Research Article - (2021) Volume 9, Issue 12
Study to Compare the Caregiver Burden of Schizophrenia and Bipolar Disorder
*Correspondence: S.Nambi, Department of Psychiatry, Sree Balaji Medical College and Hospital, Chennai-600044, Tamil Nadu, India, Email:
Abstract
Schizophrenia is a severe and disabling mental disorder characterised by fundamental distortions in thinking and perception and by inappropriate emotion and behavior. Bipolar disorder is a severe mental illness with a chronic course, fluctuating levels of severity and a complete inter episodic remission. Persons suffering from bipolar disorder experience extreme shiftsinmood,energyandactivitylevels.Toassess&comparetheburden,qualityoflifeanddepressionin caregivers of persons suffering from schizophrenia and bipolar disorder. It is a comparative study, total sample size is 100. Fifty person’s suffering from schizophrenia and fifty persons suffering from bipolar disorder and their caregivers attending the psychiatric outpatient dept. of SBMCH fulfilling the study criteria and gave informed consent were included in the study. Inclusion criteria, age between 18 and 60 years & diagnosis of schizophrenia or bipolar disorder as per ICD 10 DCR. Exclusion criteria, Presence of comorbid physical illness including neurological illness & Presence of any substance abuse/dependence except that of tobacco. Caregiver burden: The caregiver burden was found to be significantly higher among the caregivers of persons suffering from schizophrenia, with a mean normalized BAS score of 64.25 against a score of 57.92 for bipolar subjects. The study showed that though the burden of care of bipolar disorder is less when compared to schizophemia, it cannot be neglected. To conclude the study showed that though the burden of care of bipolar disorder is less when compared to schizophemia, it cannot be neglected.Keywords
Schizophrenia, Depression, Bipolar disorder, Substance abuse/Dependence, Caregivers, mentally ill, psychiatric illnessIntroduction
Schizophrenia is a chronic and severe mental disorder affecting 20 million people worldwide. Schizophrenia is characterized by distortions in thinking, perception, emotions, language, sense of self and behavior. Common experiences include hallucinations (hearing voices or seeing things that are not there) and delusions (fixed, false beliefs).People with schizophrenia are 2-3 times more likely to die early than the general population (2). This is often due to preventable physical diseases, such as cardiovascular disease, metabolic disease and infections. Stigma, discrimination and violation of human rights of people with schizophrenia is common. Schizophrenia is treatable. Treatment with medicines and psychosocial support is effective.
WHO’s Mental Health Action Plan 2013-2020, endorsed by the World Health Assembly in 2013, highlights the steps required to provide appropriate services for people with mental disorders including schizophrenia. A key recommendation of the Action Plan is to shift services from institutions to the community.
A person with bipolar disorder will experience changes in mood, energy, and activity levels that can make day-to-day living difficult. Bipolar disorder can cause severe disruption to a person’s life, but the impact varies between individuals. With appropriate treatment and support, many people with this condition live a full and productive life. According to the National Alliance on Mental Illness (NAMI), bipolar disorder affects over 10 million people in the United States or around 2.8% of the population. On average, a person will receive a diagnosis around the age of 25 years, but symptoms can appear during the teenage years or later in life. It affects males and females equally.
The National Institute of Mental Health describe the main symptoms of bipolar disorder as alternating episodes of high and low mood. Changes in energy levels, sleep patterns, ability to focus, and other features can dramatically impact a person’s behavior, work, relationships, and other aspects of life. Most people experience mood changes at some time, but those related to bipolar disorder are more intense than regular mood changes, and other symptoms can occur. Some people experience psychosis, which can include delusions, hallucinations, and paranoia.
Between episodes, the person’s mood may be stable for months or years, especially if they are following a treatment plan. Treatment enables many people with bipolar disorder to work, study, and live a full and productive life. However, when treatment helps a person feel better, they may stop taking their medication. Then, the symptoms can return. Some aspects of bipolar disorder can make a person feel good. During an elevated mood, they may find they are more sociable, talkative, and creative. However, an elevated mood is unlikely to persist. Even if it does, it may be hard to sustain attention or follow through with plans. This can make it difficult to follow a project through to the end. Aim of the study is to assess & compare the burden, quality of life and depression in caregivers of persons suffering from schizophrenia and bipolar disorder.
