Review Article - (2022) Volume 10, Issue 9
Temporomandibular Disorders: A Comprehensive Review
Mansi Sharma*, Sunita Shrivastav and Purva V Dhannawat
*Correspondence: Mansi Sharma, Department of Orthodontics and Dentofacial Orthopedics, Sharad Pawar Dental College and Hospital, Datta Meghe institute of Medical Science (Deemed to be University), Sawangi (Meghe), Maharashtra, India, Email:
Abstract
TMD (Temporomandibular Disorder) is musculoskeletal condition ofmasticatory system that causes discomfort as well as dysfunction with in jaw's joints and other structures. TMD is commonly seen as a masticatory repetitive motion condition with several similarities to musculoskeletal illnesses. Temporomandibular disorders are characterized by reducedmandibular range ofmuscle, motionand joint discomfort, joint crepitus, and limited mobility or deviations in jaw opening. The utmost common sign of temporomandibular disorder is ache in masticatory muscles and TMJ. Temporomandibular dysfunction pain has a complex cause. According to several researches, predisposing, initiating, and aggravating factors all play a role in this condition. Commonest diagnosis is based on the patient's medical and physical investigation. When there is a probability of malocclusion or intra-articular abnormalities, diagnostic imaging may be helpful. The majority of patients benefit from non-invasive treatments includes individual’s education, personal care, medicine, perceptive behaviour therapy, physical treatment or occlusal strategies. Replacement of the temporomandibular joint is reserved for seriously affected joints that have failed all otherconservative treatment methods.Keywords
TMD, Temporomandibular dysfunction, Aetiology, Diagnosis of TMD
Introduction
TMD (Temporomandibular Disorder) is musculoskeletal condition ofmasticatory system that causes discomfort as well as dysfunction with in jaw's joints and other structures. According to the glossary of prosthodontic terms, Temporomandibular Disorders (TMD) are defined as: "Conditions producing abnormal, incomplete or impaired function of the temporomandibular joint(s)" or "a collection of symptoms related to the masticatory system, frequently observed in various combinations" [1]. Others have defined TMD as a collective term, embracing several clinical problems involving the muscles, Temporomandibular Joint (TMJ), or both [2].
TMD is a frequent problem with adults from the age of 20 to 40. Over 33% of people seem to have minimum single symptom of temporomandibular disorder, while 3.6% to 7%of individuals have this disorder more complicated which requires treatment. Those with TMD might havevariety of sub-diagnoses, such as myofascial pain and TMJ inflammation [3]. A self-reported anamnestic questionnaire is used to estimate the prevalence and severity of TMD. TMD affects 34.83% of people, 8.38 percent of people have moderate TMD, and 1.96% of people have severe TMD.
TMDs (especially those of myofascial origin) are commonly related to psychological, social, as well as behavioural components, equivalent to certain other chronic pains, somesymptoms such as anxiety, anger, frustration, and depression, and also the habitssuch as bruxism, bad posture, inadequate physical activity, poor dietary andsleep habits,dependencies over drugs, as well as other tension related habits, could be present. Each of these signs or behaviours has the potential to muddle the clinical picture. Instructions for self-management of TMD, ask patients for resting their masticatory muscles by avoiding hard or chewy foods and preventing from activities that overuse the masticatory muscles (e.g., oral habits, clenching teeth, chewing gum, and yawning wide) [4]. As with other musculoskeletal disorders, pain during function and/or at rest is the primary reason patients seek treatment, and reduction in pain is generally the primary goal of therapy. Masticatory stiffness, restricted mandibular motion, TMJ dislocation, and unexplained occlusion are all indications of TMJ catching and locking in which people seek TMD therapy (change in position ofmandibular midline and either anterior or posterior open bite). Onother hand, TMJ noisesare frequent in the general population whichare typically unrecognized by individuals or practitioner and are infrequently treated which may not respond to treatment [5]. The goal of such a scientific outlook is just for presenting the assessment andhandling of TMD throughthe perspectives of both thedentist and thephysical therapist. When the dentist lacks expertise or the management of the patient's condition begins to exceed their capacity to handle independently, the dentist should consider cooperating with other health care providers, such as the patient's physician or competent medical or dental experts. Before beginning any surgery that may permanently affect the dentition or jaw connections, the patient must be fully informed of the hazards. Consent that is truly informed is critical. Re-evaluation during therapy is also necessary to ensure that the diagnosis is correct and that the treatment path is suitable.
