Research Article - (2019) Volume 7, Issue 2
The Impact of Increased Body Mass Index on the Incidence and Severity of Post-spinal Headache after Cesarean Section
Masoud Hashemi1, Seyed Hedayatollah Akhlagh2, Sahar Hashemi Shadegan2, Mehrdad Taheri1, Arash Farbood2, Payman Dadkhah1 and Saman Asadi2*
*Correspondence: Saman Asadi, Department of Anesthesiology, School of Medicine, Shiraz University of Medical Sciences, Iran, Email:
Abstract
Background: Previous studies have been controversial as to the relationship between post-dural puncture headache (PDPH) and body mass index (BMI) in parturient patients. Therefore, we decided to survey this complication in a group of patients whose pregnancies were terminated by cesarean-section under spinal anesthesia. It was hypothesized that patients with higher BMI will have lower incidence of PDPH.
Material and Method: After studying the patients' files and calling them, the demographic information was extracted and recorded. Also, development of PDPH up to three days after cesarean-section in the current delivery and headache score based on 0-10 verbal numeric rating scale (NRS) were documented.
Results: In the current study, 343 parturient patients were analyzed; 164 (47.8%) women were non-obese and the rest (52.2%) were obese (BMI above 30 kg/m2). 91% of the patients had not any past history of PDPH in the previous neuroaxial anesthesia/analgesia. Only 59 patients (17.2%) developed headache after current spinal anesthesia. There was a reverse and significant relationship between pre-cesarean BMI and the post-spinal headache (p-value: 0.016).
Conclusion: The incidence of PDPH was reduced by increased BMI at the time of cesarean-section. In obese patients, the higher intra-abdominal pressure decreases the leakage of CSF from the dural puncture point; thus, by increasing the BMI, the incidence of PDPH is decreased. This study also showed that the severity of PDPH did not significantly change with BMI, weight gain during pregnancy or any other analyzed factors.
Keywords
Headache, Spinal anesthesia, Cesarean section, Body mass index
Introduction
According to the increased risk of general anesthesia and its higher mortality rate in the cesarean section (C/S), spinal anesthesia is still the golden option for C/S. In this anesthetic procedure, post-dural puncture headache (PDPH) is one of the most prevalent side effects of this sedation technique in about 25% of patients [1]. In a casecontrol study, Webb et al. showed that the incidence of chronic headache in pregnant women after accidental dural puncture with a Touhy-needle gauge 17 was 28%. These women had also back pain [2].
PDPH can be one of the causes of maternity problems. In addition to disrupting the mother's capability to care the baby, medical management of this side effect can also increase the cost of health care and the duration of hospitalization [3]. There are contradictory ideas about the effect of body mass index (BMI) on the incidence of PDPH. Some studies protect the conventional idea about the effect of Body Mass Index on the Post-dural Puncture Headache; the lower BMI is a risk factor for PDPH [4,5]. In contrast, some other researchers do not believe in this idea [6,7]. In neuro-axial anesthesia, changes in epidural/ interstitial spaces of obese patients may be the cause of less PDPH in these patients. There is some evidence about the higher epidural pressure in the obese patients compared to the lean ones, which could cause less leakage of cerebrospinal fluid (CSF) through the dura-membrane and so less PDPH [8]. On the other hand, according to some results, patients with BMI ≥ 30 kg/m2 need less epidural analgesic dose rather than those with BMI<30 kg/m2 which could be justified by the higher CSF-pressure [9]. In Faure et al. study, the incidence of PDPH in patients with BMI<30 kg/m2 was 45% and in those with BMI ≥ 30 kg/m2 it was reported 24% (p<0.05) [10], some other studies have confirmed this finding.