Material and methodsDried this study was conducted after getting ethical clearance from the University ethical committee. It is a comparative study, total sample size is 100 who satisfied the inclusion criteria, suffering from bipolar disorder and their caregivers attending the psychiatric outpatient dept. of SBMCH and gave informed consent to be included in the study.
Inclusion criteriaAge group 18 to 50 years with age, sex and socio demographic matched general population
No current or past history of Obsessive Compulsive Disorder.
Exclusion criteriaPresent and Past history of Schizophrenia, Bipolar affective disorder, Psychosis, Recurrent.
Substance abuse other than nicotine
Depressive Disorder. (Table 1, Figure 1)(Table 2, Figure 2)
| Parameter | Attributes | Schizophrenia | BPAD | Test | Value | d.f. | Sig. |
|---|---|---|---|---|---|---|---|
| Gender | Male | 25 (50%) | 28 (56%) | Chi- Square | 0.361 | 1 | 0.548 |
| Female | 25 (50%) | 22 (44%) | |||||
| Education | Illiterate | 0 (0%) | 2 (4%) | Chi- Square | 6.927 6 | 0.328 | |
| Primary | 5 (10%) | 1(2 %) | |||||
| Middle School | 5 (10%) | 9 (18%) | |||||
| High School | 13 (26%) | 12 (24%) | |||||
| Post High School | 13 (26%) | 12 (24%) | |||||
| Grad./Post Grad. | 14 (28%) | 13 (26%) | |||||
| Professional/Honours | 0 (0%) | I (2%) | |||||
| Occupation | Unemployed | 36(72%) | 25 (50%) | Chi- Square | 16. 2115 | 0.006 | |
| Unskilled Worker | 13 (26%) . 9 ( 18 %) | ||||||
| Semiskilled Worker | 0 (0%) | 3 (6%) | |||||
| Skilled | I (2%) | 7 (14 %) | |||||
| Clerical/Shop owner/Farmer | 0 (0%) | 5 (10%) | |||||
| Semi Professional | 0 (0%) | 1 (2%) | |||||
| Income | < Rs. 1520 | 0 (0%) | 1 (2%) | Chi- Square | 15.2576 | 0.018 | |
| 1521-4555 | 11 (22%) | I (2%) | |||||
| 4556-7593 | 25 (50%) | 24 (48%) | |||||
| 7594-11361 | 10 (20%) | 21 (42%) | |||||
| 11362-15187 | 3 (6%) | 1 (2%) | |||||
| 15188-30374 | 1 (2%) | 1 (2%) | |||||
| > Rs, 30374 | 0 (0%) | 1 (2%) | |||||
| Religion | Hindu | 44 (88%) | 42 (84%) | Chi- Square | 1.247 2 | 0.536 | |
| Muslim | 3 (6%) | 6 (12% | |||||
| Christian | 3 (6%) | 2 (4%) | |||||
| Marital Status | Single | 21 (42 %) | 10 (20%) | Chi- Square | 11.9663 | 0.008 | |
| Married | 25 (50%) | 39 (78%) | |||||
| Separated | 4 (8%) | 0 (0%) | |||||
| Divorced | 0 (0%) | 1 (2%) | |||||
| Family | Nuclear | 37 (74%) | 40 (80%) | Chi- Square | 0.508 1 | 0.476 | |
| Joint | 13 (26%) | 10 (20% | |||||
| Age | Mean± SD | 34.72 ± 9,.69 | 37.54 ± 11.47 | t-test | -1.328 | 98 | 0.187 |
| Duration of illness | Mean± SD | 10.02 ± 8.05 | 10.40± | t-test | -0.243 | 98 | 0.808 |
| 7.56 | |||||||
Table 1: Comparison of sickled RBC in anti-sickling analysis of two methods with pre-treatment (n=49)
Figure 1: Income of the Family.
Figure 2: Gender of the Caregivers.