TMD is a disability of the TMJ which impairs normal jaw function and thus land up in handicapped situation for the patient to perform normal masticatory function. Paucity of appliances and methods of intervention of TMD makes it one of the most neglected aspects in orthodontics and it also adversely affects the functional ability of patient. Many appliances are there for the treatment of TMD but no appliance will give definitive treatment. TMD may get worsen due to orthodontic treatment so it should for diagnosed and treated before starting treatment.
There are different treatment modalities available for treating TMD which can be categorized as conservative treatment in which comes are physical treatment, local steam application, external muscle relaxation, occlusal alteration, analgesia, psychotropic medicine, splint therapy, alternative therapies which includes acupuncture, treatment modalities for example ultrasound, easy laser, diathermy, infrared radiation and surgical managing [6]. Purpose of this study is to reassess information regarding etiology, diagnosis and treatment planning of temporomandibular disorder. So, the current article reassessed the narrative regarding temporomandibular disorders.
Literature Review
History of TMDs
Historically, rather than research the dentist lacks expertise or the treatment of the patient's condition starts to cross thelimit oftheir capacity to handle independently, the clinicianshould consider cooperating with other health care providers, such as the patient's physician or competent medical or dental experts. Before beginning any surgery that may permanently affect the dentition or jaw connections, the patient must be fully informed of the hazards. Consent that is truly informed is critical. Re-evaluation during therapy is also necessary to ensure regarding thediagnosis is accurate andthe treatment path is suitable. In 1940 and 1950, the significance of occlusal therapies in masticatory muscle diseases where given [7]. In 1960 and 1970, occlusion and eventually emotional tension were reported as the major cause of functional masticatory system disorders. Further in the 1970’s an explosion of interest inpain disordersarising from intracapsular sources was concerned and described by Farrar and McCarty [8]. The majority of TMD patients benefit from non-invasive, conservative treatment to alleviate their symptoms.
Etiology
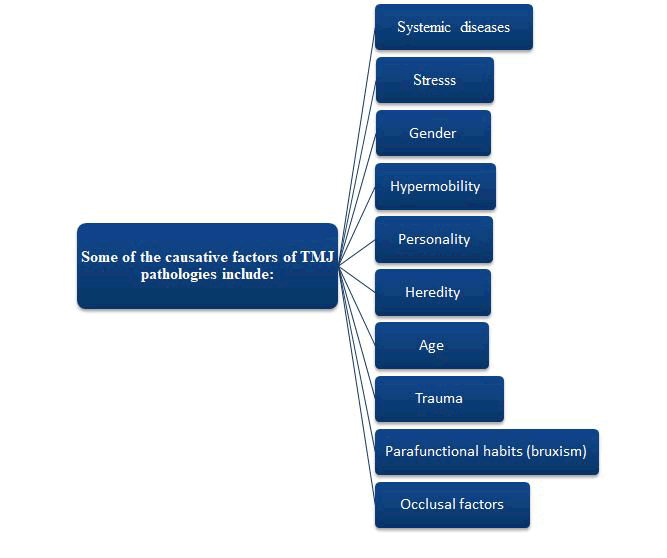
The causative factors and etiology of temporomandibular disorders are complex and multidimensional (Figure 1). The factors that mainly contribute to TMD disorder are biomechanical, bio psychosocial, neuromuscular and neurobiological [9]. These several factors are classified into three:
- Pre-disposing factors: these factor increases the risk of TMD
- Medical diseases such as rheumatic infections, dietary and metabolic issues are examples of systemic factors.
- Personality and behaviour-Psychological elements
- Structural reasons-occlusal discrepancies of all kinds, poor tooth hygiene Factors that are genetic
- Initiating factors: these factor causes the onset of TMD
- Trauma-Micro or macro trauma
- Perpetuating factors (para function, hormonal, or psychosocial factors): these factors mainly interfere with the process of healing which enhances the progression of TMD [10].
