Case Report - (2023) Volume 11, Issue 8
Submucosal vs. Oral Dexamethasone on Postoperative Sequelae Following Third Molar Surgery: A Comparative Study
*Correspondence: Dr. Kanimozhiy Senguttuvan, Department of Oral and Maxillofacial Surgery, Thai Moogambigai Dental College, Chennai, India, Email:
Abstract
Introduction: Surgical removal of the impacted third molar is a routine procedure performed in oral and maxillofacial surgery. Its post-operative sequelae include pain; swelling and trismus can cause distress to the patient and affect the patient’s quality of life after surgery. Controlling and minimizing the postoperative sequelae by various methods of giving NSAIDS, opioids and corticosteroids is common. Among that, corticosteroids are highly effective in controlling these undesirable effects postoperatively.
Aim: The aim of this study is to compare submucosal dexamethasone injection with oral dexamethasone which is administered preoperatively in reducing the postoperative sequelae after surgical removal of impacted lower third molar under local anesthesia.
Methods: This clinical study involved 40 patients who were segregated into two groups randomly.
• Group 1 (n=20) 4 mg of submucosal dexamethasone
• Group 2 (n=20) 4 mg of oral dexamethasone.
Results: Patients under group 1 were injected with submucosal dexamethasone showed facial swelling that was less evident with minimal restriction in mouth opening and less postoperative pain compared to that of oral dexamethasone that were part of group 2.
Conclusion: Pre-operative submucosal dexamethasone is considered better compared to oral dexamethasone for decreasing post-surgical sequelae.
Keywords
Dexamethasone, Impacted mandibular third molar, Oedema, Pain, Trismus
Introduction
Third molar removal represents a major part of oral and maxillofacial surgical practice. This procedure involves, injury to both soft and hard tissue which triggers inflammatory cascades resulting in synthesis of prostaglandins, leukotrienes, thromboxanes and related substances that acts as mediators for inflammatory response leading to postoperative sequelae like pain, swelling and trismus. NSAIDS and corticosteroids are widely used in minimizing and controlling postoperative pain and swelling. Among this, corticosteroids are successful in controlling acute inflammation by interfering with multiple signaling pathways in the inflammatory response primarily involving the suppression of leukocyte and macrophage aggregation and prevention of prostaglandin formation by disrupting the arachidonic acid cascade [1].
Dexamethasone has been extensively used in oral surgery due to its high potency and long half-life. It has several different routes of administration such as oral, intravenous, intramuscular and submucosal.
This study focuses on comparison between submucosal dexamethasone and oral dexamethasone in reducing postoperative sequelae after surgical removal of impacted lower third molar under local anesthesia [2].
Case Presentation
The study was conducted involving 40 patients, who presented with an impacted mandibular third molar to the department of oral and maxillofacial surgery, Thai Moogambigai dental college and hospital, Chennai. A detailed case history with relevant clinical examination was taken. The impacted mandibular third molar was assessed clinically and radiographically with an Orthopantomogram (OPG).
Risks, benefits, procedure and complications were explained to the patients. They were then divided into two groups.
• Group 1 (n=20) received 4 mg of submucosal
dexamethasone
• Group 2 (n=20) received 4 mg of dexamethasone
orally
The study was conducted after obtaining approval from the ‘institutional human ethical committee’.
Inclusion criteria:
• Patients with impacted lower third molar requiring
surgical removal.
• Age group 19 years to 30 years.
Exclusion criteria:
• Medically compromised patients.
• Pregnant and lactating women.
• Patients who are currently on steroid therapy for any
other disease.
Procedure
Under aseptic precautions, patients in group 1 were administered with 4 mg of submucosal dexamethasone and those in group 2 with 4 mg of oral dexamethasone preoperatively. All patients were given inferior alveolar nerve block (2% lignocaine with adrenaline 1:80,000). Incision was placed for surgical access and mucoperiosteal flap was raised, bone guttering was done and tooth removed. Wound irrigated with saline, flap closure was done using 3-0 black braided silk suture. Post-extraction instructions were given and prescribed with antibiotics and analgesics (NSAIDS). Patients were evaluated on 1st, 3rd and 7th postoperative day [3].