| Items | Mann-Whitney Test | |
|---|---|---|
| Z-Value | Sig. | |
| Current financial position adequate | -0.905 | 0.365 |
| Largely responsible for patient | -0.465 | 0.642 |
| Future financial position worries | -3.072 | 0.002 |
| Financial position worsened | -2.054 | 0.04 |
| Illness of patient prevents my work | -0.818 | 0.413 |
| Forced to go for work to support | 0 | 1 |
| Affects Efficiency | -1.047 | 0.295 |
| Patient looks after himself | -2.607 | 0.009 |
| Responsible for patients all needs | -2.482 | 0.013 |
| Compensate patients shortcomings | -1.653 | 0.098 |
| Family support helps to care patient | -2.581 | 0.01 |
| Patient causes disturbances | -0.866 | 0.386 |
| Able to care for others | -2.513 | 0.012 |
| Family stability disturbed | -1.913 | 0.056 |
| Family appreciates my handling | -1.625 | 0.104 |
| Illness affects relationship | -0.422 | 0.673 |
| Spouse helpswithfamily responsibility | -4.048 | 0 |
| Spouse satisfies sexual needs | -2.796 | 0.005 |
| Spouse still affectionate | -1.184 | 0.237 |
| Quality of mental relationship declined | -2.679 | 0.007 |
| Tired and exhausted | -0.019 | 0.985 |
| Workload increased | -1.628 | 0.104 |
| Health has been affected | -0.788 | 0.431 |
| Have time to look after health | -3.34 | 0.001 |
| Able to relax during the day | -1.249 | 0.212 |
| Sometimes feel depressed | -2.023 | 0.043 |
| Sometimes feel there is no solution | -2.334 | 0.02 |
| Feels like temporary separation | -0.971 | 0.331 |
| Reduce time with patient helps | -3.278 | 0.001 |
| Unpredictable behaviour disturbs me | -0.423 | 0.673 |
| Sleep got affected | -0.434 | 0.665 |
| Illness prevents satisfying relationship with friends | -2.083 | 0.037 |
| Started feeling lonely and isolated | -2.561 | 0.01 |
| Friends' support helps to care patient | -0.243 | 0.808 |
| Sharing helps to feel better | -0.682 | 0.495 |
| Friend s appreciate my way of handling | -1.962 | 0.05 |
| Often frustrated over slow improvement | -3.574 | 0 |
| Feel like doing more than the needs | -3.038 | 0.002 |
| Relatives understand and appreciate | -2.478 | 0.0]3 |
| Satisfied with the assistance of health professional | -3.129 | -3.129 |
Table 2: Family History of Mental Illness.
Results
Caregiver burdenThe caregiver burden was found to be significantly higher among the caregivers of persons suffering from schizophrenia, with a mean normalized BAS score of 64.25 against a score of 57.92 for bipolar subjects.
| Schizophrenia | BPAD | Independent Samples t-test | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t-Value | Sig. | |
| Normalized BAS Score | 64.25 | 8.2 | 57.92 | 9.6 | 3.542 | 0.001 |
| QOL Physical | 61.22 | 14.15 | 68.42 | 12.98 | -2.652 | 0.009 |
| QOL Psychological | 61.74 | 10.4 | 64.52 | 10.75 | -1.315 | 0.192 |
| QOL Social | 55.78 | 13.21 | 62.48 | 11.29 | -2.727 · | 0.008 |
| QOL Environment | 60.94 | 10 .08 | 62.96 | 10.35 | -0.989 | 0.325 |
| MADRS Score | 9.88 | 7.68 | 7.52 | 6.63 | 1.645 | 0.103 |
| GAF Score | 40.2 | 10.97 | 45.6 | 11.1 | -2.447 | 0.016 |
Table3: Burden, quality of life and depression in caregivers.
Figure 3: Magnitude of caregiver burden.
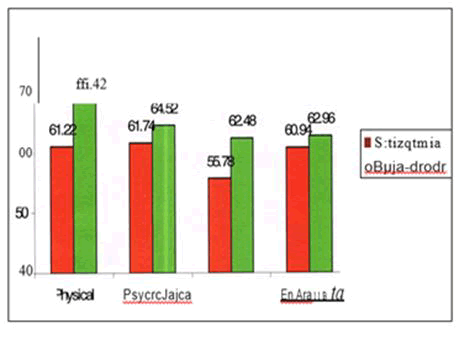
Figure 4: Quality of life of caregivers.
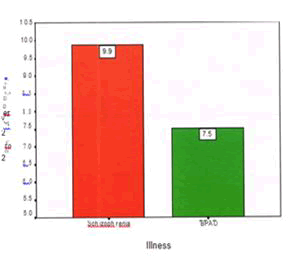
Figure 5: Depression in caregivers.
Discussion
The result of the current study gave a comparison between the burden of care of schizophrenia and bipolar disorder and QOL and depression among the caregivers of persons suffering from these disorders. Socio demographic profile of the person suffering from illness. The mean _age of subjects in schizophrenia and bipolar disorder was comparable with the mean age being 34.72 years (S.D. 9.69) and 37.0 years respectively.