A study by Birajdar et al. on the occurrence of PDPH in women with cesarean section under spinal anesthesia with different body mass indexes showed that the incidence of PDPH was less in women with BMI>30 kg/m2 compared with those with BMI<30 kg/m2 [11]. In a retrospective study of prospective follow up of more than 18000 pregnant women with unintentional durapuncture from 2007 to 2012, Miu et al. compared the rate and also severity of headache. They found no significant different results between parturient with BMI below or above 30 kg/m2 [6]. In a more recent study by Song et al., the impact of upper BMI on the decrease in the risk of PDPH was evaluated and compared to the non-obese pregnant patients. They discovered not any substantial distinct findings [3]. Therefore, we decided to survey the incidence and severity of positional headache in pregnant patients having undergone spinal anesthesia for cesarean section and assess the effect of higher BMI as a preventing factor. Our hypothesis was that patients with higher BMI have lower incidence of PDPH.
Materials and Methods
This retrospective cross-sectional study, was approved by Ethical Committee of Shiraz University of Medical Sciences (Ethical Committee No. 97-01-01-17133) at 2018 July 21. A written informed consent was obtained from the parents who accepted to participate in this study. In this study, we studied the files of elective cesarean section candidates, referred to Hafez Hospital in Shiraz during three months (April, May and June 2018).
Inclusion criteria were age of 17 years-50 years old, American Society of Anesthesiologists (ASA) class I and II, receiving spinal anesthesia with the first try using 25- G Quincke needles (Becton Dickinson, Spain), use of intrathecal bupivacaine+fentanyl without preservative substance for spinal anesthesia, and elective Cesarean/ Section. All patients were evaluated by an anaesthesiologist preoperatively and the history of headache was recorded.
Exclusion criteria were twin or multiple pregnancy, gestational diabetes, preeclampsia, eclampsia or HELLP syndromes, history of migraine or other types of headache, psychiatric diseases and change in the anesthesia plan to general anesthesia during surgery.
After studying the files of 876 cases of cesarean/section, 343 subjects were matched with the inclusion and exclusion criteria and also were available and cooperative to answer the questionnaire. Their following information was extracted and recorded in a checklist including age, gravid number, history of smoking, height, last weight before pregnancy, weight gain during pregnancy, pre-cesarean weight and BMI, history of PDPH in previous neuroaxial technique, having PDPH up to three days after delivery in the current spinal method of anesthesia, PDPH start date, headache score based on 0-10 verbal numeric rating scale (NRS), and the need for treatment with epidural blood patch, supportive treatments such as hydration, analgesics or other selfhealing treatment. To validate the early and secondary data, a sensitivity analysis was conducted by a cutoff value of 30 kg/m2, which is accepted as the threshold value defining obesity by the World Health Organization (WHO).
In parallel, patients were divided into 2 groups: based on adult obesity and BMI, calculated in the database using their weight at the time of the procedure: Group 1: Nonobese Patients (BMI<30 kg/m2, Group<30); Group 2: Obese patients (BMI ≥ 30 kg/m2, Group ≥ 30). And a subgroup of sickly obese patients (BMI>40 kg/m2), were compared with non-obese women. The sample size was calculated at least 300 patients, using a similar study [6] with a=0.05 and power=80%. This number provides power of 0.58, 0.78, 0.92, 0.98, and 0.99 for detecting a difference in PDPH of 10% to 20% in 2.5% increments between BMI groups at α of 0.05. A Fisher exact test was used for sample size analysis. Calculations were performed using PASS 11 (version 11.0.10, NCSS, LLC, Kaysville, UT). Furthermore, severity of PDPH was assessed using a visual analogue scale (VAS) extending from 0-10; 0=no headache, 1-3=mild headache, 4-7=moderate headache, >7=severe headache. The primary outcome of this study was presence of PDPH.
Secondary outcomes included association of the incidence and severity of PDPH with the height, smoking, and weight gain during pregnancy, the last weight before pregnancy, and the last weight and BMI before cesareansection. In fact, in this study, the BMI differentiation of patients as obese and lean was determined, and in the next stage, the incidence of PDPH in these patients was examined (Figure 1).
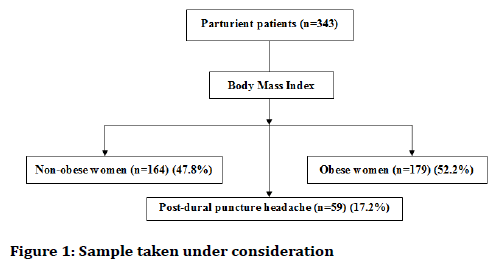
Figure 1. Sample taken under consideration
Statistical analysis
All statistical analysis was conducted using SPSS, version 22 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to describe outcomes for BMI groups with between-group comparisons using chi-square or Fisher exact tests. In addition, Mann Whitney test and Spearman correlation test were used to evaluate the incidence and severity of PDPH with BMI and other probably effective factors.
