Research - (2020) Advances in Dental Surgery
TMJ Ankylosis and OSMF Mutual Cohabitants in Restricted Mouth Opening
Sneha Krishnan, Muthusekhar MR, Senthilnathan Periasamy* and Murugaiyan Arun
*Correspondence: Senthilnathan Periasamy, Department of Oral and Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India, Email:
Abstract
Temporomandibular joint ankylosis is defined as the fusion between two articular surfaces of the TMJ (condyle and glenoid fossa) by fibrous or bony tissue. Oral submucous fibrosis is an insidious chronic disease which leads to stiffness of the oral mucosa and causes trismus and inability to eat. The aim of this case report is to study a rare case of simultaneous occurrence of TMJ ankylosis and oral submucous fibrosis in the same patient. In this present case, the patient had presented with limited mouth opening, but the diagnosis of oral submucous fibrosis was overlooked in the first scenario. It was concluded that the patient had acquired OSMF before TMJ ankylosis, as fibrosis tends to set in earlier than bony fusion and due to noncompliance of jaw exercises one condition aggravated and led to formation of another. This case was treated with release of the TMJ Ankylosis and the surgical created defect was filled with interpositional dermis fat graft. Following this fibrotomy was performed intraorally to relieve the fibrous bands and a split skin graft prepared over a polyethylene stent was placed over the raw wound area. Patient was advised aggressive physiotherapy post-surgery, as both conditions were present as mutual cohabitants resulting in restricted mouth opening.
Keywords
TMJ ankylosis, Oral submucous fibrosis, Temporomandibular joint ankylosis, Dermis fat graft, Split skin graft, Polyethylene stent
Introduction
Restricted mouth opening has serious health implications such as malnutrition due to impaired mastication, difficulty in speech, and compromised oral hygiene resulting in functional deficit of the stomatognathic system [1]. It is generally believed that “If you diagnose two rare conditions in the same patient, you are rarely correct” [2]. Temporomandibular joint (TMJ) ankylosis is a pathologic condition where the mandible is fused to the fossa by bony or fibrotic tissues [3]. There are multiple factors that can result in TMJ ankylosis, trauma being the most common cause. Few deformities of the maxillofacial region present with such a wide constellation of symptoms and clinical findings as ankylosis of the temporomandibular joint. Management of TMJ ankylosis requires aggressive surgical intervention, the main objectives of whichever are resection of ankylosed bone, restoration of form, and function and prevention of recurrence [4]. Reduced mouth opening can result from trismus as in case of OSMF, where accumulation of inelastic fibrous tissue in the juxta epithelial region results in stiffness of oral mucosa. In addition to this, subsequent muscle degeneration leads to fibrosis and scarring of temporalis muscle, further enhancing the limitation in mouth opening [1]. The incidence of the two different diseases occurring in the same patient is an exception rather than the rule [2].
With a rich case bank established over 3 decades we have been able to publish extensively in our domain [5-15]. Based on this inspiration we aim to study a rare case of simultaneous occurrence of TMJ ankylosis and oral submucous fibrosis in the same patient.
Case Report
A 28-year-old male patient reported with the chief complaint of limited mouth opening for 12 years which was associated with burning sensation of mouth. Patient had a history of road traffic accident at 17 years of age for which he underwent intermaxillary fixation for a month.Patient also had a history of smoking and pan chewing for the past 12 years and mild burning sensation while eating spicy food. On extraoral examination the right condyle was palpable with tenderness on opening the mouth. There was restriction of right-side movement during side to side movement as well. Intraoral examination revealed palpable fibrotic bands with blanching present on both right and left side of buccal mucosa which was suggestive of oral submucous fibrosis. Mouth opening was evaluated preoperatively by measuring the inter incisal distance using a ruler and the measurement was revealed to be 20 mm. A preoperative computed tomography scan was taken which revealed a mushroom shaped ankylotic mass with a definitive bony bridging between the zygomatic arch and the right condyle. A welldefined antegonial notch was also seen in relation to the right side of the mandible. We concluded with the final diagnosis as TMJ ankylosis of the right side (Sawhney Classification Type 3) with oral submucous fibrosis Type 3 (Khanna and Andrade's Classification) (Figures 1 and 2).
