Research - (2019) Volume 7, Issue 2
The Effect of Psychiatric Interventions on Depression and Fertility in Infertile Patients with Polycystic Ovarian Disease
Fatemeh Ramazanzadeh1, Ahmad Ali Nourbala2, Fatemeh Davari Tanha2 and Fatemeh Mostaan1*
*Correspondence: Fatemeh Mostaan, Department of Obstetrics and Gynecology, School of Medicine, Imam Khomeini Hospital, Iran, Email:
Abstract
Background: Nowadays, about 12% of couples face infertility problems that overwhelm their personal and social life. Psychosocial problems reported in infertile patients include depression, aggression, anxiety, sexual dysfunction, incompatibility, lack of individual control and decreased self-esteem. Polycystic Ovary Syndrome (PCO) is the most common endocrine disorder leading to infertility in women.
Objective: This clinical trial study aimed to investigate the effect of psychiatric interventions on depression and fertility in infertile patients with polycystic ovarian in comparison with non-polycystic ovarian disease.
Methods and Materials: This clinical trial study was carried out on 62 infertile women (41 cases with PCO and 31 cases without PCO) who had depression and referred to Valiasr hospital in Tehran during 2011-2012. All patients fulfilled the General Health Questionnaire-28 (GHQ-28). Those who scored at least 21, fulfilled Beck Depression Inventory (BDI-II) to check depression and patients who scored at least 17, referred to a psychiatrist to be treated with Fluoxetine 20-60 mg/day or psychotherapy. Three months after the start of treatment, beck questionnaire was examined again and after four weeks after the start of the intervention, the fertility success rate was examined by β-hCG test. Unjustifiable infertile patients, infertility with mannish causes including oligospermia or azoospermia, having with moderate to severe endometriosis, infertile patients previously treated with Invitro- fertilization (IVF) or Intra-cytoplasmic sperm injection (ICSI), and patients with infertility longer than five years were excluded. Data were analyzed using SPSS version 16 statistical software. The relationship between variables was investigated using chi-square; t-test and ANOVA repeated measure. The significance level was considered <0.05.
Results: Mean age of the patients in the intervention and control groups was 26.55 year and 26.08 years old, respectively. Both groups were homogeneous regarding age, education, occupation, type of infertility (primary or secondary), history of psychology disorder and duration of infertility (p>0.05). The fertility rate was significantly different in the two groups after the intervention (20 patients in the intervention group and only 3 in the control group) (p=0.0001). Among those who were pregnant after the intervention, 9 patients (64.2%) had PCO and 11 patients (64.7%) had no PCO (p=0.999). Mean score of Beck questionnaire in the intervention group changed from 25.48 to 13.12 (p=0.0001), but in the control group remained unchanged.
Conclusion: Psychiatric interventions in infertile patients with depression, in addition to their positive effect on the improvement of their depression, increase their fertility success rate.
Keywords
Depression, Fertility, Infertility, Polycystic ovarian
Introduction
Polycystic Ovary Syndrome (PCO) is a serious endocrine disorder and is a major cause of female infertility accompanied with ovarian and menstrual disorders, hyperandrogenism, and insulin resistance [1-3]. PCO is defined as ovulation disorder, hyperandrogenism, and other related disorders [4]. PCO is caused by a combination of genetic, neuroendocrine and metabolic factors [5]. PCO is affecting 4%-11% of women of reproductive age [6]. PCO is seen in premenopausal women or patients with type 2 diabetes [7-9].
Ovulation disorders may be clinically manifested as oligomenorrhea or amenorrhea. Hyperandrogenism manifests as hirsutism, acne or alopecia [10]. PCO is more common in women with seizure and is found in 10%-21.5% of patients with PCO [11,12]. Epileptic seizures may affect the secretion of Gonadotropinreleasing hormone (GnRH) which produces a high level of LH secretion and an increased ratio of LH/FSH [13,14].
It seems that the PCO is a complex of polygenic or genetically disrupted disorders that involves a spectrum of the ovarian androgen to the insulin receptor biosynthesis. Cooper et al. reported that a history of oligomenorrhea and polycystic ovary in mothers and sisters of patients with PCO was more common in comparison to the control group as well as male relatives often have pilosity, while supposed mechanisms was dominant autosomal inheritance [15].
