ventricular (LV) dysfunction despite having structurally normal hearts. Khamkar, et al. [16] prospective observational study of newborns in a tertiary Neonatal Intensive Care Unit (NICU) in Pune, India, revealed that hemodynamic instability (n=43, 12.36 percent) and patent ductus arteriosus (n=174, 50 percent) were the two most common indications for functional echocardiography (FnECHO). They stated that the FnECHO results led to additional therapy modifications or avoided unnecessary intervention in 148 cases (42.50 percent). Maliheh Kadivar, et al. [17] retrospective study (10) revealed that echocardiography altered the clinical care in at least 66 percent of neonates scanned, including emergency surgical intervention for 7%, medical treatment for 22%, and routine cardiologic follow-up for 37% of patients. Arjmandnia, et al. [18] retrospective study recommended that, in addition to the previous inclusion criteria of the neonates admitted to NICU requiring echocardiography, including prolonged respiratory distress murmurs and rales, cardiac causes be more carefully taken into account in term and nearterm newborns with respiratory distress. The results of this study will be shared through publication in prestigious peer-reviewed publications and presentation at conferences across the world.
Outcome Mesures
The primary outcomes will be a to assess the cardiac structural or functional abnormalities of sick neonates in NICU.
The secondary outcome will be to know the association between echocardiography indications and intervention (Medical or surgical) and the relationship between echocardiography indication and neonatal outcome.
Scope Of The Study
Echocardiography is widely used for diagnosing cardiac structural or functional abnormalities as it is a noninvasive, readily available investigation.
Minimal data on echocardiography utility in sick neonates in the NICU at the rural hospital.
Heart murmur in neonates could be a symptom of CHD, and timely echocardiography is essential in diagnosing the type of disease.
Limitation
Area of coverage will be single center study.
Implication
After completing the study, we will know the percentage of changes in the management of the newborns after the echocardiography scan. Also, after echocardiography, we will get an idea of the neonatal outcomes of the sick newborn in the intensive care unit.
Acknowledgements
The authors would like to acknowledge the support from staff of the Neonatology Department, JNMC, AVBRH, Sawangi Meghe, Wardha, India.
Author's Contributions
Conceptualization and writing of the original draft: AT and KD; Review and editing: AT and KD. All authors have read and approved the final version of the manuscript.
Source of Funding
None.
References
- Tissot C, Singh Y. Neonatal functional echocardiography. Curr Opin Pediatr 2020; 32:235-244.
- Meberg A, Otterstad JE, Frøland G, et al. Early clinical screening of neonates for congenital heart defects: The cases we miss. Cardiol Young 1999; 9:169-174.
- Singh Y, Katheria A, Tissot C. Functional echocardiography in the neonatal intensive care unit. Indian Pediatr 2018; 55:417-424.
- Bakr AF, Habib HS. Combining pulse oximetry and clinical examination in screening for congenital heart disease. Pediatr Cardiol 2005; 26:832–835.
- Koppel RI, Druschel CM, Carter T, et al. Effectiveness of pulse oximetry screening for congenital heart disease in asymptomatic newborns. Pediatr 2003; 111:451–455.
- Thangaratinam S, Daniels J, Ewer AK, et al. Accuracy of pulse oximetry in screening for congenital heart disease in asymptomatic newborns: a systematic review. Arch Dis Child Fetal Neonatal Ed 2007; 92:176-180.
- Singh Y. Echocardiographic evaluation of hemodynamics in neonates and children. Front Pediatr 2017; 5:201.
- Lopez L, Colan SD, Frommelt PC, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: A report from the pediatric measurements writing group of the American society of echocardiography pediatric and congenital heart disease council. J Am Society Echocardiography 2010; 23:465–495.
- Cui W, Roberson DA. Left ventricular Tei index in children: Comparison of tissue dopplerimaging, pulsed wave doppler, and m-mode echocardiography normal values. J Am Society Echocardiography 2006; 19:1438–1445.
- Kadivar M, Kiani A, Kocharian A, et al. Echocardiography and management of sick neonates in the intensive care unit. Congenit Heart Dis 2008; 3:325-329.
- Brown KL, Ridout DA, Hoskote A, et al. Delayed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart 2006; 92:1298 –1302.
- Moss S, Kitchiner DJ, Yoxall CW, et al. Evaluation of echocardiography on the neonatal unit. Arch Dis Child Fetal Neonatal Ed 2003; 88:287-291.
- Moss S, Kitchiner DJ, Yoxall CW, et al. Evaluation of echocardiography on the neonatal unit. Arch Dis Child Fetal Neonatal 2003; 88.
- Du ZD, Roguin N, Barak M. Clinical and echocardiographic evaluation of neonates with heart mumurs. Acta Paediatr. 1997;86(7):752–6.
- Chioukh FZ, Khemis T, Bahri J, et al. Neonatalogist-performed echography in neonatology: A Tunisian experience. Tunis Med 2019; 97:122-127.
- Arshad MS, Shakir W, Haq HMA, et al. Cardiac evaluation in newborns: An echocardiography based study. Pakistan Heart J 2021; 54:25-29.
- Khamkar AM, Suryawanshi PB, Maheshwari R, et al. Functional Neonatal Echocardiography: Indian experience. J Clin Diagn Res 2015; 9:SC11-4.
- Arjmandnia MH, Sadeghi-Moghaddam P, Habibollahi A, et al. Necessity of echocardiography in evaluation of neonates with respiratory distress admitted in NICU. J Jahrom Univ Med Sci 2016; 14:39-44.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Kushal Desai*, Amar Taksande, Revat Meshram, Amol Lohakare and Rajendra Borkar
Department of Pediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed University), IndiaCitation: Kushal Desai, Amar Taksande, Revat Meshram, Amol Lohakare, Rajendra Borkar, Study Protocol: Evaluation of Echocardiography in Sick Neonates in Neonatal Intensive Care Unit (NICU), J Res Med Dent Sci, 2022, 10 (8): 110-114.
Received: 06-Jul-2022, Manuscript No. jrmds-22-68701; , Pre QC No. jrmds-22-68701(PQ); Editor assigned: 08-Jul-2022, Pre QC No. jrmds-22-68701(PQ); Reviewed: 23-Jul-2022, QC No. jrmds-22-68701; Revised: 28-Jul-2022, Manuscript No. jrmds-22-68701 (R); Published: 04-Aug-2022