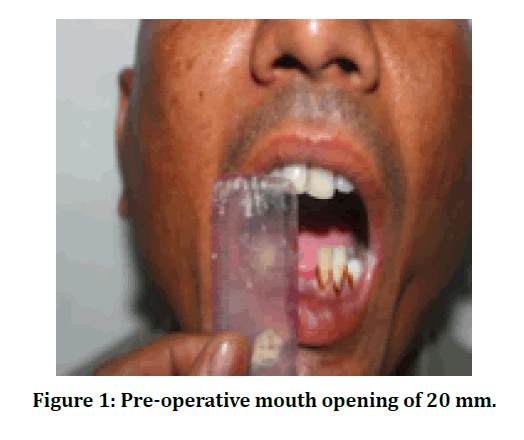
Figure 1: Pre-operative mouth opening of 20 mm.
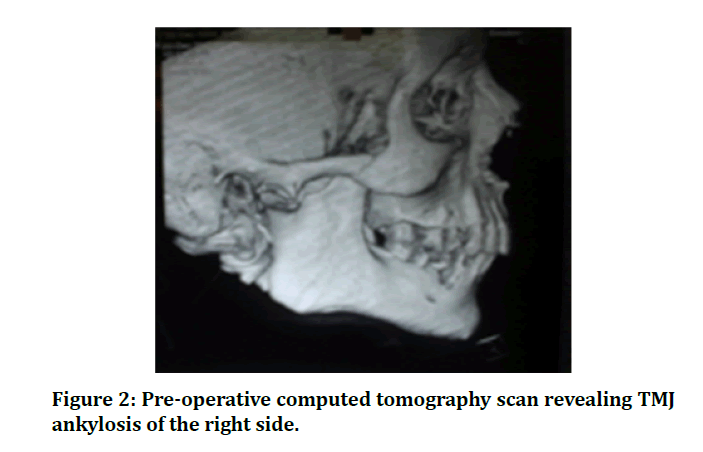
Figure 2: Pre-operative computed tomography scan revealing TMJ ankylosis of the right side.
Patient was planned and taken up for surgery. General anaesthesia with nasotracheal intubation and total muscle relaxation was administered. A preauricular incision with a temporal extension was made. The ankylosed TMJ was palpable and an incision was made directly onto the bone, exposing the ankylosed TMJ. Following this gap arthroplasty was performed by excision of the ankylotic mass beginning from the condylar neck at the level of the sigmoid notch inferiorly to a minimum 12 mm superior to this. To prevent accidental penetration into the middle cranial fossa during the excision of the ankylotic mass, the surgically created gap was at least 5 mm or more below the normal level of the original joint space. This provided a definite safety margin.The surgically created gap was filled with autogenous dermis fat procured from the patient's abdomen. The graft was folded onto itself with the dermis surfaces apposed well and the subcutaneous fat was neatly trimmed. The graft was then passively placed to fill the gap maximally ensuring that all the dead space was eliminated. Thus, dermis-fat interposition arthroplasty was done. The donor site in the abdomen was repaired by primary closure after the graft was harvested.
Fibrotomy was then performed intraorally to relieve the fibrous bands bilaterally. The extent was posteriorly up to the anterior tonsillar pillars and anteriorly up to the corner of the mouth. The fibrotic bands were palpated and freed by finger manipulation until no restrictions were felt. Following this, a split skin graft was prepared and harvested from the thigh. A surgical stent was prepared preoperatively by cutting a polyethylene sheet into an oval shape of adequate size for the patient. To ensure sterility, it was placed in 2% glutaraldehyde solution overnight. Intra operatively, the stent was cut into the adequate size for the patient. The graft was then stretched over the prepared polyethylene surgical stent and adapted onto the raw wound area. The graft and stent were secured by through-and-through bolster 2-0 silk sutures, and the stent was kept in place for 7 days, following which it was removed. Patient received prophylactic antibiotics for 3 days postoperatively. By this we achieved a maximum incisal opening of 35 mm on table as opposed to a pre-operative mouth opening of 20 mm along with reduction in pain and improvement in jaw function. The patient has been followed up regularly at an interval of 3 and 6 months and his mouth opening has been sustained due to meticulous practice of aggressive physiotherapy (Figures 3-8).
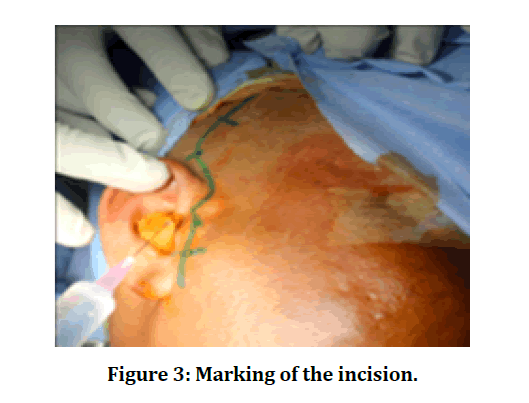
Figure 3: Marking of the incision.