In Iran, depression was studied in infertile couples, in such a way that 48% of infertile women and 23.8% of infertile men had depression and were improved after psychiatric intervention [16].
Due to the prevalence of psychological disorders in infertile patients and the negative effects of these disorders on the quality of life of these patients and the negative impact on the treatment process of these patients and given that Iran has limited studies in this field; it has been decided to do research in this field.
Materials and Methods
This clinical trial study was carried out on 62 infertile women (41 cases with PCO and 31 cases without PCO) who had depression and referred to Valiasr hospital during 2011-2012.
Inclusion criteria were infertile patients aged between 20 years-35 years old who had not been pregnant after 6 months-12 months of sexual intercourse without using contraceptive methods referred to the infertility clinic of Valiasr hospital, Tehran, Iran.
Diagnosis of PCO with ultrasound criteria (an increase of 2-5 times in the size of the ovaries and increasing the bilateral number of microcysts of 0.5 cm-0.8 cm in each ovary, so that more than 5 of these cysts are suppressed at each assumed level of imaging), clinical or laboratory hyperandrogenism (hirsutism, virilization with malepattern baldness and acne, and testosterone more than 80 ng/dl or DHEA-S more than 350 μg/dl) and oligomenorrhea [6].
Exclusion criteria were unjustifiable infertile patients, infertility with mannish causes including oligospermia or azoospermia, infertile patients with moderate to severe endometriosis, infertile patients previously treated with advanced infertility treatments such as IVF or ICSI, and patients with infertility longer than five years.
All patients fulfilled General Health Questionnaire-28 (GHQ-28) consisted of 28 4-point Likert questions. General Health Questionnaire (GHQ) is a common tool to screen and determine the problems. The original form of GHQ is consisted of 60 questions, but some forms have been shortened to 12-28 questions. The 28-item version has the high level of reliability, sensitivity and specificity compare to the other versions [17].
Those who scored at least 21, fulfilled Beck Depression Inventory (BDI-II) to check depression and patients who scored at least 17, referred to a psychiatrist to be treated with Fluoxetine 20 mg/day-60 mg/day (according to the age, weight and severity of depression of the patients) or supportive psychotherapy by 12 weeks (1-2 times per week) or combination of the both methods. To calculate the sample size, considering inclusion and exclusion criteria, all patients entered the study during 2011-2012.
Ethical consideration
This study was approved by ethic committee of Tehran University of Medical Sciences (#890).
All procedures performed in the study were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all subjects.
Statistical analysis
Data were analyzed using SPSS version 16 statistical software.
The relationship between variables was investigated using chi-square; t-test and ANOVA repeated measure. The significance level was considered less than 0.05.
Results
Mean age of the patients in the intervention and control groups was 26.55 and 26.08 years old, respectively. Duration of infertility in the intervention and control groups was 5.4 ± 2.96 years and 4.95 ± 3.66 years.
According to the results of the study, there were 14 infertile patients (45.1%) with PCO in the intervention group and 19 infertile patients (61.3%) with PCO in the control group. According to the results of the Chi-square test, there was no significant difference in the control and intervention groups regarding the cause of infertility (p=0.14) and the frequency of patients with/without PCO (p=0.09). In the intervention group, 20 infertile patients (65.4%) were pregnant after the intervention and 11 infertile patients (355%) did not become pregnant.
In the control group, only 3 infertile patients (9.7%) became pregnant after the intervention, in such a way that there was statistically significant difference between the two groups (p=0.0001). Both groups were homogeneous regarding age, education, occupation, type of infertility (primary or secondary) and history of psychology disorder (p>0.05) (Table 1).