- Mechanical and muscular stress
- Metabolic issues
- Overloading of joint structures–Para functional habits, etc.
Figure 1: Some of the causative factors of TMJ pathologies.
Occlusal conditions
The main causative factor earlier, in which the correlation between occlusal variables and TMD and their contribution to TMD, has been an intense discussion in the dentistry. Both static and dynamic circumstances should be used to assess the link between occlusion and TMDs. Reverse articulation, for example, is thought to cause asymmetric muscle function, but whether or not it is linked to TMD has yet to be determined [11]. However, four occlusal structures mainly appeared in patients:
- Occurrence of skeletal anterior open bite,
- Retruded interaction site and intercuspal site slides of superior than 4 mm,
- Overjet of more than 6-7 mm,
- 5 or additional misplaced, unreplaced posterior teeth [12].
Trauma
The circumstance that, the trauma causes TMDs has sufficient evidences in which intra capsular disorders have a bigger impact than muscle problems. There are two types of traumas: macro trauma and micro trauma. The most prevalent structural changes affecting the TMJ caused by macro trauma are elongation of the discal ligaments. Direct (open mouth, close mouth, iatrogenic) and indirect (non-iatrogenic) trauma are the two types of macro trauma in which TMJ injury is caused by rapid force which do not immediately strike and interacts the mandible. Micro trauma is defined as any little force applied repeatedly to joint structures over a lengthy period of time [13].
Emotional stress
Stress and personality have been studied extensively for aetiology of temporomandibular pain dysfunction syndrome. Psychological studies shows patient with temporomandibular disorders might have psychological appearances and dysfunction which are similar to chronic musculoskeletal pain disorders as headache and arthritis pain [14]. The association between depression and stress and different physical symptoms of TMD is widely acknowledged [15]. The relations in the psychological features and Para functions have been underlined in several studies [16]; Psychological factors mainly have an indirect effect rather than direct effect on TMD symptoms. The general level of depression or anxiety might alter the grinding and clenching habits [17].
Parafunctional factor (bruxism)
TMD has been associated to bruxism as an initiating or recurring cause. Prior studies directed that 87.5% of patients have myofascial pain and displacement of disc and 68.9% of myofascial pain patient’s reports of clenching teeth [18]. This hypothesized that bruxism might be aetiology factor for myofascial discomfort, masticatory muscle ache, and TMJ pain [19].
Clinical features
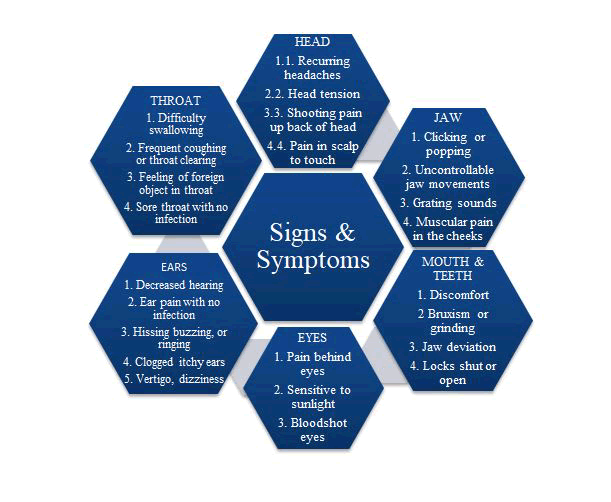
Clinical features show in Figure 2.
Figure 2: Signs and symptoms.
Diagnostic criteria for TMD
Diagnosis: TMD is diagnosed mainly fromthe patient's medical history and physical examination findings. Jaw movement such as opening and closing the mouth, chewing and pain in the pre auricular, masseter or temporal region are common TMD symptoms. If pain is not relieved by adjusting the jaw, another cause of orofacial pain should be considered. TMD can cause unusual jaw noises (such as clicking, cracking, crepitus), although it can also happen in up to 50% of people with no symptoms [20].Commonest prevalent signs and symptoms, according to great reflective research (n=4,528) conducted by a single examiner over 25 years are facial pain, ear discomfort, headache, and jaw discomfort or dysfunction [21].Extra signs and indications maybe drowsiness, ache in neck, eye, arm, or back region.
