Research - (2021) Volume 9, Issue 6
The Outcomes of the Lag-Screw Use for Treatment of the Mandibular Symphysis, Parasymphysis and Oblique Body Fractures
Hani Tareq Abd-Alwahab1* and Thair A Lateef Hassan2
*Correspondence: Hani Tareq Abd-Alwahab, Senior Resident Maxillofacial Surgery, Iraqi Board for Medical Specialization, Iraq, Email:
Abstract
Background: For most fractures of the mandible, the aim of treatment is primarily to restore function, the occlusion, and pain-free normal movements of both temporomandibular joints. One of the methods of open reduction and fixation is Lag screw. The concept of Lag Screw osteosynthesis is defined as the stable union of two bone fragments under pressure with the aid of screws which in turn are under tension. The lag screw technique was first introduced to Maxillofacial Surgery by Brons and Boering in 1970 who cautioned that at least two screws are necessary to prevent rotational movements of the fragments in mandibular body fractures.
Aims: The study is aimed to assess the post-operative results by assessing the primary stability and the need for any supplemental maxillomandibular fixation (MMF), measure the time required to complete the procedures and evaluate the incidence of post-operative complications.
Materials and Methods: This was a prospective clinical study conducted from December 2017 to December 2018. The sample included patients who attended the Department of Oral & Maxillofacial Surgery / Ghazi Al-Hariri Teaching Hospital /Medical City /Baghdad subjected to maxillofacial trauma with mandibular fractures (symphyseal, parasymphyseal region and oblique body). Patients above the age of 14 years until 50 years. A total of 10 patients fulfilled the inclusion criteria participated in this study. Those patients were treated with the use of lag screws.
Results: Study patients’ age was ranging from 14-50 years with a mean 24.2 years. Regarding gender, the proportion of males was higher than females with a male to female ratio of 4:1. Parasymphyseal and oblique body fracture were the most common sites of fracture (40% for each). Mobility was absent in 60% of them intraoperatively, while it was 80% after one month. After six months, all study patients did not show any mobility. Occlusion was corrected in 90% of them intraoperatively. No displacement observed in 90% of them intraoperatively. It had been noticed that 60% of patients did not complain from any intraoperative complications, while fracture of drill and incorrect screw position were occurred in 20% of patients. It had been noticed that the mean of duration of operation was significantly higher in operation by extraoral approach than that by intra-oral approach.
Conclusion: Lag screw technique can achieve good stability and appropriate compression. The technique needs proper case selection and careful instrumentation. Two lag screws better to be used wherever possible. Excellent rigidity achieved by the lag screw fixation. Optimal stability of treated fractures by lag screws is obtained in all cases.
Keywords
Lag screw, Parasymphysis, Mandibular symphysis
Introduction
The maxillofacial skeleton injuries occur due to a variety of causes, such as road traffic accidents and sports injuries. According to the medical literature, traffic accidents have been the leading cause of mandibular fractures; however, this trend has been changing in recent years and the primary etiological agent today is interpersonal aggression. However, Gray et al. [1] have determined that the etiology of injuries in general is heavily influenced by socioeconomic and cultural factors. The etiological agent can produce a mandibular fracture from a direct mechanism in which the fracture line occurs at the site of the injury or an indirect mechanism when the force transmission breaks the mandible at its weakest points: the condyle, mentonian hole and edentulous zones [2].
The mandible is the second most fractured bone of the maxillofacial skeleton because of its position and prominence. Although there is wide variance in the reported percentage of fracture of the anterior mandible (symphysis and parasymphysis), aggregate analysis places this at approximately 17% of all mandibular fractures. Although there is a widely accepted consensus about the need for surgical reduction and fixation of a mandibular fracture, a variety of different treatment modalities have been described. Among them are closed or open reduction, extra oral open reduction and internal fixation with a reconstruction plate, intraoral open reduction and internal fixation using different minidynamic compression or non-compression plates and an intraoral approach with lag-screw fixation. Miniplate osteosynthesis was introduced to maxillofacial surgery by Michelet et al. [3]. Miniplate osteosynthesis has caused a revolution in mandibular fracture treatment. One of the most practical methods for open reduction internal fixation of mandibular fractures is the use of lag screw fixation for approximation and stabilization of the fracture segments. The lag screw technique in maxillofacial surgery was first advocated by previous authors who stated that at least two screws were necessary to prevent rotational movement of the fragments in oblique fractures of the mandible. In North America, its use for the management of anterior mandible fractures became popular through the work of Ellis et al. [4]. Lag screw fixation is based on the concept of osteosynthesis by bone compression [5].
Fixation systems with semi-rigid plates are well known and have been widely used by maxillofacial surgeons since they were first described by Agnihotti et al. given the difficulty inherent in molding the reconstruction plates used in traditional techniques to adapt them to the mandible and not the other way around, as the rigidity of the plate can cause malocclusion [6].
For that reason, rigid plates have become relegated to specific cases like multiple fractures, edentulous patients, bone graft fixation, reconstructive surgery, and salvage surgery for non-consolidated fractures treated with other systems. In 2008, Madsen et al. demonstrated that the lag screw technique is the best internal fixation system, based on a study of biomechanical measurements on acrylic mandibles comparing lag screws with other fixation systems [7].
