Research - (2020) Volume 8, Issue 3
The Effect of Vitamin D on the Development and Pathophysiology of Osteoporosis: A Review
*Correspondence: Natherah Mohammad Ali, Department of Clinical Laboratory Science, College of Pharmacy, University of Baghdad, Iraq, Email:
Abstract
Osteoporosis is a metabolic bone ailment depicted by low bone thickness that extension the peril of breaks. It is a tranquil disease as there are no reactions before a break. The power of osteoporosis augments particularly with age. Osteoporosis is immovably related to supplement D status. The conviction impression of the dynamic supplement D metabolite 1,25(OH)2D is to enliven the absorption of calcium from the gut. The aftereffects of supplement D need are discretionary hyperparathyroidism and bone incident, provoking osteoporosis and splits, mineralization gives up, which may incite osteomalacia eventually, and muscle deficiency, causing falls and breaks. Supplement D supplementation may lessen bone turnover and augmentation bone mineral thickness. A couple of randomized phony treatment-controlled primers with supplement D and calcium showed a basic decrease in split recurrence. DEXA is seen as the best level technique for examination of osteoporosis. Treatment for osteoporosis should fuse lifestyle measures including sustenance, exercise and measures to diminish falls. Adequate calcium affirmation and supplement D should be given. Feasible pharmacological organization procedures should reliably be realized where significant including bisphosphonate as Alendronate, Etidronate, Risedronate, andraloxifene, strontium ranelate and teriparatide. Postmenopausal osteoporosis may be treated with a bisphosphonate. The expectation of osteoporosis should be considered in early life and should be continued by standard physical development and a sensible diet. The finding of osteoporosis is chiefly constrained by evaluating bone mineral density (BMD) using non-invasive twofold imperativeness x-bar absorptiometry. Osteoporosis drugs consolidate bisphosphonates, receptor activator of nuclear factor kappa-B ligand inhibitors, estrogen agonists/adversaries, parathyroid hormone analogues, and calcitonin.
Keywords
Osteoporosis, Supplementation, Osteomalacia, Bone mineral density (BMD)
Introduction
Osteoporosis
Osteoporosis is a dynamic central skeletal ailment depicted by diminished bone mass/thickness and little scope building rot of bone tissue. Bone game plan from the start outperforms bone resorption, anyway by the third decade this has exchanged realizing an overall deficiency of bone mass. This prompts an extended bone delicacy and frailty to split [1].
Various patients giving a split achieved by a tumble from standing stature or less are not on any kind of treatment and various patients who bolster these delicacy breaks are not started on treatment. Osteoporotic (delicacy) splits are breaks that result from mechanical forces that would not typically realize break. Osteoporotic breaks are portrayed as splits related with low bone mineral density (BMD) and consolidate spine, lower arm, hip and shoulder splits (Figure 1).
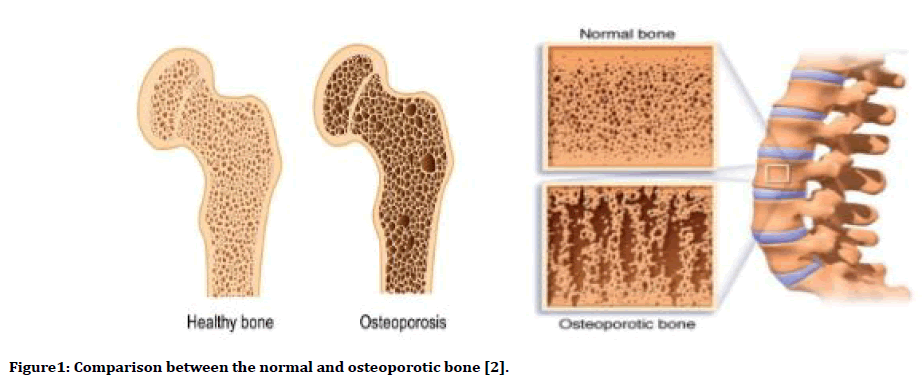
Figure 1. Comparison between the normal and osteoporotic bone [2].