With regards to the marital status 78% of the bipolar subjects were married, 20% were single and only 2% were either divorced/separated. The higher rates of marriage and lower rates of divorce/separation can well be explained on the basis of south Asian ethos and reality in general and specifically in relationship to mental illnesses, wherein marriage is a social norm and divorce is not very common.
In contrast, the schizophrenia subjects were less likely to be married as compared to bipolar subjects. Only 50% of persons suffering from schizophrenia were married. This could be partially attributed to the impact of the schizophrenia illness on the ability of the subjects to enter marital relationships.
Most of the subjects in bipolar disorder and all of the subjects m schizophrenia groups were literate. Only 4%of bipolar disorder subjects were illiterate. 28% of schizophrenia and bipolar disorder. Subjects had received at least a degree. This may reflect the recent trend towards literacy and increasing education attainment in the general population.
50% of the bipolar disorder subjects were working. This reflects a considerably high level of employment. This can be attributed to ready availability of unskilled work which our subjects, who were predominantly of the lower socio economic status, were willing to do in the milder stages of mania and depression and during remission.
On comparing the two groups with regards to occupation, a significantly more number of schizophrenia subjects were not working (72%) compared to bipolar disorder subjects(50% ). This reflects the severe psychosocial consequences of schizophrenia as well as the fact that bipolar disorder being an episodic illness give the patients greater opportunity to pursue occupation in the periods of remission. Also schizophrenia , especially of longer duration is associated with negative symptoms and decline of social skills which also impact ability to be gainfully employed.
Majority of both bipolar disorder and schizophrenia subjects were from nuclear families. This reflects the prevailing social trend. The nuclear families have lesser number of earning members and caregivers to shoulder the burden. The family income of both groups was similar to majority of subjects having family income less than 11,500 per month (92% m schizophrenia and 94% in bipolar disorder group).
Illness CharacteristicsThe mean duration of illness was 10.02 years in schizophrenia group and 10.40 years in bipolar disorder group. Thus the relatively higher duration of illness in our study subjects as compared to Roychaudhuri et al could be due to SBMCH being a tertiary institute receiving a significant number of chronic patients who are likely to have received treatment with other psychiatric and non-psychiatric set ups and who had not responded adequately.
Socio Demographic Profile of the CaregiversThe mean age of caregivers was 49.70±11.61 years in schizophrenia group and 41.94±10.36. Years in bipolar disorder group. This corresponds to other studies by researchers like Chakrabarthi et al in 19952 where the mean age of caregivers of subjects with affective disorders was 39.77years±13.0l.The difference may be explained by the more number of caregivers being parents for the schizophrenia group.
The majority of caregivers in both the groups were females- 56%in schizophrenia and 60% in bipolar disorder group. This is similar to the findings of largely female care givers, in other studies by Chakrabarti et al (1995)2, Perlick et al (1999)59, Dore and Romans (2001) 82 where females were caregivers in 50%, 66 %and 61% cases respectively. 48% of caregivers of schizophrenia subjects and 62% of caregivers of bipolar disorder were employed.
Regarding the relationship of caregivers with the subjects, the bipolar disorder group had greater number spouse as caregivers, while schizophrenia group had greater number of parents as caregivers. 32% of schizophrenia subjects had spouse as the caregivers while for the bipolar disorder subjects it was 66%. This correlates with the finding by Chakrabarti et al where it was 33.3% and 62.8% respectively.
Global Assessment of FunctioningThe mean GAF score for schizophrenia subjects was 40.20 and bipolar disorder subjects was 45.6. This is statistically significant. The number of persons with bipolar disorder who were in remission was only two, among the fifty subject’s studies, which is insignificant.
The severity of illness has a positive correlation with the caregiver burden. This would mean that the actual burden experienced by caregivers of bipolar disorder may be higher if matching for GAF between the two groups was done.
Caregiver BurdenOur study evaluated the burden experienced by the caregivers of persons suffering from two severe mental illnesses-shizophrenia and bipolar disorder, using the Burden Assessment Schedule. The burden of schizophrenia was found to be significantly higher than bipolar disorder with mean normalized BAS scores of 64.25 and 57.92 respectively. This correlates with the results of similar studies by Chakrabarti et ai2, Roychaudhuri et al4 6, Nehra et al39 and Chadda et al72.