Results and Discussion
Evaluation criteria
Measurements of facial swelling, trismus and pain score were recorded preoperatively and also on the 1st, 3rd and 7th postoperative days by the same surgeon.
Facial swelling on the operated side was evaluated by two facial measurements: Tragus corner of the mouth (Dimension A) and lateral canthus gonion (Dimension B) (Figure 1).
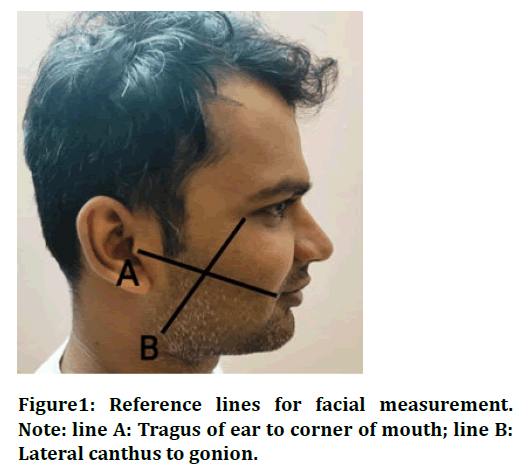
Figure 1: Reference lines for facial measurement. Note: line A: Tragus of ear to corner of mouth; line B: Lateral canthus to gonion.
Postoperative pain was evaluated using 10 point Visual Analogue Scale (VAS); on a scale of increase in pain severity from 0 to 10 (Figure 2).
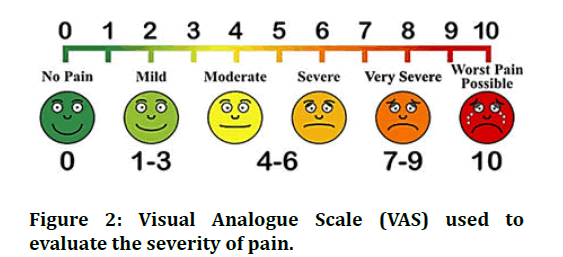
Figure 2: Visual Analogue Scale (VAS) used to evaluate the severity of pain.
Maximal mouth opening (inter incisal distance) was recorded to evaluate the trismus.
Statistical analysis
• Parametric independent t-test for inter group
comparison was applied after checking for normality
using EPI-INFO (version 7.2.2.6, CDC, license: Public
domain) software
• Significance level is fixed as 5% (α=0.05)
• Independent t test comparing both the groups
As the Levene’s test shows equality of variances, the independent t test p-value was found to be <0.05 with all the variables. An intergroup statistical evaluation of facial swelling measured using dimension-A revealed a significantly minimal increase in horizontal dimension among group 1 compared to group 2.
Evaluation of facial swelling measured using dimension B also revealed a significantly lesser vertical dimension among group 1 compared to group 2. Statistically significant reduction in pain (p<0.002) was observed after 1st, 3rd and 7th post-operative days revealing a comparatively lesser score on VAS among group 1 compared to group 2.
The result shows reduction in trismus on 1st, 3rd and 7th postoperative days. The difference between these mean reductions were found to be statistically significant (p<0.016) using independent t test with less trismus in group 1 compared to group 2. The surgical removal of impacted mandibular 3rd molar is a common oral surgical procedure which involves trauma to the surrounding soft tissues and guttering of bone around the teeth resulting in pain, swelling and trismus [4].
Postoperative oedema represents fluid accumulation in the interstitial area due to transudation from injured blood vessels and fibrin obstruction of lymph drainage resulting in swelling. Trismus is frequently caused by muscular spasm resulting from inflammation related to operative trauma. Pain has been attributed to pressure on nerve endings resulting from exudation. Pain following surgical removal of third molar is due to release of various mediators into the local environment, such as arachidonic acid metabolites, 5-HT and bradykinin. These mediators increase the responsiveness of local nociceptors [5].