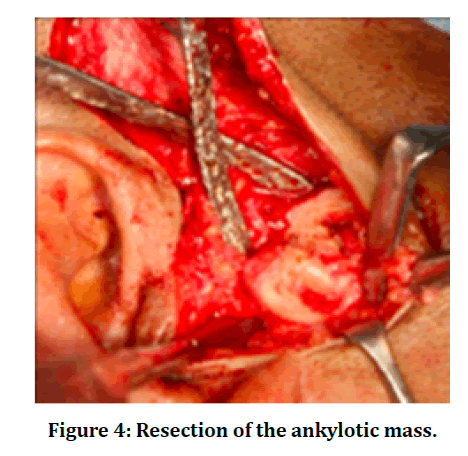
Figure 4: Resection of the ankylotic mass.
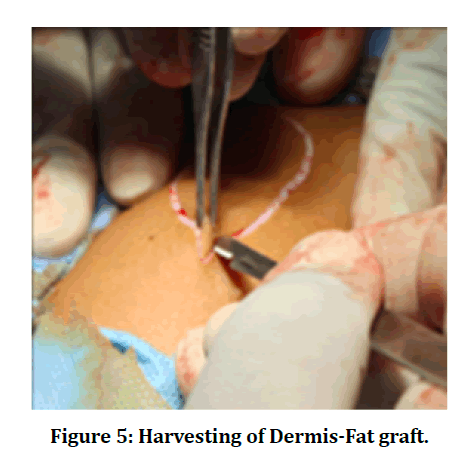
Figure 5: Harvesting of Dermis-Fat graft.
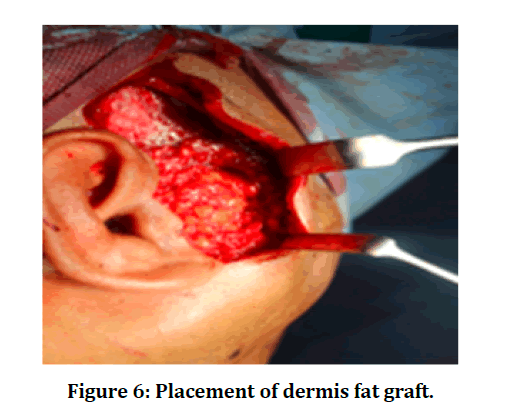
Figure 6: Placement of dermis fat graft.
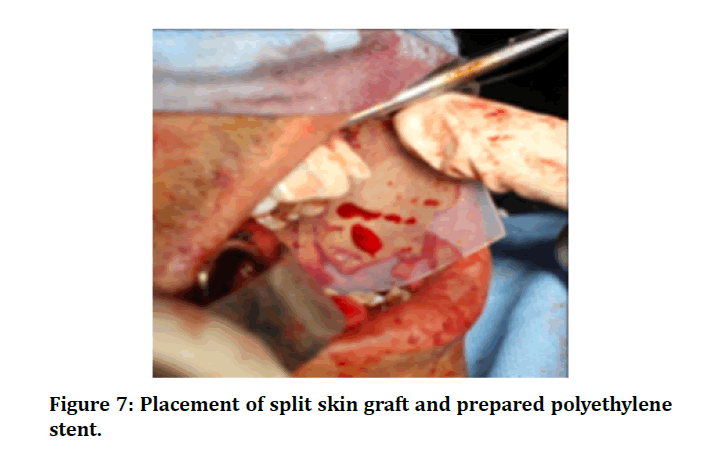
Figure 7: Placement of split skin graft and prepared polyethylene stent.
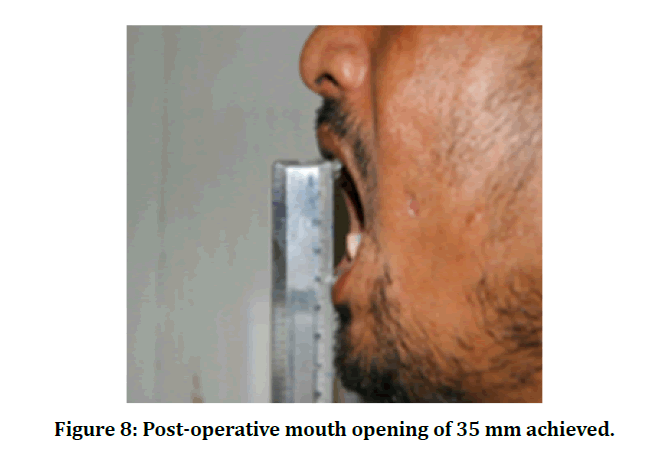
Figure 8: Post-operative mouth opening of 35 mm achieved.