Materials and Methods
Study design
This was a prospective clinical study conducted from December 2017 to December 2018. The sample included patients who attended the Department of Oral & Maxillofacial Surgery/Ghazi Al-Hariri Teaching Hospital/ Medical City/Baghdad subjected to maxillofacial trauma with mandibular fractures (symphyseal, parasymphyseal region and oblique fracture of the body). A total of 10 patients fulfilled the inclusion criteria participated in this study. Those patients were treated with the use of lag screws. A detailed history with thorough clinical and radiographic examinations were done and the findings were recorded in special forma. The patient signed on this special forma for the participation in this research. The study was approved by the Ethical Committee in the Council of Maxillofacial Surgery.
Inclusion criteria
• Patients with symphyseal, parasymphyseal and oblique body fractures of mandible.
• Patients above the age of 14 years old until 50 years old.
Exclusion criteria
• Comminuted fractures of the mandible and fractures with gap defects.
• Patients with preexisting infection at fracture site.
• Completely edentulous patients.
• Immunocompromised patients and Patients with other systemic conditions contraindicated for surgery under G.A. (such as patients with advanced heart failure or severe respiratory compromised patients).
Instruments and equipment
• Surgical set.
• 2. Lag Screws set. 2 mm diameter and different lengths (15, 17, 20, 21, 25, 29, 35, 39 mm), Figure 1A and 1B).

Figure 1. Surgical training questionnaire
• Lag screw application set Figure 2.

Figure 2. Surgical training questionnaire
• Small round bur to make a depression in the near cortex.
• Drill bit 2mm.
• Depth gauge.
• Erich arch bar.
• Stainless steel wire for inter maxillary fixation (0.5 mm).
• Micromotor hand piece.
• Engine motor.
Medications
• Local anesthesia, 2.2 mL cartridge of lidocaine hydrochloride 2% with adrenalin 1:80000, (ligospane special, septodont, France).
• 0.2 % chlorhexidine mouthwash.
• Ceftriaxone vial 1g I.V.
• Diclofenac ampule 75mg I.M.
• Dexamethasone ampoule 8 mg I.M.
• Amoxicillin / Clavulanate potassium capsule 625 mg oral.
• Metronidazole tablets 500 mg oral or vial 500 mg I.V.
• Povidone iodine solution 10%.
The diagnosis was based on clinical and radiographical examination.
Clinical examination: All the required information about the patient and detailed previous medical history were taken from each patient by a special form of a case sheet designed for this study (Appendix).
Extra-oral: The patients were examined for the presence of ecchymosis, swelling, soft tissue laceration, deformity of bony contour, tenderness over the fracture site, step deformity or bony crepitus, anesthesia or paresthesia of lower lip and limitation of mouth opening.
Intra-oral: Ecchymosis or hematoma especially in the lingual sulcus, which is almost pathognomonic of a fracture, obvious laceration in the overlying mucosa, occlusal disturbance, tenderness, and step deformities in the bone.
Radiographical examination: A pre-operative radiographical examination was obtained for all patients to diagnose and assess the site and the extent of the fractures. The views included:
• Orthopantomogram (OPG) (Figure 3A).
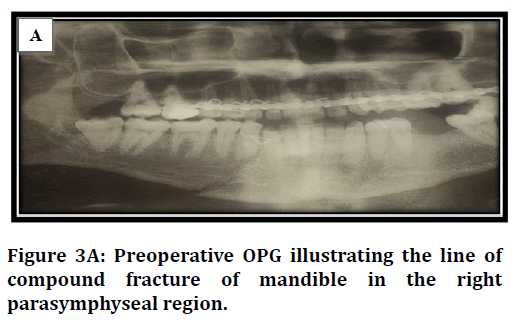
Figure 3a. Surgical training questionnaire
• Posteroanterior mandible (PA) (Figure 3B).
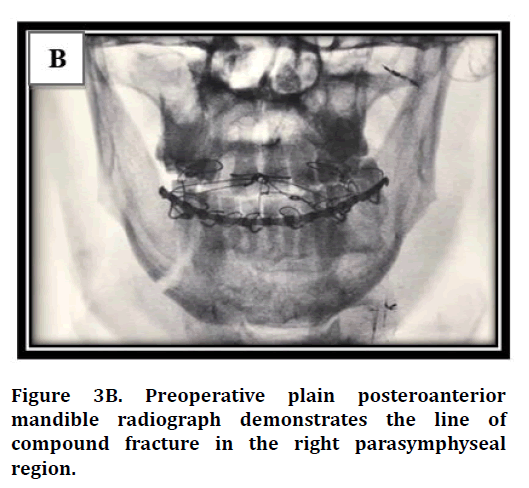
Figure 3b. Surgical training questionnaire
• Computed tomography (CT) scan (Figure 3C and 3D).