Various treatment modalities have been tried to control the post-operative sequelae of third molar surgery. These include the use of steroids, serratio peptidase, NSAIDS etc. which have their own contraindications and adverse effects. Whereas, preoperative administration of antiinflammatory medication is more efficient in reducing pain than post-operative therapy [6].
Many authors have reported about the use of parenteral corticosteroids in oral surgery compared to oral and submucosal routes of administration. Effectiveness of the oral route of administration is dependent on the patient compliance. Orally administered gluco corticosteroids are rapid and almost completely absorbed however, repeated dose is required to maintain adequate blood levels. The intramuscular route allows the use of repository (acetate) drug forms, which provides slow absorption, prolonged anti-inflammatory effect but may pose a higher risk for adrenal suppression. Studies using intravenous drug dosing proposed that a single preoperative intravenous dose results in immediate but unsustained improvement in pain, swelling and trismus. Hence, intravenous dosing may require post-operative supplemental drug administration to be optimally effective. The submucosal administration of dexamethasone in lower than routine doses to achieve reduction of postoperative oedema comparable with or greater than other routes of administration. Apparently, injection of low dose dexamethasone in the surgical site achieves a higher effective drug concentration at the site of injury without loss due to distribution to other compartments or the onset of elimination [7].
Corticosteroids alone do not have a clinically significant analgesic effect, but has been reported with the reduction in the number of analgesic tablets required postoperatively. The results of this study show a statistically significant (p<0.002) decrease in patient’s pain perception observed in both the groups with the least among group 1 after first and seventh post-operative day. Our result indicates that steroids have synergistic effect with analgesics in controlling postoperative pain [8].
There was a significant difference (p<0.016) between the groups in the inter incisal mouth opening on the first and seventh post-operative days. It shows that steroids have definite role in controlling postoperative trismus. This is comparable with the retrospective study conducted by Michael R. et al., who found that trismus was lesser among those administered with corticosteroid compared to the control group. Our result suggests oral dexamethasone is less effective in controlling the trismus when compared with submucosal dexamethasone at when assessed on the first post-operative day [9].
In both the groups, facial swelling was most severe on the first post-operative day after surgery and began to return to normal baseline facial contour by the seventh day post-operatively. Post-operative oedema tended to be less severe among group 1 on the first day when compared to group 2. Other studies in the past have also demonstrated that administration of steroids showed reduced incidence of oedema postoperatively [10]. Even when teeth are extracted utilizing a delicate surgical approach, the surgical removal of third molars is frequently accompanied by acute postoperative agony. As a result, several medical professionals have tried to use anti-inflammatory medications to lessen the postsurgical side effects. When third molars are extracted, corticosteroids are frequently used due to their antiinflammatory effectiveness. In dento alveolar surgery, corticosteroids like dexamethasone and methylprednisolone have been utilized a lot [11,12].
Dexamethasone 4 mg submucosal injection is an efficient therapeutic approach for enhancing quality of life following surgical removal of impacted lower third molars with an effect on postoperative sequelae comparable to intramuscular administration. For moderate and severe instances, it provides a straightforward, secure, painless, noninvasive and economical therapeutic option [13-15].
Conclusion
Administration of steroids have a definite role in reducing post-operative swelling, trismus and pain in patients undergoing surgical removal of impacted mandibular third molar. The test drugs used in this study were well tolerated and safe with no complications or side effects. This study shows that preoperative sub mucosal administration of steroids has a better antiinflammatory action depicting significantly lesser pain, oedema and trismus postoperatively compared to that of oral administration.
References
- Neupert III EA, Lee JW, Philput CB, et al. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg 1992; 50:1177-1182.
[Crossref] [Google Scholar] [PubMed]
- Gersema L, Baker K. Use of corticosteroids in oral surgery. J Oral Maxillofac Surg 1992; 50:270-277.