The United States released a report on osteoporosis proposing that specialists get a pyramidal method to manage treatment. The base of the pyramid fuses calcium, supplement D, non-nosy treatment and fall contravention. The ensuing level requires the board or removal of helper explanations behind osteoporosis. The third level includes treatment with either threatening to resorptive or anabolic drugs. The trouble is osteoporosis is a "peaceful ailment", considering the way that there are no reactions going before a break. In any case, when an individual has broken a bone, their peril of breaking another delicacy split augmentation basically. After the fundamental break, one out of eight will break another bone inside a year and a quarter inside five years [2].
Pathophysiology
Bones offer structure to the body, security for the organs, and limit with respect to minerals, for instance, calcium and phosphorus, that are fundamental for bone improvement and quality. Individuals continue building bone and will show up at top bone mass at around 30 years of age, after which they begin to lose bone mass reliably. Regardless of the way that zenith bone mass is significantly destitute upon genetic characteristics, various modifiable parts can affect bone mass, for instance, sustenance, work out, and certain ailments just as medications [3]. All through life, bones are remodelled, suggesting that they are unendingly resorbed by osteoclasts and replaced with new bone made by osteoblasts. This strategy considers backing of mechanical quality and fix. Past the age of 40 years, resorption begins to outperform improvement by 0.3 to 0.5% consistently in the two sexes. In women around menopause, revived loss of cortical bone is superimposed on the age-related hardship. Up to 5% of trabecular bone hardship consistently and 1 to 1.5% of cortical bone mass setback occur after menopause. An anomaly in remaking activity where resorption outperforms advancement may result in the pathophysiological changes found in osteoporosis [4]. Bone includes a colossal collagenous system which is impregnated with mineral salts and populated by cells. The cross section is made from type I collagen lying in a mucopolysaccharide ground substance there furthermore humble amount of non-collagenous protein on a very basic level as proteoglycans and the bone-express proteins osteocalcin and gamma carboxyglutamic acid (GLA) protein, whose function is unknown. Gamma carboxyglutamic destructive protein is conveyed just osteoblasts and its obsession in the blood is to some degree extent of osteoplastic activity. The unmineralized matrix is known as osteoid. Bone mineral, which has for all intents and purposes a huge bit of the bone volume, occupies almost half the bone volume, consists mainly of calcium and phosphorus as crystalline hydroxyapatite. In mature bone, the proportion of calcium and phosphorus is consistent, and the molecule is enduringly bound to collagen. Bone cells are of four sorts as Osteoblasts, Osteocytes, Osteoclasts and lining cells. Hormones and growth factors have an occupation in controlling bone function. Estrogen and testosterone altogether influence bone redesigning basically by frustrating bone breakdown. Cytokines that effect remaking have furthermore been perceived, for instance, receptor activator of the nuclear factor kappa-B ligand (RANKL). RANKL is made by osteoblasts that bind to RANK receptors on osteoclasts, provoking the activation and maturation of osteoclasts and turning up at ground zero in bone resorption [3]. Late advances in nuclear bone science have perceived a solid protease named cathepsin K (CatK). CatK is produced by activated osteoclasts during the bone resorption process, achieving the defilement of bone cross section and breakdown of mineral pieces of bone tissue. Parathyroid hormone (PTH) expect a critical activity in bone improvement by in an indirect way growing the development of osteoblasts through rule of calcium homeostasis [5].
Epidemiology
Osteoporosis (Operation) has become a worldwide general medical issue that is evaluated to influence in excess of 200 million individuals around the world. The sickness influences 1 out of 3 postmenopausal ladies and 1 of every 5 men matured over 65. The predominance of osteoporosis in North Iraq was higher than that in South Iraq, and that local distinction was ascribed to contrasts in vitamin D levels. As has been accounted for, vitamin D3 blend may not be adequate to represent BMD decrease because of the absence of bright beams in high-scope locales [6]. As per a complete audit from Iraq, the predominance of osteoporosis was 12% among men, 3% among premenopausal ladies, and 19% among postmenopausal ladies, recommending a huge sexual orientation distinction. Comparable outcomes have been accounted for in the US (4.5% versus 15.4%) [6,7]. One potential purpose behind the sexual orientation contrast is that the estrogen inadequacy related with menopause or oophorectomy may prompt a quick BMD decrease in ladies, while in men, a lessening in testosterone levels may have a comparative however less articulated impact [7].