Imaging: Plain radiography, such as panoramic radiography, can detect dislocations, acute fractures or severe degenerative disease, whereas computer tomography permits more thorough analysis of delicate bony morphology. MRI is the ideal imaging modality for TMJ. In symptomatic patients, MRI findings and joint morphology have a 78-95% association. Ultrasound, which is dynamic, affordable, non-invading method of diagnosing inner TMJ dysfunction in absence of an MRI [22].
Questionnaire: The questionnaire was used to evaluate the degree of TMD in the participants. The questionnaire is framed of series of questions, evaluating for the presence of pain in TMJ, head, and while chewing, Para functional habits, limitation of movements, joint clicking, and perception of malocclusion, and emotional stress, which becomes a vital instrument for diagnosis [23].
Various indexes are:
- Helkimo Index
- Fonseca Index
- Research Diagnostic Criteria for TMD
- Craniomandibular Index
- TMD Disability Index
Frequently accepted criteria for TMD evaluation is research diagnostic criteria. The developed RDC/TMD Axis I diagnostic algorithms arevalid for the most severe pain-related TMD as well asTMJ intra-articular condition. The RDC/TMD Axis II instruments are accurate and reliable.
Physical examination: A thorough physical examination will aid in identifying the source of discomfort and the severity of the condition. TMJ assessment includes joint range of motion, pain palpation, joint sound inspection and muscle palpation in the section of the evaluation. For some patients, additional diagnostic testing may be required. Dental and occlusal evaluations are also performed [24].
TMJ evaluation: Pain on palpation, range of Joint’s motion and joint sounds are present during movements of mandibleand opening movement are all common criteria for a TMJ clinical examination.
TMJ range of motion: Limitation in mouthopening and difficulty in mandibular mobility are two of the major complaints. The patient is being asked to open their mouth completely, and total of interincisal measurement and overbite is recorded using the millimetre rule. The usual maximal opening is between 45 and 55 mm, while lesser figures are common in asymptomatic individuals [25]. To evaluate deviation or deflection, the mandibular closing and opening movements could keep on performing in the straight line. Protrusion measurements, as well as lateral right and left movements, should be recorded. It is advised tomark 2 markings points on mandible and maxilla, approximately towards midline, for those measurements. These reference areas shall provide a movement series which measures mandibular excursion.
Recognition of the joint sounds: The presence of joint noises during mouth opening and mandibular excursion can help todetect disc-condyle incoordination. The clinical assessment of articular sounds using physical examination or stethoscope is considered to be quite effective [25]. The maximum frequent sounds in TMD patients are clicking, a terminal thud (relative to hyper translation) and crepitation.
TMJ palpation: One of the most essential indicators in the identification of intra capsular diseases is tenderness upon palpation. The physician should look for the lateral polo of the mandibular condyle following repeated opening and closing movements. Simultaneously, with the patient’s mouth in a comfortable situation, bilateral tactual exploration of lateral part of the TMJ should be performed. Pressure of 1 kg should be applied to the lateral and posterior sides of the joints during this palpation. Capsulitis and/or synovitis can be diagnosed based on pain reports. Scores ranging from 0 to 3 can be used to grade the patient's response to palpation which indicates as follows:
- 0=indicates no pain when palpated
- 1=indicates slight discomfort
- 2=indicates sensible pain
- 3=indicates acute pain, palpebral reaction, and "jump sign" [26].
Palpation of the muscles: Tactual exploration of muscles is an essential part of themyofascial pain and temporomandibulardisorders diagnosis process. Nociceptive neurons in the muscle and myofascial tissues are triggered by mechanical stimuli which areinduced by digital pressure,to detect and transfer pain messages to the CNS. Progression of a patient's response to palpation is used to determine the intensity of the pain and for assessing a success of treatment during recall visits. If there is no underlying bone support, palpation must be done bilaterally byafingers tipor viapincer palpation in therelaxed state. The posterior, medial, and anterior temporalis muscles, as well as the superficial and deep masseters and the attachment of the medial pterygoid muscle, should all be explored. Significant cervical muscles which are also taken into account in this assessment include the sternocleidomastoid,sub occipital and superior trapezius [27].