[Crossref] [Google Scholar] [PubMed]
- Dionne RA, Gordon SM, Rowan J, et al. Dexamethasone suppresses peripheral prostanoid levels without analgesia in a clinical model of acute inflammation. J Oral Maxillofac Surg 2003; 61:997-1003.
[Crossref] [Google Scholar] [PubMed]
- Markovic A, Todorovic LJ. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: A clinical trial. Int J Oral Maxillofac Surg 2007; 36:226-229.
[Crossref] [Google Scholar] [PubMed]
- Roynesdal AK, Bjornland T, Barkvoll P, et al. The effect of soft-laser application on postoperative pain and swelling: A double-blind, crossover study. Int J Oral Maxillofac Surg 1993; 22:242-245.
[Crossref] [Google Scholar] [PubMed]
- Hooley JR, Hohl TH. Use of steroids in the prevention of some complications after traumatic oral surgery. Int J Oral Maxillofac Surg 1974; 32:864-866.
[Google Scholar] [PubMed]
- Troullos ES, Hargreaves KM, Butler DP, et al. Comparison of nonsteroidal anti-inflammatory drugs, ibuprofen and flurbiprofen, with methylprednisolone and placebo for acute pain, swelling and trismus. J Oral Maxillofac Surg 1990; 4:945-952.
[Crossref ] [Google Scholar] [PubMed]
- Esen E, Tasar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg 1999; 57:1201-1206.
[Crossref ] [Google Scholar] [PubMed]
- ElHag M, Coghlan K, Christmas P, et al. The anti-inflammatory effects of dexamethasone and therapeutic ultrasound in oral surgery. Br J Oral Maxillofac Surg. 1985; 23:17-23.
[Crossref ] [Google Scholar] [PubMed]
- Amin MM, Laskin DM. Prophylactic use of indomethacin for prevention of postsurgical complications after removal of impacted third molars. Oral Surg Oral Med Oral Radiol 1983; 55:448-451.
[Crossref ] [Google Scholar] [PubMed]
- Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose prednisolone with and without diclofenac on pain, trismus and swelling after removal of mandibular third molars. J Oral Maxillofac Surg 2006; 64:1761-1766.
[Crossref ] [Google Scholar] [PubMed]
- Chopra D, Rehan HS, Mehra P, et al. A randomized, double-blind, placebo-controlled study comparing the efficacy and safety of paracetamol, serratiopeptidase, ibuprofen and betamethasone using the dental impaction pain model. Int J Oral Maxillofac Surg 2009; 38:350-355.
[Crossref ] [Google Scholar] [PubMed]
- Grossi GB, Maiorana C, Garramone RA, et al. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: A prospective study. J Oral Maxillofac Surg 2007; 65:2218-2226.
[Crossref ] [Google Scholar] [PubMed]
- Gupta S, Padhyae M. Efficacy of dexamethasone in wisdom tooth extraction-a double blind split technique. Int J Oral Maxillofac Surg 2007; 36:1006.
- Markiewicz MR, Brady MF, Ding EL, et al. Corticosteroids reduce postoperative morbidity after third molar surgery: A systematic review and meta-analysis. Int J Oral Maxillofac Surg 2008; 66:1881-1894.
[Crossref ] [Google Scholar] [PubMed]
Author Info
Department of Oral and Maxillofacial Surgery, Thai Moogambigai Dental College, Chennai, IndiaCitation: Kanimozhiy Senguttuvan, Submucosal vs. Oral Dexamethasone on Postoperative Sequelae Following Third Molar Surgery: A Comparative Study, J Res Med Dent Sci, 2023, 11 (08): 041-044.
Received: 15-Nov-2021, Manuscript No. JRMDS-23-47423; , Pre QC No. JRMDS-23-47423 (PQ); Editor assigned: 18-Nov-2021, Pre QC No. JRMDS-23-47423 (PQ); Reviewed: 02-Dec-2021, QC No. JRMDS-23-47423; Revised: 19-Jul-2023, Manuscript No. JRMDS-23-47423 (R); Published: 16-Aug-2023