Etiology
Primary Osteoporosis
Primary osteoporosis is frequently connected with age and sex hormone inadequacy. Age-related osteoporosis results from the consistent decay of the trabeculae in bone. Likewise, the decrease of estrogen creation in postmenopausal ladies causes a noteworthy increment in bone misfortune. In men, sex-hormone – restricting globulin inactivates testosterone and estrogen as aging happens, which may add to the diminishing in BMD with time [8-10].
Secondary osteoporosis
Optional osteoporosis is brought about by a few comorbid maladies and additionally drugs. Ailments embroiled in osteoporosis frequently include mechanisms identified with the awkwardness of calcium, vitamin D, and sex hormones. For instance, Cushing's syndrome has been found to quicken bone misfortune through abundance glucocorticoid creation. Furthermore, numerous incendiary maladies, for example, rheumatoid arthritis, might necessitate the patient to be on long haul glucocorticoid treatment and have been related with auxiliary osteoporosis. Eminently, glucocorticoids are viewed as the supreme widely recognized meds connected to tranquilize actuated osteoporosis [3,8].
Risk factors of osteoporosis
Main risk factors for osteoporosis are shown in table 1 [11].
| Modifiable risks | Non modifiable risks |
|---|---|
| Alcohol | Age |
| Smoking | Female gender |
| Low body mass index | Family history (history of hip fracture) |
| Poor nutrition | Previous fracture |
| Eating disorders such as anorexia | Race/ethnicity (Caucasians and Asians) |
| Insufficient exercise | Early menopause/hysterectomy |
| Low dietary calcium intake | Long term glucocorticoid therapy |
| Vitamin D deficiency | Primary/secondary hypogonadism in men |
Table 1: Main risk factors for osteoporosis.
Clinical presentation
In a large portion of the belongings osteoporosis is asymptomatic and the condition for the most part presents simply subsequently bone crack. It is significant that clinicians be aware of perceive low injury 'delicacy breaks.' Delicacy cracks happen most ordinarily in the spine (vertebrae), hip (proximal femur), and wrist (distal range). They may likewise happen in the arm (humerus), pelvis, ribs, and different bones. Signs contrast as indicated by the crack site [12].
Vitamin D
Nutrient D is a significant enhancement in the sustenance of bone security. The crucial elements of vitamin D are the guideline of intestinal calcium retention and the incitement of bone resorption prompting the support of serum calcium focus. Wellsprings of vitamin D incorporate daylight, diet, and enhancements. Most of Americans don't accomplish satisfactory vitamin D levels. Truth be told, it is assessed that 90% of grown-ups somewhere in the range of 51 and 70 years old don't get enough vitamin D from their eating regimen. Vitamin D originates from 7-dehydrocholesterol. During presentation to sun oriented bright B (UVB) radiation, 7- dehydrocholesterol in the skin is changed over to pre nutrient D3, which is promptly changed over to vitamin D3 in a warmth subordinate procedure. Vitamin D2 and Vitamin D3 from dietary sources are joined into chylomicrons and moved by the lymphatic framework into the venous course. Vitamin D made in the skin or ingested in the eating routine can be put away and afterward discharged from fat cells. Vitamin D in the course is bound to the vitamin D-restricting protein, which transports it to the liver, where Vitamin D is changed over by Vitamin D-25-hydroxylase to 25- hydroxy Vitamin D. This type of Vitamin D is organically dormant and must be changed over to the dynamic structure it has been perceived that numerous patients with renal inadequacy show the two highlights of an insufficiency of calciferol and a protection from treatment with portions of calciferol which are physiologically powerful in ordinary people. These examinations demonstrated a nearby relationship between Vitamin D digestion and kidneys, discovered 25 hydroxy Vitamin D-1α hydroxylase in the kidney, and explained that 25 hydroxy nutrient D must be changed over in kidneys by this compound to the naturally dynamic structure – 1,25 dihydroxy nutrient D.12 1,25 dihydroxy Vitamin D can build the outflow of 25 hydroxy Vitamin D-24 hydroxylase to catabolize 1,25 dihydroxy Vitamin D to the water-solvent, organically dormant calcitroic corrosive, which is discharged in the bile [13] (Figure 2).