It is found that financial difficulties were experienced by caregivers in both the groups without significant differences. This is comparable to the findings by Nehra et al39 But worsening of families finances and worries regarding the patients future financial situation is significantly more with caregivers of schizophrenia. High financial burden in schizophrenia has been established by researchers such as Giel et al13, Moiley et al17 and Saldhana et al19
The caregivers who formed our study group experienced disruption of relations with other _family members and friends, and disruption of family stability. The relationship with friends was significantly affected in schizophrenia. This reflects the findings of early studies by Chakrabarti et al, and Gowtham and Nijhawan 30
Symptoms of depression and anxiety were reported by almost 90% of caregivers of both the groups. But frustration over slow improvement of patient and feelings of isolation and !onliness are more with caregivers of schizophrenia than bipolar disorder. The severe toll on the mental health of caregivers correlates with the findings of researchers such as Rodrigo et al77 and Li Yu Song et al78.
Appreciation for caring is a positive factor which reflects the satisfaction caregivers receive from the appreciation and acknowledgement of their good care from the friends and family members. Caregivers of schizophrenia and bipolar disorder do not significantly differ in this aspect, though a significant number of caregivers reported lack of appreciation, which has been described by Ghadge et al34 as rejection and discrimination in personal and social contexts.
Quality of Life of Caregivers: The quality of life of caregivers had significant differences in the physical domain with caregivers of schizophrenia subjects scoring low. The may be attributed to the fact that that the schizophrenia subjects had more number of parents as their caregivers who suffer from various minor physical ailments that causes pain, and who require varying degrees of medical help to lead their lives. The caregivers of schizophrenia subjects have poorer quality of life in the social domain as well, and there is no statistically significant difference in the psychological and environmental domains.
Depression in CaregiversThe mean MADRS score for caregivers of schizophrenia subjects was 9.88 and that of bipolar disorder subjects was 7.52. The difference was not statistically significant. Taking the cut off score as 14 which is the norm in most studies, 14 caregivers of schizophrenic subjects ie.28% and? Caregivers of bipolar subjects ie 14% were found to have clinical depression. Of the 100 caregivers assessed, 21 had clinical depression. This is concurrent with the findings of Li Yu Song et al. 78 where more than 20% of caregivers of chronic mental illnesses suffered from depression, but less than the study from Mexico76 where the rate was 40%.
Limitation And SuggestionsAlthough this study was limited with time constrain, manual-steps process but it was good to establish such a study in Saudi Arabia where SCD affects many patients particularly in Eastern and South Western areas.
Further studies are recommended to identify the specific compounds of different parts of these herbs that pharmacologically cause their therapeutic activity. Moreover, dose and additive effects as well as drug-interactions are suggested in future evaluation. In addition, in vivo researches with more objective, practical and validated advanced techniques are recommended, also, to correlate all of that with the disease phenotypes in multicentre analysis on larger cohort groups to provide more understanding of the beneficial effects of such plant products.
Conclusion
The study showed that though the burden of care of bipolar disorder is less when compared to schizophemia, it cannot be neglected. The QOL of caregivers of persons suffering from schizophrenia and bipolar disorder are comparable at least in the psychological and environmental domains. A significant number of caregivers of both schizophrenia and bipolar disorder suffer from clinical depression. Poverty and disruption of relationships and family integrity remain major factors in adding to the burden of both schizophrenia and bipolar disorder. No treatment of any chronic mental disorder is complete until the burden of care is assessed and addressed.
References
- Chakrabarti S, Raj L, Kulhara P, et al. Comparison of the extent and pattern of family burden in affective disorders and schizophrenia. Indian J Psychiatry 1995; 37:105.
- Provencher HL. Objective burden among primary caregivers of persons with chronic schizophrenia. J Psychi Mental Heal nurs 1996; 3:181-187 .
- Hamilton MW. The schizophrenic patient in the community and his effect on the household. International journal of social psychiatry 1966;12(3):165-176.
- Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: domains and distress. Schizo Bull 1998 Jan 1;24:609-618.
- De Jong A, Giel R, Slooff CJ, et al. Social disability and outcome in schizophrenic patients. The British Journal of Psychiatry 1985 Dec;147:631-636.
Author Info
Department of Psychiatry, Sree Balaji Medical College and Hospital, Chennai-600044, Tamil Nadu, IndiaCitation: Ajith Premnath, S.Nambi Study to Compare the Caregiver Burden of Schizophrenia and Bipolar Disorder, J Res Med Dent Sci, 2021, 9(9): 1-7
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021