Discussion
Ankylosis of the temporomandibular joint (TMJ) is a rare phenomenon that results in chronic and severe limited mouth opening [16]. TMJ Ankylosis can be classified into true ankylosis (intracapsular) and pseudo ankylosis (extracapsular). True ankylosis of the TMJ is defined as any condition that produces fibrous or bony adhesions between the articular surfaces of the TMJ [17]. True ankylosis is most associated with trauma or infection [18]. Pseudoankylosis results from muscular, osseous, neurological, or psychiatric disorders. Iatrogenic causes of ankylosis may arise from cytotoxic medication, repeated TMJ surgery and irradiation [16]. Diagnosis of TMJ ankylosis is usually made by clinical examination and imaging studies, such as plain films, orthopantomograms, computed tomography (CT) scans, MRI, and threedimensional reconstruction [19].
Sawhney et al. [20] and his colleagues [21] proposed a classification system for TMJ ankylosis:
Type 1: The head of the condyle is flattened or deformed by lying closely approximated to the upper articular surface.
Type 2: The head of the condyle is misshaped or flattened, but it is still distinguishable and lies in close approximation to the articular surface.
Type 3: A bony block is seen to bridge across the ramus of the mandible and the zygomatic arch.
Type 4: The bony block is wide and deep and extended between the ramus and the upper articular surface, completely replacing the architecture of the joint [3].
The management goal in TMJ ankylosis is to increase the patient’s mandibular function, correct associated facial deformity, decrease pain, and prevent re-ankylosis. The two primary objectives of surgery are:
1. To establish jaw movement and jaw function by surgical release of the ankylosis.
2. To prevent relapse by interpositional grafting, early jaw mobilization and intensive physiotherapy [16].
In order to manage TMJ ankylosis multiple treatment modalities including gap arthroplasty, interpositional arthroplasty, and total joint reconstruction (TJR) have been proposed. The requirement to use an interpositional material to prevent TMJ re-ankylosis after arthroplasty in treatment of TMJ ankylosis has been widely discussed [17]. Autogenous tissues, such as ear cartilage, temporalis muscle flap, dermis, fat, and bone, have been used or after gap arthroplasty [3].Today, gap arthroplasty with interpositional grafting has become the acceptable standard for the primary surgical management of TMJ ankylosis as it is a more effective means of reducing re-ankylosis [22].
The first interpositional graft was developed by Eschmarc in the 19th century who described the pterygomasseteric sling technique of suturing together the masseter and medial pterygoid muscles across a divided mandibular ramus. The first reported use of autologous fat graft placement into the TMJ for the treatment of ankylosis was by Blair et al. [23] in 1913 followed by Murphy et al. [24] in 1914. Wolford et al. [25] published the first study evaluating fat grafts placed around TMJ total joint prostheses.
Although there is no interpositional graft material that fulfills all conditions, the rationale for placing autologous dermis fat grafts in this case was for multifold [2]. Dermis fat graft has the potential to obliterate the dead space around the joint. This helps in preventing the formation and subsequent organization of a blood clot. The presence of pluripotential cells is thus minimized due to creation of this physical barrier, which thereby prevents the formation of extensive fibrosis and heterotopic calcification. The fat grafts may be an obstruction to heterotopic bone formation and may also isolate any residual reactive tissue which may have been present from previous alloplastic failure or disease to the periphery of the region. This helps in minimizing its formation around the joint components [3].
Dermis-fat grafts are more stable and less likely to fragment when handled and manipulated into a cavity such as a gap arthroplasty. They can be easily sculptured with fine scissors to fit neatly into any size cavity which is the greatest advantage of this material to other interpositional materials which have been already reported [16]. They also tend to show little change in the volume of the graft in non-load bearing areas [26]. Graft procurement is relatively quick and easy, with minimal morbidity [27,28]. With dermis-fat interpositional grafts there is availability of ample interpositional material, it can be passively placed, and dermis acts like a scaffold to hold the graft [16]. The most common complication found in the donor area was seroma or hematoma, which however could be treated with aspiration and pressure dressing [3].