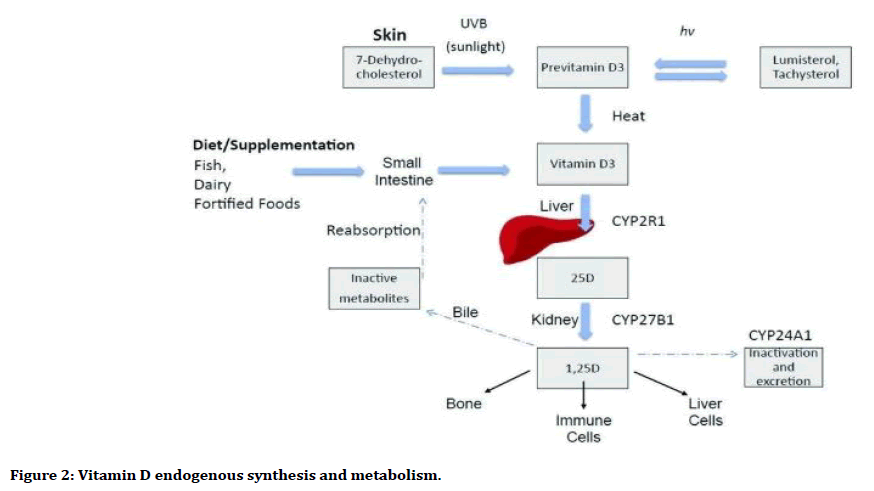
Figure 2. Vitamin D endogenous synthesis and metabolism.
Vitamin D deficiency
In vitamin D insufficiency states, diminished calcium assimilation happens from the intestines, causing expanded osteoclast creation, which improves the preparation of calcium from the bone. During times of diminished dietary admission, 1,25(OH)2D collaborates with receptors in osteoblasts, at last prompting expanded development of osteoclasts. The mature osteoclast at that point discharges enzymes to breakdown bone framework at last discharging calcium and different minerals into the dissemination. If the serum free calcium level stays low, the parathyroid organ is invigorated. Arrival of parathyroid hormone (PTH) causes expanded renal reabsorption of calcium and furthermore animates osteoclast creation, prompting expanded serum levels of calcium. On the off chance that nutrient D lack isn't amended, calcium keeps on being pulled from the bone and rickets can happen in youngsters, while osteomalacia and osteoporosis can happen in grown-ups [14]. The serum centralization of 25(OH) D3 is multiple times of that of serum 1,25(OH) D3, and this overabundance fixation comprises a storeroom like that of other steroid hormones. 25(OH)D3 is utilized by clinicians to decide vitamin D status. Vitamin D inadequacy has traditionally been characterized as flowing groupings of 25 hydroxy vitamin D [25(OH)D]<10 ng/mL [12]. However ensuing examinations have demonstrated that fixations <20 ng/mL are inadequate for blood parathyroid hormone (PTH) homeostasis. More as of late, it was suggested that healthful vitamin D lack be characterized as centralizations of coursing 25(OH)D<32 ng/mL, considering enhancement of PTH fixations, calcium assimilation, and bone mineral density [13,14].
Vitamin D and osteoporosis
Analysts have found that individuals with osteoporosis will in general have lower levels of vitamin D in their blood than individuals who don't have osteoporosis [1]. They don't have a clue whether this is on the grounds that having less vitamin D in their blood makes them bound to create osteoporosis or if having osteoporosis makes their bodies have lower levels of vitamin D for reasons unknown. Osteoporosis and age-related delicacy break fluctuate by ethnicity [14]. The metabolic capacity of bone is significant for Ca and P homoeostasis, while Ca, P and bone digestion are managed by regular components, like parathyroid hormone (PTH) and 1,25- dihydroxy vitamin D [1,25(OH)2D] [15]. Additionally, time brown complexion pigmentation with the higher melanin content squares daylight and along these lines lessens cutaneous vitamin D combination skin pigmentation ruins the change from 7- dehydrocholesterol to vitamin D. Moreover, the percentage of cutaneous 7- dehydrocholesterol is conversely connected to age and low common cholesterol levels [14]. White Caucasians have the most elevated hazard identified with osteoporosis and hip breaks when contrasted and African Americans, Chinese and Gambians although Caucasians have the most elevated admission of Ca through milk and dairy items [15]. Contrasts in social inclinations, financial status and nourishment accessibility are markers of dietary admission between ethnic groups within and between countries [11].