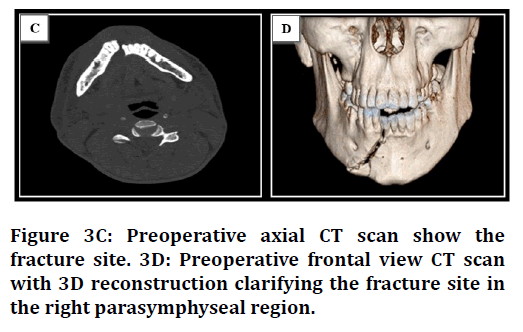
Figure 3c. Surgical training questionnaire
Surgical procedure
After stabilization of the occlusion with Erich arch bar and intermaxillary fixation with elastics or stainless-steel soft wire 0.5 mm, an extra-oral or intra-oral approach were utilized for open reduction of the fracture site. Extra-oral approach was used when there is an associated extra-oral wound exposing the fractured site of the mandible through the same wound. For intra-oral approach, a proposed vestibular incision with the surgical field infiltrated with 2% lidocaine with 1:80,000 Epinephrine solution to reduce bleeding. Anterior to the first premolar, the incision was either taken into the lip, splitting the mentalis muscle into two layers to facilitate two-layer closure, or in the sulcus below the attached gingival to facilitate single layer closure. Care was taken not to injure the mental nerve. A mucoperiosteal flap is elevated to expose the fracture site. The entire fracture was examined following slight distraction to visualize the obliquity and relationship of the cortices and is compared with the pre-operative radiographs then the direction of insertion of lag screws is decided. Once the fracture has been examined and cleared off all debris and fibrous tissue with a curette, a bone clamp used to assist in firmly reducing and stabilizing the fracture before the application of lag screws. Simultaneously occlusion was maintained by IMF. Selection of the proper point of entry for drilling hole into the buccal cortex was based on placing it sufficiently away from the fracture (about 12-15 mm) and the drill is introduced perpendicular to the line of fracture so that sufficient amount of bone is present between the head of the lag screw and the fracture after drilling and countersinking. The first screw was placed just above the lower border of mandible so that sufficient space was available for a second screw. In cases were placing a second screw was not feasible, Erich arch bar applied on teeth used as a tension band. After establishing the proper point of entry, with the help of a small round bur a depression was made in the neighboring cortex; this depressed point prevents the extra-long drill bit from slipping over the cortical bone while making the drill hole. Two mm extra-long drill bit can be used to the selected angulation (perpendicular to the fracture line) to drill through the buccal cortex passing medullary bone and the lingual cortex. During this procedure copious irrigation of saline solution is manditory and repeatedly the drill bit is withdrawn to prevent clogging and heat generation. The mucoperiosteal flap and adjacent soft tissues were retracted and held with Langen Beck retractors and periosteal elevators to permit for the proper adaptation of drill guide and angulation of extra-long drill bit during drilling. The next step was creating a sunken area by using a large round bur. Care was taken not to countersink deep into the bone to the point where the screw head rested on medullary instead of cortical bone. The depth gauge was then inserted through the hole to determine the length of the screw required for fixation.
Following that, with the help of 2 mm hand tap threads were cut in both inner as well as outer cortex and the drill hole was irrigated thoroughly to clear off any debris. With the help of 2 mm screw holder and screwdriver the lag screw was introduced and tightened. Care was taken not to overtighten the screw. If required, the application of a second lag screw also proceeds in the same way leaving at least 5 mm space between the first and second screws. In case of fractures in the vicinity of mental foramina where it is not possible to place the second lag screw; Erich arch bar was maintained as a tension band for a period of two weeks. The wound was closed in two layers with the use of absorbable suture vicryl 3/0 for muscular layer and black silk suture 3/0(simple interrupted technique). The procedure time measurement was done by using a stopwatch start counting from the incision to the finish of wound closure. It is important to denote that when there is any intraoperative technical complication causing the surgeon to stop or wait for a while, the stopwatch also stopped to collect the proper time.
Postoperative care and follow-up
Intermaxillary fixation can be removed in the first day postoperatively and the patient advised to remain on soft diet for a period of two weeks. All the patients placed on systemic antibiotic coverage consisted of Ceftriaxone 1g IV twice a day in addition to Metronidazole 500 mg IV infusion every eight hours for seven days. Analgesic (Diclofenac ampule 75 mg on need) was prescribed immediately post operatively for relief of pain. Dexamethasone 8 mg ampoules started to be given I.M. from the first day of operation and continued two times daily for two days in order to reduce oedema. Intravenous antibiotic was given during the period of hospitalization and been replaced by oral preparations, Amoxicillin /Clavulanate potassium 625 mg cap every eight hours and Metronidazole 500 mg tablets every eight hours were administered after the patient’s discharged. For a patient allergic to penicillin, Cephalexin 500 mg capsule were given and in case of allergy to cephalosporin, macrolides (Erythromycin 500 mg four times a day) were given. Antibiotic treatment was maintained for seven days postoperatively.
All patients were instructed to maintain good oral hygiene measures and 0.2 % Chlorhexidine mouth wash was requested at least twice daily for ten days. Postoperative radiographs (OPG) were taken on the second postoperative day to confirm the accuracy of reduction and the position of screws. Sutures were removed on the seventh postoperative day.All patients were informed to be seen every week for one month postoperatively and then once monthly in the subsequent period for six months. During the follow up period, postoperative complications were assessed, recorded, and managed. The assessment includes pain on fracture site, evaluation of occlusion, mental nerve examination, disfigurement, infection, wound dehiscence, malunion and non-union.