A p-value<0.05 was considered statistically significant.
Results
This study was performed on 343 women who had undergone cesarean section under spinal anesthesia in Hafez Hospital, Shiraz, Iran in a three-month period (March, April and May 2018). The age of the subjects was between 17 years and 47 years old (30.44 ± 5.90). The parturient patients were between gravid 1-8: 91 (26.5%) gravid 1, 133 (38.8%) gravid 2, 61 (17.8%) gravid 3, 35 (10.2%) gravid 4, 10 (2.9%) gravid 5, 8 (2.3%) gravid 6, 4 (1.2%) gravid 7 and 1 (0.3%) gravid 8.
The Tables 1 and 2 show the clinical and quantitative data of the study population.
| Variable | Minimum | Maximum | Mean | Std. deviation |
|---|---|---|---|---|
| Weight before pregnancy (kg) | 40 | 122 | 63.53 | 11.08 |
| Last weight before cesarean/section (kg) | 52 | 135 | 77.97 | 11.65 |
| Weight gain (kg) | 0 | 33 | 14.44 | 5.8 |
| Body Mass Index (BMI) before cesarean/section (kg/m2) | 23 | 47 | 30.54 | 3.66 |
| Height (cm) | 140 | 180 | 159.59 | 5.85 |
Table 1: The status of the population studied in terms of clinical variables
| Variable | Frequency (%) | |
|---|---|---|
| Smoking | Yes | 5 (1.5%) |
| No | 338 (98.5%) | |
| Past history of PDPH | Yes | 31 (9%) |
| No | 312 (91%) | |
Table 2: The frequency of smoking and past history of post-dural puncture headache in parturient patients
From the 343 parturient patients, 164 (47.8%) women were non-obese and the rest (52.2%) were obese (BMI above 30 kg/m2); 98.5% of them were non-smoker and 91% had not any past history of PDPH in the previous neuro-axial anesthesia/analgesia. In this study, only 59 patients (17.2%) developed headache after the current spinal anesthesia; most of them [28 women] had a headache on the second day after the intrathecal technique.
According to Table 3, there was a significant relationship between pre-cesarean BMI and post-dural puncture headache (PDPH) [p=0.016]; the most incidence of PDPH was observed in the body mass index less than 30 kg/m2.
| Variable | Incidence of post-spinal headache (%) | Result (p-value) | ||
|---|---|---|---|---|
| no | yes | |||
| Pre-cesarean | ≤ 30 | 126 (76.8%) | 38 (23.2%) | - |
| Body Mass Index (kg/m2) | 30-40 | 153 (87.9%) | 21 (12.1%) | 0.016 |
| >40 | 5 (100%) | 0 (0%) | ||
| Past history of PDPH | Yes | 17 (54.8%) | 14 (45.2%) | <0.001 |
| No | 267 (85.6%) | 45 (14.4%) | ||
Table 3: The relationship of pre-cesarean body mass index (BMI) and history of previous PDPH with the incidence of post-spinal headache
Also, there was a statistically significant relationship between the past history of PDPH in the previous procedures and the subsequent headache (p<0.001); that is, 17 (54.8%) of the patients who had previous history of PDPH in the previous cesarean-sections or other procedures, developed PDPH.