Diagnosis of osteoporosis
Finding of osteoporosis can be made by:
Measuring bone mineral thickness and radiotherapy to discover the bone quality
Dual vitality X-beam absorptiometry help to recognize the bone mineral thickness with absolute body structure and fat substance.
Ultrasound densitometer.
Computed tomography and fringe double vitality X-beam absorptiometry.
Resolve of erythrocyte sedimentation rate, platelet tally, protein electrophoresis, serum calcium, serum phosphorus, serum antacid phosphatase, serum creatinine and 24-hour urinary calcium discharge, to reject potential reasons for optional osteoporosis.
DXA is presently considered the highest quality level imaging strategy for the diagnosis of osteoporosis since it shows the best prescient incentive for break hazard. A gauge of break hazard might be acquired with DXA of radium, ulna, spinal segment or proximal femur [16,17]. Bone mineral thickness is accounted for as T score, Table 2. It is expressed negative term. Diagnostic criteria for osteoporosis according to WHO is following owing (Table 2) [16]. As a rule, the risk of fracture increases 1.5-3 times each standard deviation of BMD below the reference population [17].
| Interpretation | T-Score* |
|---|---|
| Normal | –1.0 and higher |
| Osteopenia | –1.0 to –2.5 |
| Osteoporosis | –2.5 and lower |
| Severe osteoporosis | –2.5 and lower with one or more fragility fractures |
Table 2: Diagnostic criteria for osteoporosis according to WHO.
Treatment
Nonpharmacological management
Nonpharmacological executives of osteoporosis incorporate enough calcium and nutrient D admission, weight-bearing activity, smoking end, confinement of liquor/caffeine utilization, and fall-anticipation methods [9,18,19]. The Institute of Medicine (IOM) suggests that dietary calcium admission ought to be 1,000 mg every day for men 50 to 70 years old and to 1,200 mg day by day for ladies 51 years old and more established and for men 71 years old and more seasoned. Supplementation with vitamin D has been appeared to improve musculoskeletal capacity and decrease the danger of falling in older ladies. Human muscle contains vitamin D receptors that may prompt expanding muscle quality and improving dependability. The blend of 700 units/day of nutrient D and 500 mg of calcium (acquired through supplementation notwithstanding diet) was appeared to lessen falls by as much as 65% more than three years in less dynamic ladies beyond 65 years old [19]. Vitamin D supplementation may expand BMD in a few areas of the skeleton, particularly in individuals who are vitamin D insufficient. The expansion of BMD might be clarified by mineralization of overabundance osteoid in cases with progressively extreme vitamin D lack and by diminishing parathyroid capacity and bone turnover which will diminish bone misfortune in the long-term. Vitamin D is a key part in calcium retention and bone wellbeing [20].
Pharmacological treatment
The goal of pharmacological therapy is to reduce the risk of fractures. Medications to treat osteoporosis are categorized as either antiresorptive (i.e., bisphosphonates, estrogen agonist/ antagonists [EAAs], estrogen, calcitonin, and denosumab) or anabolic (i.e., teriparatide). Antiresorptive medications primarily decrease the rate of bone resorption while anabolic medications increase bone formation more than bone resorption [21]. Recommendations for treatment options are based on different characteristics, such as gender, degree of fracture risk, and additional risk factors, such as comorbid diseases or medications [9].
Antiresorptive agents
Bisphosphonates
Bisphosphonates (BPs) are prescribed as the primary line meds for treatment of osteoporosis. Their consequences for bone cells are generally striking through inactivating osteoclastic bone resorption and quickening apoptosis of osteoclasts BPs can expand BMD, and abatement break hazard [22].