Post-operative clinical assessment
Stability of the fracture: checked by forceful bimanual manipulation of the segments (following IMF removal) to check for mobility presence or absence.
Occlusion: was checked clinically if there was any step or gap in the occlusal plane while teeth in occlusion. When all the teeth in either of the fracture fragments were out of occlusion, they considered to be severe derangement. When only few teeth (one to two teeth) in either of the fracture fragments or both fragments were out of occlusion was considered as mild occlusal discrepancy.
Mental nerve injury: nerve function was evaluated by gentle stroking of the skin in the region of mental nerve and chin by using cotton role. The subjective sensations of the patient be recorded.
Findings then recorded one day, two weeks, four weeks, and six weeks post operatively (appendix).
Post-operative radiographic assessment
Orthopantamogram (OPG) and posteroanterior mandible (PA) view radiographs were used for radiographic assessment.
Screw position assessment: The position was assessed using OPG to see if the screws penetrated the mandibular canal or adjacent roots (Figure 4A and 4B). Findings was recorded immediate postoperatively and six weeks later to look for any displacement of screws when compared to immediate post-operative position.
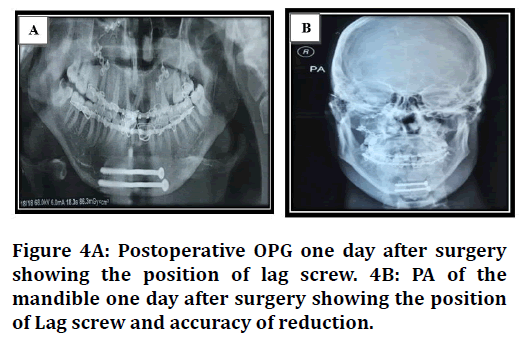
Figure 4. Surgical training questionnaire
Accuracy of reduction: Accuracy of reduction was assessed using mandibular radiograph to see if there was any discrepancy in the continuity of the outer cortex, inner cortex, or inferior border of the mandible Figure 4A and 4B). Findings were recorded immediate postoperatively, one week, two weeks, one month and six months postoperatively.
Bone healing: was assessed by observing if there is a visible radiolucent gaping at the fracture line or absence of this sign. The absence of radiolucency at the fracture line considered as complete bony union, while the presence of radiolucent gaping or visible radiolucent line is considered as incomplete bony union Figure 5A and 5B). These findings were reported six months post operatively.
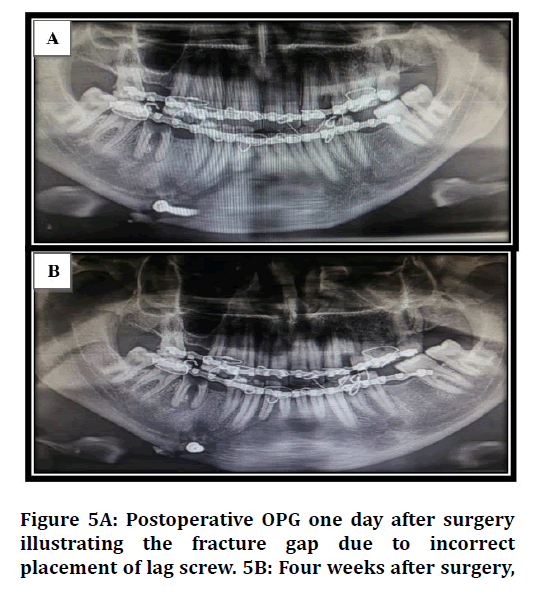
Figure 5. Surgical training questionnaire
Statistical analysis
The data analyzed using Statistical Package for Social Sciences (SPSS) version 25. The data presented as mean, standard deviation and ranges. Categorical data presented by frequencies and percentages. Independent t-test and Analysis of Variance (ANOVA) (two tailed) was used to compare the continuous variables accordingly. Chi square test was used to assess the association between intraoperative complication and mobility with certain information. A level of P – value less than 0.05 was considered significant.
Results
The total number of the study patients was 10. All of them were diagnosed with symphyseal, parasymphyseal, and oblique body fracture and treated by open reduction and fixation using lag screws under general anaesthesia.
Age and gender
The distribution of study patients by age and gender is shown in Figure 6. Study patient’s age was ranging from 14-50 years with a mean of 24.2 years (standard deviation of ± 13.5 years).
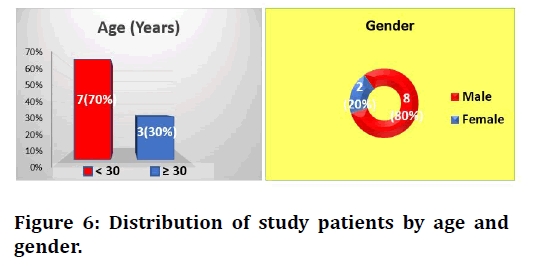
Figure 6. Surgical training questionnaire
The highest proportion of study patients was aged < 30 years (70%). Regarding gender, the proportion of males was higher than females of 80% versus 20% with a male to female ratio of 4:1.