Oral submucous fibrosis is a chronic insidious disease that has been identified as a precancerous condition, with a potential for malignant transformation of 7–30% [29]. It is attributed most to areca nut chewing which is said to result in the activation of a cascade of matrix metalloproteinases and other enzymes which ultimately result in promotion of fibrogenesis [30]. The disease most commonly begins as a burning sensation and intolerance to spicy food which was seen in this case. This is followed by ulceration and vesicle formation, after which fibrosis with paleness and blanching of the oral mucosa ensues [31].
Currently treatment for OSMF includes both surgical and conservative management. Conservative management includes the use of antioxidants, corticosteroid injections and proteolytic agents [32,33]. Surgical management commonly involves incision and release of fibrous bands which relieves the trismus [34]. This is followed by covering the raw wound area with suitable grafts and flaps like split skin grafts [35], buccal fat pad [36], or other local flaps [37].
The split skin graft, although an older technique, is still a viable option for the treatment of OSMF. The graft with a simple polyethylene stent, provides the surgeon with a cheap and costeffective method in treating OSMF. The stent helps in securing the skin graft to the wound, which was done in this case with the aid of through and through bolster sutures passed through the cheek. The stent also allows the graft to be spread sufficiently over the raw wound area and being semi-rigid, it helps in keeping the patients’ mouth open in the immediate postoperative period which helps in contributing to the success in regaining mouth opening later. However patient compliance is of utmost importance in the success of this surgical treatment [38].
Due to high recurrence of both these entities, the goal in restoring normal mouth opening and function in this case poses a significant challenge to the operating surgeon [2]. Meticulous postoperative physiotherapy is extremely essential when either of the pathology is treated in the patients, moreover when both are present in a single patient as mutual cohabitants.
Conclusion
Unusual presentation of both these conditions in the same patient presents us with a dichotomy as to whether there exists any relationship between the two pathologies. It also raises the importance in establishing the causative factors in such cases. To rule out any occurence of TMJ ankylosis, an orthopantomogram is a must for every patient presenting with OSMF. Also, in patients presenting with both these conditions, active mouth opening exercises are essential to prevent shrinkage and adhesions postoperatively. Therefore, this makes it one of the main factors behind surgical success.
Acknowledgement
The authors would like to acknowledge the help and support rendered by the Department of Oral and Maxillofacial Surgery and Information Technology of Saveetha Dental College and Hospitals for their constant assistance with the research.
Conflict of Interests
The authors declare no conflicts of interest.
References
- Gupta H, Tandon P, Kumar D, et al. Role of coronoidectomy in increasing mouth opening. National J Maxillofac Surg 2014; 5:23–30.
- Andrade NN, Gandhewar T, Aggarwal N, et al. Unusually rare occurrence and recurrence of temporomandibular joint ankylosis and oral submucous fibrosis simultaneously in a patient: A surgeon’s dilemma. National J Maxillofac Surg 2019; 10:238.
- Movahed R, Mercuri LG. Management of temporomandibular joint ankylosis. Oral Maxillofac Surg Clin North Am 2015; 27:27–35.
- Shevale VV, Kalra RD, Shevale VV, et al. Management of oral sub-mucous fibrosis: A review. Indian J Dent Sci 2012; 4.
- Wahab PA, Nathan PS, Madhulaxmi M, et al. Risk factors for post-operative infection following single piece osteotomy. J Maxillofac Oral Surg 2017; 16:328–332.
- Eapen BV, Baig MF, Avinash S. An assessment of the incidence of prolonged postoperative bleeding after dental extraction among patients on uninterrupted low dose aspirin therapy and to evaluate the need to stop such medication prior to dental extractions. J Maxillofac Oral Surg 2017; 16:48–52.
- Patil SB, Durairaj D, Kumar GS, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg 2017; 16:312–321.
- Jain M, Nazar N. Comparative evaluation of the efficacy of intraligamentary and supraperiosteal injections in the extraction of maxillary teeth: A randomized controlled clinical trial. J Contemporary Dent Practice 2018; 19:1117–1121.
- PC J, Marimuthu T, Devadoss P, et al. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Related Res 2018; 20:531–534.
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291–297.