Drugs of this group include Alendronate, Risendronate, Ibandronate, Zoledronic corrosive, Clodronate, Minodronate, Pamidronate, Etidronate, Tiludronate. Which are diverse as far as structure, strength and liking to bone. Alendronate and risendronate are the most ordinarily utilized bisphosphonates BPs overall are alendronate and risendronate. Alendronate have longer span not just high partiality to bone. Inception of defensive enemy of break impact of alendronate is fluctuated dependent on bone destinations or if two years after treatment for vertebral bone, hip, and no vertebral bone, individually. Risendronate has a low liking to bone, and its defensive enemy of break impact is begun in any event a half year after treatment for vertebral and nonvertebral bones [22,23]. Bisphosphonates are accessible in different definitions. Alendronate, risedronate, and ibandronate are accessible as uttered medicines. Alendronate is additionally accessible as bubbly tablets and a blend definition with vitamin D. Risedronate is accessible as quick discharge or deferred discharge. Zoledronic corrosive and ibandronate are accessible as IV infusions [24]. Dosages for every operator rely on whether prophylactic or treatment portions are being prescribed [25]. Oral bisphosphonates ought to be controlled with a complete flute of water in the first part of the day on an unfilled stomach 30 minutes preceding a dinner or different prescriptions (an hour for ibandronate). Patients ought to stay upstanding for at any rate 30 minutes present portion on forestall esophageal disturbance [26].
Denosumab
Denosumab is a completely human monoclonal counter acting agent that restrains the separation and capacity of osteoclast antecedents. It has been endorsed for postmenopausal patients who are at high danger of osteoporotic breaks. There is little proof of the adequacy of denosumab against constant agony in patients with osteoporosis. Denosumab diminishes bone agony following a year of treatment [27]. Denosumab is accessible as an injectable definition in moreover a prefilled nozzle or a solitary practice ampoule. The behavior portion for osteoporosis is 60 mg subcutaneously (SC) like clockwork controlled by a social insurance proficient. Denosumab is all around endured, yet detailed unfriendly impacts incorporate excessive touchiness, genuine diseases, dermatological responses, musculoskeletal agony, and hypercholesterolemia. Denosumab can source hypocalcemia, so calcium levels ought to be remedied preceding treatment inception [28].
Estrogen agonist/antagonists
This class of medications is otherwise called estrogen receptor modulators (SERMs) has been considered for treating osteoporosis in both genders because of the unfriendly impacts of estrogen in extra-skeletal organs. SERMs contain non-steroidal engineered mixes with comparative impacts of estrogen on bone and cardiovascular framework with no unfavorable impacts of estrogen on bosom and endometrium. Raloxifene which is described as an Estrogen Agonist/Opponent (EAA), displays double agonistic and hostile assets in estrogenic pathways. Raloxifene goes about as an estrogenic agonist on the bone by diminishing bone resorption and bone turnover, along these lines expanding BMD. It likewise has estrogen hostile movement on bosom and uterine tissue [29].
Conjugated Estrogens/Bazedoxifen A blend of conjugatation estrogens with bazedoxifene got FDA endorsement in 2013 for use in postmenopausal ladies with an unblemished uterus for the avoidance of osteoporosis and for the management of moderate-toserious vasomotor indications. Duavee is occasionally alluded to as a tissue-particular estrogen complex. Bazedoxifene goes about as an EAA to lessen the danger of endometrial hyperplasia related with the estrogen segment [30].
Estrogen-progestin therapy
Regarding osteoporotic the executives, estrogen treatment is FDA affirmed exclusively for the counteraction of osteoporosis in high-chance postmenopausal ladies and ought to be utilized simply after all nonestrogenic osteoporotic medications have been viewed as improper [31]. The Women ’ s Health Initiative (WHI) was critical decrease in cracks with estrogen-progestin blend treatment; nonetheless, the WHI study information likewise announced an expansion in the danger of cardiovascular occasions, stroke, venous thromboembolism (VTE), and intrusive bosom malignant growth related with the estrogenprogestin gatherings [32].
Calcitonin
Calcitonin is a manufactured polypeptide hormone with assets like common calcitonin found in warm blooded creatures, fowls, and angle. The impacts of calcitonin on typical human bone physiology are indistinct; nonetheless, calcitonin receptors have been found osteoclasts and osteoblasts [33]. Calcitonin-salmon nasal splash is accessible just as a conventional and is controlled as one shower in one nostril every day, substituting nostrils. Miacalcin nasal shower and Fortical nasal splash. Subcutaneous infusion is accessible yet occasionally utilized. The most widely recognized unfriendly responses gotten through usage incorporate rhinitis, nasal disturbance, posterior agony, arthralgia, nosebleed, and cerebral pain [34].