Clinical informations
Table 1 demonstrates the distribution of study patients by certain clinical informations. Parasymphyseal and body fractures were the most common sites of fracture (40% for each).
| Variable | No. (n= 10) | Percentage (%) |
|---|---|---|
| Site of fracture | ||
| Symphyseal | 2 | 20 |
| Parasymphyseal | 4 | 40 |
| body fracture | 4 | 40 |
| No. of lag screw used | ||
| 1 | 3 | 30 |
| 2 | 7 | 70 |
| Arch bar used | ||
| Yes | 4 | 40 |
| No | 6 | 60 |
Table 1: Distribution of study patients by clinical informations.
It had been noticed that two lag screws were used in 70% of study patients and arch bar was utilized in 40% of them.
Surgical approach
Figure 7 illustrates the distribution of study patients by surgical approach. Surgical procedures were distributed equally via extraoral and intraoral approaches.
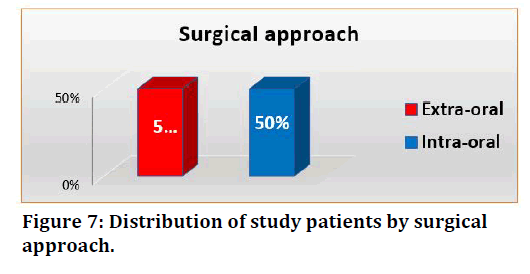
Figure 7. Surgical training questionnaire
Intra and postoperative informations
Stability of fracture
The distribution of study patients by stability of fracture is clarified in Table 2.
| Time interval | Stability of fracture | |
|---|---|---|
| Mobility present (%) | Mobility absent (%) | |
| Intraoperatively | 4 (40.0) | 6 (60.0) |
| One month postoperatively | 2 (20.0) | 8 (80.0) |
| Six months postoperatively | 0 (0) | 10 (100.0) |
Table 2: Distribution of study patients by stability of fracture.
Mobility was absent in 60% of them intraoperatively, while it was being 80% after one month.
After six months, all study patients did not show any mobility.
Evaluation of occlusion
The distribution of study patients contributed to the evaluation of occlusion is reported in Table 3. Occlusion was corrected in 90% of them intraoperatively.
| Time interval | Evaluation of occlusion | |
|---|---|---|
| Corrected occlusion (%) | Deranged occlusion (%) | |
| Intraoperatively | 9 (90.0) | 1 (10.0) |
| One month postoperatively | 10 (100.0) | 0 (0) |
| Six months postoperatively | 10 (100.0) | 0 (0) |
Table 3: Distribution of study patients by evaluation of occlusion.
Accuracy of bone reduction
Table 4 shows the distribution of study patients in relation to the accuracy of bone reduction. No displacement observed in 90% of them intraoperatively.
| Time interval | Accuracy of bone reduction | |
|---|---|---|
| No displacement (%) | Displacement (%) | |
| Intraoperatively | 9 (90.0) | 1 (10.0) |
| One month postoperatively | 10 (100.0) | 0 (0) |
| Six months postoperatively | 10 (100.0) | 0 (0) |
Table 4: Distribution of study patients by accuracy of bone reduction.
Bone healing
Bone healing of patients is demonstrated in Table 5. One month postoperatively, 90% of study patients revealed visible radiolucent line and 40% showed visible gaping atfracture site. After six months, 90% of them presented with complete bony union.
| Time interval | Bone healing | ||
|---|---|---|---|
| Visible gaping at fracture site (%) | Visible radiolucent line (%) | Complete bony union (%) | |
| One month postoperatively | 4 (40.0) | 9 (90.0) | 0 (0) |
| Six months postoperatively | 0 (0) | 1 (10.0) | 9 (90.0) |
Table 5: Distribution of study patients by bone healing.
Intraoperative complications
Figure 8 illustrates the intraoperative complications. It had been noticed that 60% of patients didn’t complain from any intraoperative complications, while fracture of drill and incorrect screw position were occurred in 40% of patients.
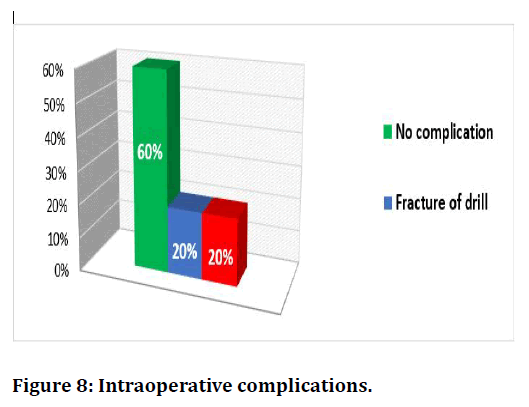
Figure 8. Surgical training questionnaire
Postoperative complications
Figure 9 shows the postoperative complications. Until four and 24 weeks after operation, 90% of study patients didn’t complain from any complication.