Dental and occlusal estimation
Dental investigation: Periodontal disorders which may causepain,such as poor restorations ormissing teeth, should be diagnosed during this time. The majority of orofacial pain is caused by dental problems. Dental attrition on the incisal or occlusal surfaces can also signify parafunctional behaviours [28].
Occlusal examination: The over jetand overbiteare determined by the existence otherwise by lack of adjacent and frontal guides. The patient is requested to conduct lateral mandibular motions with a cellophane paper to detect occlusal interfering on the side that is not in used [29].
Additional diagnostic tests: Additional testing can assist todefine a diagnostic impression if there is still any doubt. And here it is where modulation of functional muscles, cryotherapy,TMJ overworking, also investigative nerve blocking is beneficial [29].
Treatment
TMD treatment is usually required in 5-10% of individuals; however, 40% of cases recover on their own. Conservative therapy is estimated to be 50-90% successful in studies. Surgical intervention is usually reserved for patients in whomsymptoms hadnot responded to non-surgical therapy.
Non-pharmacological management
Patient Instruction
- Jaw relaxation, passive stretching exercises, soft diet, warm compress.
- Immobilization of Temporomandibular joint is ineffective.
Physical Therapy (PT)
- There is lack of evidences to justify the use of specialised physical treatment such as ultrasonography and electrotherapy.
- Range of motion, coordination, muscle strength and relaxation should all be improved.
Acupuncture
- It is utilized in treatment of myofascial pain.
Biofeedback
- In case of short and long-span treatment of TMD, cognitive behaviour therapy and biofeedback therapy are recommended.
- Examples are: avoiding excessive mandibular movements, stress modification, elimination of Para functional habits, and sleep hygiene.
Iontophoresis
Occlusal splints and adjustments. According to Okeson [2].
- Stabilization appliance
- Anterior Repositioning Appliances (ARA)/Mandibular Orthopedic Repositioning Appliance (MORA)
Other types - Anterior/Posterior bite plane
- Pivoting appliance
- Soft/resilient appliance (silicone)
Surgery: Condylotomy, Arthrocentesis, Arthroscopy, Discectomy for modification in anatomic or articular deviations. Surgical procedures have been demonstrated to improve joint mobility and alleviate TMD symptoms.
Pharmacological therapy
- Acetaminophen
- Anxiolytics
- Benzodiazepines
- Muscle relaxants
- Non-steroidal anti-inflammatory drugs
- Tricyclic antidepressants
- Intra-articular corticosteroids or anaesthetic injections [30].
Discussion
Temporomandibular disorder is musculoskeletal condition of masticatory system that causes discomfort as well as dysfunction within jaws, joints and other structures [31-35]. They are characterized by reduced mandibular range of muscle, motion and joint discomfort, joint crepitus, and limited mobility or deviations in jaw opening. The most common symptom of TMD is pain in the masticatory muscles and temporomandibular joint. Additional signs and symptoms may be drowsiness, pain in the neck, eye, arm, or back region. It impairs normal jaw function and thus land up in handicapped situation for the patient to perform normal masticatory function. The factors that mainly contribute to TMD disorder are biomechanical, bio psychosocial, neuromuscular and neurobiological [9]. Some of the causative factors of TMJ pathologies include stress, hypermobility, heredity, age, trauma, Para functional habits (bruxism), occlusal factors. TMD is diagnosed mainly from the patient's medical history and physical examination findings [20,36-40]. TMD treatment is usually required only in 5-10% of individuals, 40% of cases recover on their own, which mainly includes non-pharmacological therapy, conservative therapy, surgical intervention and pharmacological therapy [41-45].
Conclusion
Dentist is challenged by a temporomandibular mandibular problem at any time and must be prepared to describe it completely even if diagnosis is not possible. This concern becomes absolute when dentist accepts global rehabilitation projects that require an effective mandibular reference position, centric relation, which depends on the state of the musculo articular relationship. Dentist can make a right management posture and adapt the treatment plan to serve the patient's best interests by precisely discovering the source of an existing problem and assessing the risk factors. Dentist must remain careful, well aware of the occlusal condition and ready to change occlusion as needed, without neglecting the importance of establishing a differential diagnosis that excludes "non-TMD" diseases that can be significantly more harmful.