As displayed in Table 4, there was a significant relationship between pre-cesarean weight and also the amount of weight gain during pregnancy period and the incidence of post-dural puncture headache (p-value: respectively 0.006 and 0.002). That is, with the increase in pregnancy weight gain and pre-cesarean weight, the incidence of headache will decrease.
| Variable | Incidence of post-spinal headache | Result (p-value) | |
|---|---|---|---|
| yes | no | ||
| Pre-cesarean Weight (kg) [mean ± std. deviation] | 78.76 ± 11.77 | 74.20 ± 10.32 | 0.006 |
| Weight gain during pregnancy (kg) [mean ± std. deviation] | 14.87 ± 5.81 | 12.36 ± 5.34 | 0.002 |
Table 4: The relation of pre-cesarean weight (kg) and weight gain during pregnancy (kg) with the incidence of post-spinal headache
According to this study, there was not any significant relationship between post-spinal headache incidence with age (p-value: 0.320), gravid number (p-value: 0.591), pre-pregnancy weight (p-value: 0.199), height (pvalue: 0.753), and history of smoking (p-value: 0.592).
The severity of headache (Numerical Rating Scale as pain score in the group of parturient patients with post-spinal headache) had not any statistical correlation with age (pvalue: 0.145), gravid number (p-value: 0.918), height (pvalue: 0.167), past history of post-dural puncture headache (p-value: 0.668), pre-pregnancy weight (pvalue: 0.087), weight gain during pregnancy (p-value: 0.620), pre-cesarean weight (p-value: 0.116), and precesarean Body Mass Index (p-value: 0.703).
Discussion
The present study showed that most headache cases occurred in patients with BMI<30 (p=0.016), but the NRS in the parturient women with different BMI levels did not have any significant difference (p=0.703). Thus the higher the BMI at the time of cesarean-section, the less is the incidence (but not severity) of PDPH after cesareansection under spinal anesthesia. In parallel, there are a number of similarities among our study population and other studies that showed a lower incidence of PDPH [10,12-15] which may account for our findings to find an effect of BMI on outcome. These include similarity in BMI demographics and dural puncture with the same needles. Previous studies [10,12,14,15] that noted lower rates of PDPH as BMI increased were conducted after spinal anaesthesia. But, in contrast with these findings, in a study by Miu et al. [6] which assessed the association between body mass index and PDPH in patients with cesarean section did not show that patients with high body mass index were less likely to have PDPH.6, while our study, unlike that of Miu et al. [6], confirmed this idea.
In addition, our findings on the relationship of BMI with PDPH after dural puncture are consistent with the findings of Peralta et al., which reported that the relationship between BMI and PDPH in women with cesarean section by spinal method, showing that the prevalence of PDPH in patients with higher BMI was reduced [4]. The results of this study confirm our findings.
Our study also showed that the severity of headache after the spinal anesthesia (numerical rating scale in cases who had headache related to dural puncture) did not changed with patients’ age, gravid number, height, weight before pregnancy, weight gain during the pregnancy period, pre-cesarean weight, and BMI (p-value>0.05). Also, in patients with the past history of PDPH, the severity of post-spinal headache was not significantly greater than the others (p-value: 0.668). According to the results of the present study, it is suggested that spinal technique should be used as the anesthesia method in lean pregnant women (BMI less than 30 kg/m2) with more precautions because these people are considered to be in higher risk of PDPH. It seems that the presumptive cause of the decrease in PDPH rate in obese patients is that the increase in BMI leads to the higher intraabdominal pressure which decreases the CSF leakage from the hole of the dura at the site of needle entrance. In parallel, Hogan et al. suggested that intraabdominal pressure increases linearly with body weight and found a decrease in CSF volume with external abdominal compression that may simulate a static increase in abdominal pressure similar to that found in pregnancy [16]. Moreover, the same investigators recommended that the mechanism involves “inward movement of soft tissue in the intervertebral foramen”. Increased abdominal pressure in the obese parturient may also enhance pregnancy-induced epidural venous engorgement, resulting in a decrease in the volume of CSF in the lumbar neuraxial canal [17].
Limitations
Limitations in this study are the presence of a small number of patients with BMI more than 40 kg/m2. It is preferable to design a larger cohort study to reveal all occult points of PDPH. Furthermore, despite the large number of topics in this study, our sample was insufficient to examine the association between PDPH and BMI with a high level of confidence. So the comparison may be more appropriate if done on a nonpregnant population indicated for spinal anesthesia
Conclusion
Taken together, our data confirm the previously reported association between high BMI and reduced likelihood of a PDPH, and there was not any statistical relationship between the patients’ characteristics such as height, weight and BMI. Although the incidence of a PDPH was lower in subjects with high BMI, the severity and need for treatment of a PDPH were not influenced by body weight. It is recommended that further studies should be conducted about the effective factors on the severity of post-spinal headache in larger sample sizes.