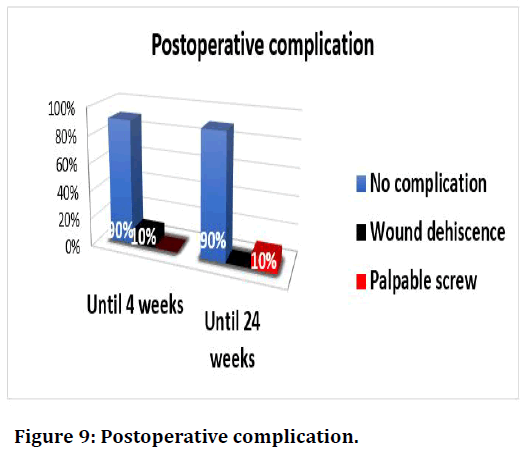
Figure 9. Surgical training questionnaire
Duration of operation
Table 6 demonstrates the comparison in time of operation according to certain surgical information. It had been noticed that the mean duration of operation was significantly higher in operation performed by extraoral approach than that by intra-oral approach (93.4 versus 82 minutes, P= 0.01), and significantly higher in patients with oblique body fracture than that in patients with symphyseal and parasympheseal fractures (94.3 versus 80 and 85 minutes, P=0.049).
| Variable | Duration of operation (mints) Mean ± SD | P-Value |
|---|---|---|
| Surgical approach | ||
| Extra-oral | 93.4 ± 5.02 | 0.01 |
| Intra-oral | 82.0 ± 5.7 | |
| Site of fracture | ||
| Symphyseal | 80.0 ± 7.07 | 0.049 |
| Parasymphyseal | 85.0 ± 5.8 | |
| Oblique body fracture | 94.3 ± 5.4 |
Table 6: Comparison in time of operation according to certain surgical informations.
The association between intraoperative complication and certain variables is shown in Table 7. There was no statistically significant association (P ≥ 0.05) observed between intraoperative complication and all clinical features (age, gender, surgical approach, site of fracture, number of lag screws, and using of arch bar).
| Variable | Intraoperative complication | Total (%) No.= 10 | P - value | |
|---|---|---|---|---|
| Yes (%) No.= 4 | No (%) No.= 6 | |||
| Age group (Years) | ||||
| < 30 | 3 (42.9) | 4 (57.1) | 7 (70.0) | 0.667 |
| ≥ 30 | 1 (33.3) | 2 (66.7) | 3 (30.0) | |
| Gender | ||||
| Male | 3 (37.5) | 5 (62.5) | 8 (80.0) | 0.667 |
| Female | 1 (50.0) | 1 (50.0) | 2 (20.0) | |
| Surgical approach | ||||
| Extra-oral | 1 (20.0) | 4 (80.0) | 5 (50.0) | 0.262 |
| Intra-oral | 3 (60.0) | 2 (40.0) | 5 (50.0) | |
| Site of fracture | ||||
| Symphyseal | 1 (50.0) | 1 (50.0) | 2 (20.0) | 0.09 |
| Parasymphyseal | 3 (75.0) | 1 (25.0) | 4 (40.0) | |
| Oblique body fracture | 0 (0) | 4 (100.0) | 4 (40.0) | |
| Number of lag screw used | ||||
| 1 | 2 (66.7) | 1 (33.3) | 3 (30.0) | 0.333 |
| 2 | 2 (28.6) | 5 (71.4) | 7 (70.0) | |
| Using arch bar | ||||
| Yes | 1 (25.0) | 3 (75.0) | 4 (40.0) | 0.429 |
| No | 3 (50.0) | 3 (50.0) | 6 (60.0) | |
Table 7: Association between intraoperative complications and certain variables.
Table 8 represents the association of intraoperative mobility with surgical information. No statistically significant association (P ≥ 0.05) was found between intraoperative mobility and all surgical variables (site of fracture, number of lag screws, and using of arch bar).
| Variable | Intraoperative Mobility | Total (%) No.= 10 | P - value | |
|---|---|---|---|---|
| Present (%) No.= 4 | Absent (%) No.= 6 | |||
| Site of fracture | ||||
| Symphyseal | 0 (0) | 2 (100.0) | 2 (20.0) | 0.435 |
| Parasymphyseal | 2 (50.0) | 2 (50.0) | 4 (40.0) | |
| Oblique body fracture | 2 (50.0) | 2 (50.0) | 4 (40.0) | |
| Number of lag screw used | ||||
| 1 | 1 (33.3) | 2 (66.7) | 3 (30.0) | 0.667 |
| 2 | 3 (42.9) | 4 (57.1) | 7 (70.0) | |
| Using arch bar | ||||
| Yes | 1 (25.0) | 3 (75.0) | 4 (40.0) | 0.429 |
| No | 3 (50.0) | 3 (50.0) | 6 (60.0) | |
Table 8: Association between intraoperative mobility and surgical information.
Discussion
Age and gender distribution
In this study motor vehicle accident was dominant among young males with age group less than 30 years (70%) since traffic rules are not followed with the presence of reckless driving. Males were affected more than females in a ratio of 4:1, this was logical since a major part of patients in this study was military forces (six form about 60% of all patients) in which they are highly prone to trauma; this relatively close to the results reported by Kotrashetti et al. [8] in which the majority of the patients were males (93.3%) and Heidrun et al. [9] who stated that males with mandibular fracture were more than females in a percentage of (95%) with maximum number of patients were in the age group 27 years.