Anabolic drugs
Teriparatide
Teriparatide is a human parathyroid hormone analog that animates osteoclasts to resorb bone and influences the age of osteoblasts, instigating the development of new bone. It brings down the rate of vertebral and hip cracks and has been affirmed for Osteoporosis (Operation) in patients who are at high danger of breaks. Patients with extreme Operation who were controlled teriparatide, antiresorptives (raloxifene and bisphosphonates), or both detailed fundamentally less LBP [35].
New agents
The most significant component of treating osteoporosis depends on stamped increment in BMD and crack freeperiod. The present meds have adequately decreased crack hazard and expanded BMD. Understanding the objectives of flagging pathways have served to revelation of more current operators.
At present movement being developed of fresher specialists, for example,
Cathepsin k inhibitor.
Strontium ranelate.
Romosozumb.
Blosozumab.
They are not just having expanded the accessible choices for treating osteoporosis, yet additionally have opened entryways of chance to enhancements in the powerful treatment [36].
Prevention
Enough admission of calcium is basic for support of bone thickness and working of muscles. Essential and auxiliary counteraction of osteoporosis incorporate supplementation of calcium and vitamin D. vitamin D assists with upgrading the assimilation of serum calcium in small digestive tract. Weight bearing and non-weight bearing activity are viable in osteoporosis anticipation. These activities improve the stance, equalization, exuberance and solidarity to forestall falls. For diminishing danger of spine breaks, mix practice programs were progressively successful [37,38].
Discussion
Bone loss and osteoporosis with the resultant increase in fracture risk should be major concerns for patients and health care providers. As the population ages, the longterm effects of osteoporosis including pain, loss of independence and institutionalized care will become more prevalent. Efforts to prevent bone loss and osteoporosis should start with proper education about a healthy lifestyle, including optimal calcium and vitamin D and exercise in adolescence. Many sources agree to use vitamin D and calcium supplementation in osteoporosis supplements are available that can supply the body with amounts necessary for bone health. The relationship between vitamin D and BMD in osteoporosis is very important, use vitamin D increase BMD and reduce risk of fracture and osteoporosis [3,4].
The combination of 700 units/ day of vitamin D and 500 mg of calcium obtained through supplementation in addition to diet was shown to reduce falls by as much as 65% over three years in less active women over the age of 65 [19].
Other sources that disagree with depending on vitamin D and calcium only considered as complementary with treatment and must use real treatment for osteoporosis such as Antiresorptive Agents and Anabolic drugs. These drugs are used in more cases of osteoporosis. Their effects on bone cells are most notable through inactivating osteoclastic bone resorption and accelerating apoptosis of osteoclasts BPs can increase BMD and decrease fracture risk [21].
Conclusion
We can infer that osteoporosis is an overall anxiety, initiating supplementary than 8.9 million breaks for every year. The normal increment in clinical appointments, hospitalizations, and cherishing homebased arrangements identified with osteoporotic breaks will add to a generous financial weight on medicinal services frameworks. Along these lines, screening is significant dependent on age, sexual orientation, and other hazard factors. Nutrient D and calcium are significant in the mechanical and basic honesty of the skeleton. Subclinical nutrient D lack (nutrient D inadequacy) is basic in the fit, dynamic old populace and prompts an intensification old enough related bone turnover, bone misfortune and subsequently expanded danger of crack. Bisphosphonates remain the principal line and most practical treatment choice for osteoporosis, yet there is expanding worry about their long-haul security. Prescriptions with novel systems to treat osteoporosis can be normal sooner rather than later. Albeit suitable BMD screening and treatment with medicine is significant, osteoporosis is preventable with appropriate administration of diet, way of life, and fall avoidance intercessions.
References
- http://www.laalamedilla.org/GUIAS/Guia%20NICE%20osteoporosis%20P2%202011.pdf
- https://www.nice.org.uk/guidance/cg146
- https://www.bones.nih.gov/health-info/bone/SGR/surgeon-generals-report
- Raisz LG. Pathogenesis of osteoporosis: Concepts, conflicts, and prospects. J Clin Invest 2005; 115:3318–3325.
- Das S, Crockett J. Osteoporosis: A current view of pharmacological prevention and treatment. Drug Des Devel Ther 2013; 7:435–448.
- McGuire S. Institute of Medicine. 2009. School meals: Building blocks for healthy children. Washington, DC: The national academies press. Adv Nutr 2011; 2:64–65.
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 2014; 29:2520–2526.