Acknowledgments
The present article was extracted from the thesis written by Sahar Hashemi Shadegan M.D. and was financially supported by Shiraz University of Medical Sciences grants No. 97-01-01-17133. The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Gosch U, Hueppe M, Hallschmid M, et al. Post-dural puncture headache in young adults: Comparison of two small-gauge spinal catheters with different needle design. Br J Anaesth 2005; 94:657-61.
- Webb CAJ, Weyker PD, Zhang L, et al. Unintentional dural puncture with a tuohy needle increases risk of chronic headache. Anesth Analg 2012; 115:124-32.
- Song J, Zhang T, Choy A, et al. Impact of obesity on post-dural puncture headache. Int J Obstet Anesth 2017; 30:5-9.
- Peralta F, Higgins N, Lange E, et al. The relationship of body mass index with the incidence of postdural puncture headache in parturients. Anesth Analg 2015; 121:451-6.
- Kwak KH. Postdural puncture headache. Korean J Anesthesiol 2017; 70:136-43.
- Miu M, Paech M, Nathan E. The relationship between body mass index and post-dural puncture headache in obstetric patients. Int J Obstet Anesth 2014; 23:371-5.
- Angle P, Thompson D, Szalai JP, et al. Expectant management of postdural puncture headache increases hospital length of stay and emergency room visits. Can J Anaesth 2005; 52:397.
- Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults. 2008. JAMA 2010; 303:235-41.
- Panni MK, Columb MO. Obese parturients have lower epidural local anaesthetic requirements for analgesia in labour. Br J Anaesth 2006; 96:106-10.
- Faure E, Moreno R, Thisted R. Incidence of postdural puncture headache in morbidly obese parturients. Reg Anesth 1994; 19:361.
- Birajdar SB, Allolli DN, Javed M. Study of incidence of postdural puncture headache (pdph) in pregnant women with different body mass index undergoing caesarean section under spinal anaesthesia. Indian J Clin Anaesth 2016; 3:443-5.
- Brown RS, Johnson MD, Zavisca R, et al. Morbid obesity in the parturient reduces the risk of post dural puncture headache (PDPH) after large bore continuous spinal anesthesia. Anesth 1993; 79:A1004.
- Bell ED. Decreased incidence of post dural puncture headache in morbidly obese parturients following continuous spinal using 17 gauge Tuohy needle. Anesth 1997; 87:A886
- Peralta F, Higgins N, Chalifoux LA, et al. Obese parturients and the incidence of postdural puncture headache after unintentional dural puncture. SOAP Abstracts 2010:6.
- Spielman FJ, Mayer DC, Criswell HE. The relationship between body mass index and postdural headache in parturients. Anesth 2003; 98:A99.
- Hogan QH, Prost R, Kulier A, et al. Magnetic resonance imaging of cerebrospinal fluid volume and the influence of body habitus and abdominal pressure. Anesth 1996; 84:1341-9.
- Hirabayashi Y, Shimizu R, Fukuda H, et al. Soft tissue anatomy within the vertebral canal in pregnant women. Br J Anaesth 1996; 77:153-6.
Author Info
Masoud Hashemi1, Seyed Hedayatollah Akhlagh2, Sahar Hashemi Shadegan2, Mehrdad Taheri1, Arash Farbood2, Payman Dadkhah1 and Saman Asadi2*
1Anesthesiology Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran2Department of Anesthesiology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
Citation: Masoud Hashemi, Seyed Hedayatollah Akhlagh, Sahar Hashemi Shadegan, Mehrdad Taheri, Arash Farbood, Payman Dadkhah, Saman Asadi, The impact of increased body mass index on the incidence and severity of post-spinal headache after cesarean section, J Res Med Dent Sci, 2019, 7(2): 1-5.
Received: 22-Feb-2019 Accepted: 01-Mar-2019 Published: 30-Mar-2019