A previous prospective study demonstrated that there was higher number of males, 31 patients (73.80%) suffered from maxillofacial fractures compared to 11 females’ patients (26.20%). This may be attributed to that most of the females staying in door for housework or office work, and that they drive less frequent and more carefully when compared with males. Moreover, females only occasionally participate in trading, industrial work, Iraqi army, or sports. This yield in exposure to less trauma regarding females.
Most of patients in this study suffered from maxillofacial fractures were of the young age. The highest being the age decade ranged from 21-30 years old, were 20 patients (47.60%) and the least was the age group 61-70 years old, 2 patients (4.76%). These decades of young people are violent and immature. They like the thrill of driving and predisposed to unreasonable road traffic accidents. In addition, the increasing trend of war & bomb injuries in Iraq, most of them are involved in this age decades.
Clinical informations
Parasymphyseal and oblique body fracture were the most common sites (40% for each), this may be related to the fact that the symphysis and body of the mandible are more prone to trauma. These are within the line of Michael et al. [10] who stated that body fracture account for about (29.5%) while in contrast parasymphyseal fracture account about (19.5%) of all mandibular fractures. In the present study it was 40%, these differences in percentages may be contributed to the small sample size (only 10 cases).
The arch bar was used as a tension band in four patients (40%) out of total number of 10 patients. Three of them because of using single lag screw as the fracture site was in the parasymphyseal region near the mental nerve which jeopardize the insertion of two lag screws. One patient with fractured mandible accompanied by midface fracture that need arch bar application. The remaining six patients (60%) required no arch bars to be applied. Sanjay et al. [11] in his study used the arch bar one day postoperatively in one case out of ten cases (10%) because of screw got displaced fracturing a portion of buccal cortical plate, so mild mobility was noted which was treated by MMF for a period of 3 weeks. This is close to the study achieved by Sanjay [11] who mentioned that in 2 patients out of 10, placement of second lag screw was not possible due to the proximity of mental foramina, arch bar was used as a tension band splint.
Surgical approach and duration of operation
In the present study, it has been noticed that surgical procedures were performed with equal distribution via extraoral or intraoral approaches. In some cases, intraoral approach was utilized in the parasymphyseal and symphyseal region owing to better access. While extraoral approach was performed either when there is a preexisting extraoral wound associated with the fracture or in case of inaccessible region like in the body of the mandible.
It had been observed that the mean time of operation was significantly higher in those operations achieved via extraoral approach than that with the intraoral one (93.4 versus 82 minutes, (P=0.01). This is logically attributed to that the extraoral approach required more time for dissection to expose the fracture line to accomplish reduction and fixation. Furthermore, the mean time for operation was significantly higher in patients with oblique body fracture than that in patients with symphyseal and parasympheseal fractures (94.3 versus 80 and 85 minutes, P= 0.049). While with symphyseal and parasympheseal fractures the approach were intraorally with good access and minimum dissection were needed. In contrast, Rangila Ram et al. [12] stated that the time taken in using extraoral approach was less than that for intraoral owing to the careful dissection of mental nerve and exposure of lower border.
Basheer-Rehman et al. [13] reported that the intra-oral approach was completed within 30 minutes, while with the extra-oral approach in most procedures (93.34%) were completed in 30-60 minutes time.
Stability of fracture
It has been found in the present study that mobility was absent in 60% of the cases intraoperatively and being 80% after one month. Six months later, all of the study patients didn’t illustrate any mobility. These results may be related to the compression force that applied by lag screw and progress in bone healing process with time. Our results was disagree with with Agnihotri et al [14] in his study who worked on 40 patients treated with using lag screw fixation advocated that all the patients in his study (100%) showed clinically stable fracture fixation with lag screws and postoperative MMF was not required indicating earlier functional rehabilitation.
Evaluation of occlusion and accuracy of bone reduction
In this research, it was observed intraoperatively that occlusion corrected in 90% of the patients, also there was no displacement observed in 90% of them. Only one case was recorded as deranged occlusion with displacement as this was the first case to deal with and the little experience of the researcher with the use lag screw system played role in this issue. So, the positioning of the lag screw was incorrect Figure 5. However, this was corrected postoperatively using arch bar with elastics.
Our result was in coordination with Rangila Ram et al. [12] who stated that postoperative dental occlusion was achieved in all the patients and no intermaxillary fixation required postoperatively and 85% of patients showed good anatomical bone reduction on postoperative CT scan.
Conclusion
• Fixation of anterior mandible fracture using lag screw technique can achieve good stability and appropriate compression.
• The technique is simple and easily performed, reducing the surgical time and the chances of infection due to less exposure of surgical site and promote the healing process by producing stress in the fracture lines.
• The proper selection of cases and careful instrumentation are major factors to be keep in mind when the surgeon utilizing this sort of fixation technique.
• Two lag screws better to be used wherever possible. If, however, this is not possible due to anatomic constraints, the single lag screw should be supplemented with arch bar as a tension band.
• Rigidity achieved by the lag screw fixation is excellent and can be compared to any other form of the rigid fixation.
• Optimal stability of treated fractures by lag screws is obtained in all cases.
• The study reported a low complication rate concerning the use of lag screws.