References
- Ferro KJ, Morgano SM, Driscoll CF, et al. The glossary of prosthodontics terms. J Prosthetic Dent 2017;117:1-105.
- Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dental Clinics 2011; 55:105-120.
- Okeson JP. American Academy of Orofacial Pain. De Leeuw R, ed. Orofacial Pain: Guidelines for Assessment, Diagnosis and Management. 4th ed. Chicago: Quintessence 2008.
- Wright EF. Manual of Temporomandibular Disorders. 4th ed, Wiley-Blackwell, Hoboken, NJ, USA, 2005.
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 6th ed. St. Louis, MO: CV Mosby 2008.
- Murphy E. Managing Orofacial Pain in Practice. Oxford: Wiley-Blackwell, 426, 2008.
- Ribeiro RF, Tallents RH, Katzberg RW, et al. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J Orofac Pain 1997; 11:37-47.
- Egermark I, Carlsson GE, Magnusson T, et al. A 20 years longitudinal study of subjective symptoms of temporomandibular disorders from childhood to adulthood. Acta OdontolScand 2001; 59: 40–48.
- Magnusson T, Egermark I, Carlsson GE, et al. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J OrofacPain 2000; 14:310–319.
- Wassell RW, Adams N, Kelly PJ, et al. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: One-year follow-up.
- Dhannawat P, Shrivastav S, Ranjit K, et al. Different Types of Occlusal Splint Used In Management of Temporomandibular Joint Disorders-A Review.Europ J Mol Clin Med 2020; 7:1787-1794.
- Jeffery P Okeson. Management of temporomandibular disorder and occlusion. 4th edition, Elsevier Health Sciences, 2019.
- WBFarrar,WLMcCartyJr. The TMJ dilemma. J Ala Dent Assoc 18979;63:19-26.
- Suvinen TI, Reade PC, Hanes KR, et al. Temporomandibular disorder subtypes according to self-reported physical and psychosocial variables in female patients: a re-evaluation. J Oral Rehabil 2005; 32:166-73.
- McNeill C. Evidence-based TMD guidelines. J Orofac Pain 1997; 11:93.
- Sharma S, Gupta DS, Pal US, et al. Etiological factors of temporomandibular joint disorders. Nat J Maxillofac Surgery 2011; 2:116-119.
- Landi N, Manfredini D, Tognini F, et al. Quantification of the relative risk of multiple occlusal variables for muscle disorders of the stomatognathic system. J Prosthet Dent 2004; 92:190-195.
- McNamara JA Jr, Seligman DA, Okeson JP. Occlusion, Orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain 1995; 9:73-90.
- Pullinger AG, Seligman DA. A multiple logistic regression analysis of the risk and relative odds of TMDs as a function of common occlusal features. J Dent Res 1993; 72:968-979.
- Bhat S. Etiology of temporomandibular disorders: the journey so far. Int Dentistr sa 2010; 12:88-98.
- Suvinen TI, Hanes KR, Reade PC, et al. Outcome of therapy in then conservative management of temporomandibular pain dysfunction disorder. J Oral Rehabil 1997; 24:718-724.
- Suvinen TI, Reade PC. Temporomandibular disorders: a critical review of the nature of pain and its assessment. J Orofac Pain 1995; 9:317-339.
- Dworkin SF, Massoth DL. Temporomandibular disorders and chronic pain: disease or illness? J Prosthet Dent 1994; 72:29-38.
- Lupton DE. Psychological aspects of temporomandibular joint dysfunction. J Am Dent Assoc 1969; 79:131-136.
- Molina OF, J dos Santos Jr. Hostility in TMD/bruxism patients and controls: a clinical comparison study and preliminary results. Cranio 2002; 20:282-288.
- Velly AM, Gornitsky M, Philippe P, et al. Contributing factors to chronic myofascial pain: a case-control study. Pain 2003; 104:491-499.