- Wahab PA, Madhulaxmi M, Senthilnathan P, et al. Scalpel versus diathermy in wound healing after mucosal incisions: A split-mouth study. J Oral Maxillofac Surg 2018; 76:1160–1164.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in south India. Annals Maxillofac Surge 2019; 9:114–117.
- Ramadorai A, Ravi P, Narayanan V. Rhinocerebral mucormycosis: A prospective analysis of an effective treatment protocol. Annals Maxillofac Surg 2019; 9:192–196.
- Senthil Kumar MS, Ramani P, Rajendran V, et al. Inflammatory pseudotumour of the maxillary sinus: Clinicopathological report. Oral Surg 2019; 12:255–259.
- Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Annals Maxillofac Surg 2019; 9:110–113.
- Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg 2004; 33:755–760.
- Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg 2001; 30:189–193.
- Haidar Z. Ankylosis of the temporo-mandibular joint; causes and management. J Oral Med 1986; 41:246–249.
- Spijkervet FK, de Bont LG, Boering G. Management of pseudoankylosis of the temporomandibular joint: Report of cases. J Oral Maxillofac Surg 1994; 52:1211–1217.
- Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plastic Reconstructive Surg 1994; 77:29–40.
- He D, Yang C, Chen M, et al. Traumatic temporomandibular joint ankylosis: Our classification and treatment experience. J Oral Maxillofac Surg 2011; 69:1600–1607.
- Moorthy AP, Finch LD. Interpositional arthroplasty for ankylosis of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1983; 55:545–552.
- Blair VP. Operative treatment of ankylosis of the mandible. Surg Gynecol Obstetr 1914; 19:436.
- Murphy JB. Arthroplasty For Intra-Articular Bony And Fibrous Ankylosis Of Temporomandibular Articulation: Report of nine cases. J Am Med Assoc 1914; 23:1783–1794.
- Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: Preliminary treatment outcomes. J Oral Maxillofac Surg 1997; 55:245–251.
- Mackay DR, Manders EK, Saggers GC, al. The fate of dermal and dermal-fat grafts. Annals Plastic Surg 1993; 31:42–46.
- Topazian RG. Etiology of ankylosis of temporomandibular joint. J Oral Surg 1964; 22:227–235.
- Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg 1966; 24:405–409.
- Pindborg JJ. Oral submucous fibrosis as a precancerous condition. J Dent Res 1966; 45:546–553.
- Rajalalitha P, Vali S. Molecular pathogenesis of oral submucous fibrosis--a collagen metabolic disorder. J Oral Pathol Med 2005; 34:321–328.
- Rajendran R, Deepthi K, Nooh N, et al. α4β1 integrin-dependent cell sorting dictates T-cell recruitment in oral submucous fibrosis. J Oral Maxillofac Pathol 2011; 15:272.
- Lai DR, Chen HR, Lin LM, et al. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Pathol Med 1995; 24:402–406.
- Kerr AR, Warnakulasuriya S, Mighell AJ, et al. A systematic review of medical interventions for oral submucous fibrosis and future research opportunities. Oral Diseases 2011; 17:42–57.
- Aziz SR. Oral submucous fibrosis: case report and review of diagnosis and treatment. J Oral Maxillofac Surg 2008; 66:2386–2389.
- Yen DJC. Surgical treatment of submucous fibrosis. Oral Surg Oral Med Oral Pathol 1982; 54:269–272.
- Yeh CJ. Application of the buccal fat pad to the surgical treatment of oral submucous fibrosis. Int J Oral Maxillofac Surg 1996; 25:130–133.
- Bande CR, Datarkar A, Khare N. Extended nasolabial flap compared with the platysma myocutaneous muscle flap for reconstruction of intraoral defects after release of oral submucous fibrosis: A comparative study. Br J Oral Maxillofac Surg 2013; 51:37–40.
- Soh CL, Muthusekhar MR. Treatment of oral submucous fibrosis using split skin graft and a polyethylene stent: A prospective study. J Maxillofac Oral Surg 20114:5; 370–373.
Author Info
Sneha Krishnan, Muthusekhar MR, Senthilnathan Periasamy* and Murugaiyan Arun
Department of Oral and Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, IndiaCitation: Sneha Krishnan, Muthusekhar MR, Senthilnathan Periasamy, Murugaiyan Arun, TMJ Ankylosis and OSMF Mutual Cohabitants in Restricted Mouth Opening, J Res Med Dent Sci, 2020, 8 (7): 253-258.
Received: 16-Sep-2020 Accepted: 02-Nov-2020 Published: 09-Nov-2020