- Hunter DJ, Sambrook PN. Bone loss: Epidemiology of bone loss. Arthritis Res 2000; 2:441–445.
- Buckley L, Guyatt G, Fink HA, et al. American college of rheumatology guideline for the prevention and treatment of glucocorticoid- induced osteoporosis. Arthritis Care Res 2017; 69:10951110.
- Maeda SS, Lazaretti-Castro M. An overview on the treatment of postmenopausal osteoporosis. Arg Bras Endocrinol Meta 2014; 58:161-171.
- https://www.nice.org.uk/guidance/ta160/documents/osteoporosis-primary-prevention-appraisal-consultation-document2
- https://www.nice.org.uk/guidance/cg146/documents/osteoporosis-fragility-fracture-risk-nice-guideline2
- Holick MF, Garabedian M. Vitamin D: Photobiology, metabolism, mechanism of action, and clinical applications. In: Favus MJ, Primer on the metabolic bone diseases and disorders of mineral metabolism, 6th Edn 2006; 129–37.
- Holick MF. 2008b. Vitamin D: Important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J 2008; 98:1024–1027.
- Libon F, Cavalier E, Nikkels AF. Skin color is relevant to vitamin D synthesis. Dermatology 2013; 227:250-254.
- Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int 2005; 16:3-7.
- Guglielmi G, Scalzo G. Imaging tools transform diagnosis of osteoporosis. Diagnostic Imaging Europe 2010; 26:7-11.
- Das S, Crockett J. Osteoporosis: A current view of pharmacological prevention and treatment. Drug Des Devel Ther 2013; 7:435–448.
- https://consensus.nih.gov/2000/2000osteoporosis111html.htm
- Holick MF. High prevalence of vitamin D inadequancy and implications for health. Mayo Clin Proc 2006; 81:353-73.
- Cosman F, de Beur S, LeBoff M, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 2014; 25:2359– 2381.
- Simon JA. Are all bisphosphonates the same? Potential reasons for clinical differences: A perspective. J Womens Health 2010; 19:719–27.
- Kanis JA, McCloskey EV, Johansson H, et al. Scientific advisory board of the european society for clinical and economic aspects of osteoporosis and osteoarthritis (ESCEO) and the committee of scientific advisors of the international osteoporosis foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 2013; 24:23–57.
- Camacho PM, Petak SM, Binkley N, et al. American association of clinical endocrinologists and american college of endocrinology: clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2016. Endocr Pract 2016; 22:S1–S42.
- https://www.gene.com/medical-professionals/medicines/boniva-tablets
- https://www.merck.com/product/usa/pi_circulars/f/fosamax/fosamax_pi.pdf
- Cummings SR, San Martin J, McClung MR, et al. Freedom trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 2009; 361:756–765.
- https://www.pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/prolia/prolia_pi.pdf
- https://pi.lilly.com/us/evista-pi.pdf
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022247s002lbl.pdf
- http://labeling.pfizer.com/showlabeling.aspx?id=131
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the women’s health initiative randomized controlled trial. JAMA 2002; 288:321–333.
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021406s008lbl.pdf
- https://www.fda.gov/drugs/drug-safety-and-availability
- Devogelaer JP, Boutsen Y, Manicourt DH. Biologicals in osteoporosis: Teriparatide and parathyroid hormone in women and men. Curr Osteoporos Rep 2010; 8:154–161.
- Pacheco-Costa R, Han SW, Pochini AC, et al. Gene therapy for osteoporosis. Acta Ortop Bras 2011; 19:52.
- Tobon GJ, Izquierdo JH, Canas CA (2013) B lymphocytes: Development, tolerance, and their role in autoimmunity-focus on systemic lupus erythematosus. Autoimmune Dis 2013; 2013:827254.
- National osteoporosis foundation. Clinician’s guide to prevention and treatment of osteoporosis. Washington, DC. National Osteoporosis Foundation 2010; 1-56.
Author Info
Department of Clinical Laboratory Science, College of Pharmacy, University of Baghdad, IraqCitation: Natherah Mohammad Ali, The Effect of Vitamin D on the Development and Pathophysiology of Osteoporosis: A Review, J Res Med Dent Sci, 2020, 8(3): 65-72
Received: 10-Apr-2020 Accepted: 28-Apr-2020