References
- http://india.accurascan.com/cgi-bin/open/file.php?title=robbins+textbook+of+pathology+8th+edition+pdf&id=4dccc7f9a2d9c9b5596b72b645c30955
- https://www.worldcat.org/title/janeways-immunobiology/oclc/212399882
- Mukhopadhyay S, Farver CF, Vaszar LT, et al. Causes of pulmonary granulomas: A retrospective study of 500 cases from seven countries. J Clin Pathol 2012; 65:51-57.
- Broos CE, van Nimwegen M, Hoogsteden HC, et al. Granuloma formation in pulmonary sarcoidosis. Frontiers Immunol 2013; 4:437.
- James DG. What makes granulomas tick? Thorax 1991; 46:734-736.
- James DG. Granuloma formation signifies a Th1 cell profile. Sarcoidosis 1995; 12:1-3.
- Roman J, Leon YJ, Gal A, et al. Distribution of extracellular matrices, matrix receptors and transforming growth factor-I in human granulomatous inflammation. Am J Med Sci 1995; 309:124-133.
- Reiser H, Stadecker MJ. Costimulatory B7 molecules in the pathogenesis of infectious and autoimmune diseases. N Engl J Med 1996; 335:1369-77.
- Woodard BH, Rosenberg SI, Farnham R, et al. Incidence and nature of primary granulomatous inflammation in surgically remove material. Am J Pathol 1982; 6:119-129.
- https://www.sciencedirect.com/book/9780702034855/weedons-skin-pathology
- Lever WF, Schaumberg-Lever G. Histopathology of the skin. Philadelphia, JB Lipincott Company, 8th Edn.1997; 51- 60.
- John D Bancroft. Theory and practice of Histological techniques. 6th Edn Churchill Livingstone, 2007; 178-298.
- Jardine DL, Chambers ST, Hart DJ, Chapman BA. Primary biliary cirrhosis presenting with granulomatous skin lesions. Gut. 1994 Apr 1;35(4):564-6.
- Zafar MNU, Sadiq S, Menon MA. Morphological study of different granulomatous lesions of the skin. J Pak Assoc Dermatol 2008; 18:21-28.
- Mohan H, Bal A, Dhami GP. Non-infectious granulomatous dermatitis: A clinicopathological study. J Cutan Pathol 2006; 33:767-71.
- Dhar S, Dhar S. Histopathological features of granulomatous skin diseases: an analysis of 22 skin biopsies. Indian J Dermatol 2002; 47:88.
- Gautam K, Pai Bhat. Clinicopathological correlation of granulomatous lesions of skin. J Pathol Nepal 2011; 1:81-86.
- http://www.mjpath.org.my/past_issue/MJP1980/skin-lesions-in-leprosy.pdf
- Nadkarni NS, Rege VL. Significance of histopathological classification in leprosy. Indian J Lepr 1999; 71:329-331.
- Moorthy BN, Kumar P, Chatura KR, et al. Histopathological correlation of skin biopsies in leprosy. Indian J Dermatol Venereol Leprol 2001; 67:299-301.
- Hong SJ, Kim DJ, Son SJ, et al. The clinicopathological study of granuloma annulare. Korean J Dermatol 1999; 37:1029-1037.
- Pailoor J. Histopathology of skin lesion in Leprosy. Malaysian J Pathol 1980; 3:39-45.
- Thakur BK, Verma S, Hazarika D. A clinicopathological study of cutaneous tuberculosis at Dibrugarh district, Assam. Indian J Dermatol 2012; 57:63.
- Hirsh BC, Johnson WC. Concepts of Granulomatous information. Int J Dermatol 1984; 23:90-99.
- Pei Shan Yen, Kuo Hsien Wang, Wei Yu Chen, et al. The many faces of necrobiosis lipoidica; A report of 3 cases with histological variations. Dermatologica Sincia 2011; 29:67-71.
- Flores AF. Necrobiosis lipoidica and cutaneous anesthesia: Immunohistochemical study of neural fibres. Folio Neuropathol 2008; 46:154-157.
- Boulton AJ, Outfield RG, Abouganem D, et al. Necrobiosis lipoidica diabeticorum: A clinicopathologic study. J Am Acad Dermatol 1988; 18:530-7.
- Betlloch I, Moragon M, Jorda E, et al. Linear rheumatoid nodule. Int JDermatol 1988; 27:645-646.
- Magro CM, Crowson AN. The spectrum of cutaneous lesions in rheumatoid arthritis: A clinical and pathological study of 43 patients. J Cutaneous Pathol 2003; 30:1-0.
- Sayah A, English JC. Rheumatoid arthritis: A review of the cutaneous manifestations. J Am Acad Dermatol 2005; 53:91-209.
Author Info
Hani Tareq Abd-Alwahab1* and Thair A Lateef Hassan2
1Senior Resident Maxillofacial Surgery, Iraqi Board for Medical Specialization, Iraq2President of the Iraqi Scientific Council of Maxillofacial Surgery in Iraqi Board for Medical Specialization, Iraq
Citation: Hani Tareq Abd–Alwahab, Thair A Lateef Hassan,The Outcomes of the Lag-Screw Use for Treatment of the Mandibular Symphysis, Parasymphysis and Oblique Body Fractures, J Res Med Dent Sci, 2021, 9(6): 44-53
Received: 28-Apr-2021 Accepted: 09-Jun-2021