| Variable | Control | Treatment | p-value | |||
|---|---|---|---|---|---|---|
| Frequency | Percent (%) | Frequency | Percent (%) | |||
| Age (year) | 19-25 | 18 | 58.1 | 17 | 54.8 | 0.064 |
| 30-26 | 9 | 29 | 10 | 32.3 | ||
| ≥ 31 | 4 | 12.9 | 4 | 12.9 | ||
| Occupation | Housework | 28 | 90.6 | 28 | 6/90 | 0.999 |
| Occupied | 3 | 9.7 | 3 | 7/9 | ||
| Education | Primary | 13 | 41.9 | 8 | 25.8 | 0.661 |
| High school | 8 | 25.8 | 9 | 29 | ||
| Diploma | 9 | 29 | 11 | 35.4 | ||
| >Diploma | 2 | 6.4 | 3 | 9.6 | ||
| Infertility | Primary | 24 | 77.4 | 29 | 93.5 | 0.144 |
| Secondary | 7 | 226 | 2 | 6.5 | ||
| Psychology disorder | Yes | 5 | 16.2 | 5 | 16.2 | 0.999 |
| No | 26 | 83.8 | 26 | 83.8 | ||
| Infertility duration | 1-4 | 17 | 8/54 | 17 | 8/54 | 0.445 |
| 5-9 | 12 | 38.7 | 8 | 25.8 | ||
| 9-16 | 3 | 9.6 | 6 | 19.3 | ||
| PCO | Yes | 19 | 61.2 | 14 | 45.1 | 0.309 |
| No | 12 | 38.7 | 17 | 54.8 | ||
| Pregnancy after intervention | Yes | 3 | 9.7 | 20 | 64.5 | 0.0001 |
| No | 28 | 90.3 | 11 | 35.5 | ||
Table 1: Frequency distribution of demographic characteristics of patients in the intervention and control groups
In the intervention group, 20 infertile patients were pregnant. Of these 20; 6 subjects (30%) spontaneously, 3 subjects (15%) by ART, 1 subject (5%) by LAP, 6 subjects (30%) by induction of ovulation and 4 subjects (20%) by IUI were pregnant. In the control group, 3 subjects were also pregnant (Table 2).
| Method | Control | Treatment | ||
|---|---|---|---|---|
| Frequency | Percent (%) | Frequency | Percent (%) | |
| Spontaneously | 0 | 0 | 6 | 30 |
| Art | 0 | 0 | 3 | 15 |
| Lap | 1 | 23.3 | 1 | 5 |
| Induction of ovulation | 2 | 66.7 | 6 | 30 |
| IUI | 0 | 0 | 4 | 20 |
Table 2: Frequency distribution of how to become pregnant in the intervention and control.
According to the results of independent t-test, there was a significant difference in the mean score of Beck questionnaire in the control and intervention groups before and after the intervention (p=0.0001) (Table 3).
| Variable | Control | Treatment | p-value | ||
|---|---|---|---|---|---|
| Before intervention (Mean ± SD) | After intervention (Mean ± SD) | Before intervention (Mean ± SD) | After intervention (Mean ± SD) | ||
| Beck score | 25.77 ± 7.44 | 23.87 ± 4.23 | 25.48 ± 5.79 | 13.12 ± 4.32 | 0.0001 |
Table 3: Comparison of the mean and standard deviation of Beck score in the intervention and control groups before and after the intervention
The status of beck scores was compared before and after the intervention in the both groups and indicated a change to improve depression. According to the results obtained from McNemar's test, there was a significant difference for the score changes before and after the intervention (Table 4 and Figure 1).
| Score | Point 1 | Point 2 | Point 3 | Point 4 |
|---|---|---|---|---|
| Point 1 | 0 | 2 (3.2%) | 0 | 0 |
| Point 2 | 19 (30.6%) | 12 (19.4%) | 7 (11.3%) | 0 |
| Point 3 | 9 (14.5%) | 5 (8.1%) | 0 | 6 (9.7%) |
| Point 4 | 2 (3.2%) | 0 | 0 | 0 |
| p-value | 0.0001 | |||
Table 4: Comparison of Beck score changes in the two groups before and after intervention
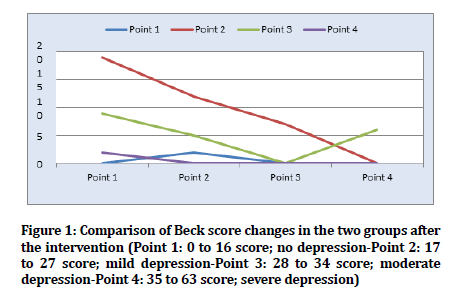
Figure 1. Comparison of Beck score changes in the two groups after the intervention (Point 1: 0 to 16 score; no depression-Point 2: 17 to 27 score; mild depression-Point 3: 28 to 34 score; moderate depression-Point 4: 35 to 63 score; severe depression)
Discussion
PCO is the most common cause of oligomenorrhea and infertility in the general population of women [15,18,19]. PCO is the most common cause of endocrine infertility in women, and it is estimated that more than 20% of women suffer from it [10]. Psychiatric problems in infertile patients include depression, aggression, anxiety, sexual dysfunction, incompatibility, lack of control and decreased self-esteem [20,21]. In this study, we investigated the effect of psychiatric interventions on depression and fertility in infertile patients with/without polycystic ovarian.