- Manfredini D, Cantini E, Romagnoli M, et al. Prevalence of bruxism in patients with different Research Diagnostic Criteria For Temporomandibular Disorders (RDC/TMD) Diagnoses. Cranio 2003; 21:279-285.
- Huang GJ, LeResche L, Critchlow CW, et al. Risk factors for diagnostic subgroups of painful Temporomandibular Disorders (TMD). J Dent Res 2002; 81:284-288.
- Scrivani SJ, Keith DA, Kaban LB, et al. Temporomandibular disorders.N Engl J Med 2008; 359:2693–2705.
- Cooper BC, Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders.Cranio 2007; 25:114–126.
- Bas B, Yilmaz N, Gokce E, et al. Diagnostic value of ultrasonography in temporomandibular disorders.J Oral Maxillofac Surg 2011; 69:1304–1310.
- Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state.Sven Tandlak Tidskr1974; 67:101–121.
[Crossref]
- Fonseca DM.Craniomandibular Dysfunction (DCM): Diagnosis by the Anamnesis [Master's Dissertation]Bauru: Faculty of Dentistry of Bauru of USP 1992.
- Okeson JP. History and examination for temporomandibular disorders. In: Okeson JP. Management of temporomandibular disorders and occlusion. Saint Louis: Mosby-Year Book; 1993; 245-320.
- Dworkin SF, Huggins KH, LeResche L, et al. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6:301-355.
- Fischer AA. Pressure threshold measurement for diagnosis of myofascil pain and evaluation of treatment results. Clin J Pain 1987; 2:207-214.
- Graff-Radford SB, Solberg WK. Atypical odontalgia. J Craniomandib Disord 1992; 6:260-265.
- Austin DG, Peters RA. Examination of the TMD patient. In: Peters RA, Gross SG. Clinical management of temporomandibular disorders and orofacial pain Chicago: Quintessence 1995; 123-160.
- Gauer R, Semidey M. Diagnosis and Treatment of Tempomandibular Disorders. American Academy of Family Physicians 2015; 91:378-388.
- Naqvi WM, Fating TB. Temporomandibular joint dysfunction: A non-invasive approach towards the management of a long-standing condition. Int Jou Pharm Res 2020; 12:1131–1134.
[Crossref]
- John ZAS, Shrivastav SS, Kamble R, et al. Three-dimensional comparative evaluation of articular disc position and other temporomandibular joint morphology in Class II horizontal and vertical cases with Class i malocclusion. A magnetic resonance imaging study. Angle Orthodontist 2021; 90:707–714.
- Shyamsukha B, Nimonkar S, Belkhode V, et al. Prevalence of temporomandibular disorders among medical students of Wardha district: A cross-sectional study. J Datta Meghe Inst Med Sci 2021; 16:47–51.
- Mohabey A, Gupta S, Gawande V, et al. A study on correlation of magnetic resonance imaging and arthroscopy in evaluation of anterior cruciate ligament injury in cases of acute traumatic haemarthrosis of knee: A prospective study. Int J Curr Res and Rev 2020; 12:14–17.
[Crossref]
- Naik S, Agarwal S, Prakash S, et al. Autologous PRP injection: A safe solution for plantar fasciitis. J Arthroscop Joint Surg 2021; 8:253–255.
[Crossref]
Author Info
Mansi Sharma*, Sunita Shrivastav and Purva V Dhannawat
Department of Orthodontics and Dentofacial Orthopedics, Sharad Pawar Dental College and Hospital, Datta Meghe institute of Medical Science (Deemed to be University), Sawangi (Meghe), Maharashtra, IndiaCitation: Mansi Sharma, Sunita Shrivastav, Purva V Dhannawat,Temporomandibular Disorders: A Comprehensive Review, J Res Med Dent Sci, 2022, 10 (9): 000-000.
Received: 18-Jun-2022, Manuscript No. JRMDS-22-47345; , Pre QC No. JRMDS-22-47345; Editor assigned: 21-Jun-2022, Pre QC No. JRMDS-22-47345; Reviewed: 05-Jul-2022, QC No. JRMDS-22-47345; Revised: 22-Aug-2022, Manuscript No. JRMDS-22-47345; Published: 01-Sep-2022