In summary the results of this study showed that the mean age and duration of infertility in the intervention and control groups was not significantly different. There was no significant difference in the control and intervention groups regarding the cause of infertility and the frequency of patients with/without PCO. In the intervention group, more than half of infertile patients became pregnant after the intervention. In the control group, only one-tenth of infertile patients became pregnant after the intervention, in such a way that there was significant difference between the two groups. Both groups were homogeneous regarding age, education, occupation, type of infertility (primary or secondary) and history of psychology disorder. There was a significant difference in the mean score of Beck questionnaire in the control and intervention groups before and after the intervention.
In a study by Klemetti et al., it was found that about 20% of women and 9% of men had infertility experiences. Infertile women had a higher risk of dysthymia and anxiety disorders than those who did not have a history of infertility. Women with a history of infertility but with a child are at risk of panic disorder. Men with a history of infertility and without childhood had a lower quality of life than men without a history of infertility and without childhood. This study concluded that the problem of infertility is related to mental health, especially dysthymia and anxiety [21]. These results were consistent with our study and in the control group the mean score of beck indicating depression of the patients were high. Another study by Deeks et al. suggested that PCO is associated with high degrees of depression that could affect the quality of life of the patient. However, there was little information about the prevalence of anxiety in these patients. In this cross-sectional and community-based study, it was found that in women with PCO, anxiety is diagnosed at higher levels than depression [22]. Indeed, in our study, we did not investigate the level of anxiety but after the intervention the mean score of beck decreased that may be correlated with anxiety and then it can reduce anxiety accordingly.
Another study by Bhattacharya et al. on PCO patients showed that women with PCO have a higher risk of depression than non-PCO women, but this study did not find evidence that high prevalence of depression in patients with PCO can be diagnosed with biochemical, clinical, and social parameters [19].
In 2009, a study was conducted by Bishop et al. on the prevalence of depression and psychological disorders and their impact on the quality of life of women with PCO. According to this study, in women with PCO, the presence of depression and related disorders often lowers the sense of being good and merits. Symptoms such as hirsutism, obesity, menstrual disorders and low fertility were the main source of psychological morbidity. The most complicated psychological problem for these patients was obesity, while other symptoms such as hirsutism and infertility were not considered as important factors in psychological problems. Although the findings appeared to be inadequate in some studies, eating disorders and a 7-fold increase in suicide rates in PCO women were observed in these studies [23].
In 2004, a study was conducted by Schmid et al. on two groups of women with PCO, a group of immigrant Muslims and the other non-Muslim Austrian women. In this study, although the typical manifestations of PCO were almost identical in both groups, it was found that the quality of life of Muslim women with PCO was significantly more than of Austrian women. Both groups were in similar situations in terms of infertility, overweight, hirsutism, menstrual disorders and emotional disorders. Among migrant Muslim women with PCO, infertility was at the top of the problem, which was due to the fact that Muslim women are more prone to childhood, and Muslim women with PCO suffer more with infertility in comparison to Austrian women with PCO [18]. In our study, demographic characteristics were homogenous in the two groups. In a study of Thomson et al. on the effect of life style to increase the quality of life and decrease depression in women with PCO, patients followed up for twenty weeks. Their intervention was diet and exercise. After the period of the study, weight loss and improvement in quality of life (except for hirsutism) and depression were observed in all groups. The study found that diet alone or in combination with exercise has a similar beneficial effect on depression and quality of life in overweight or obese women with PCO [24].
Conclusion
Finally, due to the negative impact of depression on women's quality of life and their increased fertility after psychiatric intervention, it is recommended that all infertile women should be examined for depression and treated appropriately if depression is diagnosed.
Conflict of Interest
The authors declare that there is no conflict of interest in this study.
References
- Akiskal HS, Tohen M. Bipolar psychopharmacotherapy: Caring for the patient. John Wiley & Sons 2011.
- Duniaf A. Insulin resistance and polycystic ovary syndrome: Mechanisms and implications for pathogenesis. Endocr Rev 1997; 18:774-800.
- Hasanpour DA, Abbaszadeh A, Mir S, et al. Metformin and its anti-inflammatory and anti-oxidative effects; new concepts. J Renal Inj Prev 2019; 8:54-61.
- Zawadzski JK. Diagnostic criteria for polycystic ovary syndrome: Towards a rational approach. Polycystic Ovary Syndrome, Blackwell Scientific 1992; 39-50.
- Dunaif A, Givens JR, Haseltine FP, et al. Polycystic ovary syndrome. Current issues in endocrinology and metabolism. Blackwell Scientific Publications 1992.
- van Rossum EF, Lamberts SW. Glucocorticoid resistance syndrome: A diagnostic and therapeutic approach. Best Pract Res Clin Endocrinol Metab 2006; 20:611-26.
- Legro RS, Kunselman AR, Dodson WC, et al. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: A prospective, controlled study in 254 affected women. J Clin Endocrinol Metab 1999; 84:165-9.
- Chandra A, Biersmith M, Tolouian R. Obesity and kidney protection. J Nephropathol 2014; 3: 91-7.
- Kafeshani M. Diet and immune system. Immunopathol Persa 2015; 1:e04.
- Gilling-Smith CA, Willis DS, Beard RW, et al. Hypersecretion of androstenedione by isolated thecal cells from polycystic ovaries. J Clin Endocrinol Metab 1994; 79:1158-65.
- Knobil E. The neuroendocrine control of the menstrual cycle. In Proceedings of the 1979 Laurentian hormone conference. Academic Press 1980; 53-88.
- Khazaei M. Systemic or chronic low-grade inflammation in clinical conditions. J Inj Inflamm 2016; 1:e01.
- Dehghan SF. From oxidative stress to endothelial cell dysfunction. J Prev Epidemiol 2016; 1:e04.
- Wilroy JR, Givens JR, Wiser WL, et al. Hyperthecosis: An inheritable form of polycystic ovarian disease. Birth Defects Orig Artic Ser 1975; 11:81-5.
- Cooper HE, Spellacy WN, Prem KA, et al. Hereditary factors in the Stein-Leventhal syndrome. Am J Obstet Gynecol 1968;100:371-87.
- Noorbala AA, Ramezanzadeh F, Malakafzali H, et al. Effectiveness of psychiatric interventions on depression rate in infertile couples referred to Vali-Asr. Hakim Res J 2008; 10:17-26.
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979; 9:139-45.
- Schmid J, Kirchengast S, Vytiska-Binstorfer E, et al. Infertility caused by PCOS-Health-related quality of life among Austrian and Moslem immigrant women in Austria. Hum Reprod 2004; 19:2251-7.
- Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS). Fertil Steril 2010; 94:357-9.
- Kerchner A, Lester W, Stuart SP, et al. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: A longitudinal study. Fertil Steril 2009; 91:207-12.
- Klemetti R, Raitanen J, Sihvo S, et al. Infertility, mental disorders and well-being–A nationwide survey. Acta Obstet Gynecol Scand 2010; 89:677-82.
- Deeks AA, Gibson-Helm ME, Teede HJ. Anxiety and depression in polycystic ovary syndrome: A comprehensive investigation. Fertil Steril 2010; 93:2421-3.
- Bishop S, Basch S, Futterweit W. Polycystic ovary syndrome, depression, and affective disorders. Endocr Pract 2009; 15:475-82.
- Thomson RL, Buckley JD, Lim SS, et al. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertil Steril 2010; 94:1812-6.
Author Info
Fatemeh Ramazanzadeh1, Ahmad Ali Nourbala2, Fatemeh Davari Tanha2 and Fatemeh Mostaan1*
1Department of Obstetrics and Gynecology, School of Medicine, Imam Khomeini Hospital, Tehran, Iran2Department of Psychology, School of Medicine, Imam Khomeini Hospital, Tehran, Iran
Citation: Fatemeh Ramazanzadeh, Ahmad Ali Nourbala, Fatemeh Davari Tanha, Fatemeh Mostaan, The effect of psychiatric interventions on depression and fertility in infertile patients with polycystic ovarian disease, J Res Med Dent Sci, 2019, 7(2): 187-191.
Received: 17-Apr-2019 Accepted: 26-Apr-2019
