Research - (2019) Volume 7, Issue 5
To Compare the Efficacy of Dexamethasone Versus Ketorolac with Ropivacaine for Nerve Stimulator Guided Infraclavicular Brachial Plexus Block: A Prospective Randomised Comparative Study
Gudala Prasanna Kumar1 and Middepogu Yerra Sun Kanna2*
*Correspondence: Middepogu Yerra Sun Kanna, Department of Anaesthesiology, Nimra Institute of Medical Sciences, Vijayawada, Andhra Pradesh, India, Email:
Abstract
Introduction: Infraclavicular Brachial plexus block is an advanced regional anaesthetic technique well suited for hand and fore arm surgeries. The aim of the study is to determine the efficiency of Ropivacaine with Ketorolac for infraclavicular Brachial plexus block for hand and fore arm surgeries.
Methodology: 50 ASA grade I and II patients, aged between 18–58 years. of both sexes were randomly allocated into two groups equally of D and K. Group D were assigned to receive Infraclavicular Brachial plexus block under nerve stimulator guided technique with 0.5% Ropivacaine 28 ml+Dexamethasone 2 ml (8 mg) [total volume of 30 cc] Group K were assigned to receive Infraclavicular Brachial plexus block with 0.5% Ropivacaine 28 ml+Ketorolac 2 ml (60 mg) [total volume of 30 cc].
Results: The mean duration of sensory and motor block was significantly prolonged in group D compared to group K,10.5 vs. 9.3 hours for sensory block and 8.5 vs. 6.40 hours for motor block, p<0.05. The mean time to first request analgesia was significantly prolonged in group D compared to group K, 17.40 hours, 12.40 hours respectively.
Conclusions: Ropivacaine with dexamethasone combination produced profound analgesia and prolonged postoperative analgesia when compared to Ropivacaine with ketorolac.
Keywords
Dexamethasone, Perineural block, Local anaesthetic, Ketorolac, Nerve stimulator guided technique
Introduction
Infraclavicular Brachial plexus block is an advanced regional anaesthetic technique well suited for distal arm and fore arm surgeries [1]. Several techniques for infraclavicular blocks have been described. The coracoid approach was first described by Kurt Whiffler in 1981 [2]. Though coracoid approach has been popular, now-a-days approaches around the mid clavicle has come into vogue because of success rate with single injection technique with nerve – stimulator guidance through precision and expertise is required [3,4]. The nerves that are blocked muscle cutaneous nerve, radial nerve, median nerve, and ulnar nerve [5]. Local anaesthetic Ropivacaine is being widely used for regional blocks because of its safety and availability [6]. Ropivacaine acts by causing reversible inhibition of sodium influx thus blocking conduction of impulses in nerve fibres. Various adjuvants like fentanyl, dexamethasone, dexmedetomidine, clonidine, ketorolac, magnesium sulphate etc. were added to local anaesthetics to improve the speed of onset, quality and duration of block [7,8]. Ketorolac is parenteral NSAID which produces anti-nociception by inhibition of prostaglandin synthesis. Dexamethasone produces antinociception by decreasing the release of inflammatory mediators, inhibiting potassium channel regulated discharge of C-fibres and also by reducing ectopic neuronal discharge.
The aim of the study is to determine the efficiency of Ropivacaine with Ketorolac for infraclavicular Brachial plexus block for hand and fore arm surgeries.
Materials and Methods
After approval from institutional ethics committee and written and informed consent from patients and their attendants, 50 ASA grade I and II patients, aged between 18–58 years. belonging to both sexes were randomly selected for this single centred, randomised parallel design and comparative study. They were allocated into two groups equally of D and K using computer generated random numbers as following.
Group D: were assigned to receive Infraclavicular Brachial plexus block with 0.5% Ropivacaine 28 ml+Dexamethasone 2 ml [total volume of 30 cc].
Group K: were assigned to receive Infraclavicular Brachial plexus block with 0.5% Ropivacaine 28 ml+Ketorolac 2 ml (60 mg) [total volume of 30 cc].
Exclusion criteria
• Bleeding disorders
• Pt on anticoagulants
• Local infection
• History of allergy to study drugs
• History of contraindication to steroids
• Co-morbid conditions like hepatic, renal, cardiac and pulmonary insufficiencies
Technique
Single injection infraclavicular Brachial plexus block is preferred using 21 G 100 mm insulated needle under the guidance of peripheral nerve stimulator. The patients were placed in supine position with the head facing away from the side to be blocked. The patient’s arm was abducted and flexed at elbow to keep the relationship of land marks to the brachial plexus constant. The coracoid process was identified by palpating the bony prominence just medial to the shoulder while the arm is elevated and lowered. As the arm is lowered the coracoid process meets the fingers of the palpating hand. Medical clavicular head is another land mark. Midpoint of the line connecting coracoid process and medial clavicular head was marked. The needle insertion site was marked approximately 3 cm caudal to the midpoint of the line connecting coracoid process and medial clavicular head. The insertion site was infiltrated with local anaesthetic 2% with 25 G needle. A 100 mm, 21 G insulated needles, attached to nerve stimulator, was inserted at 45° angle to the skin and advanced parallel to the line connecting the medial clavicular head with the coracoid process. The nerve stimulator is initially set to deliver 1.5 mA at 1 Hz. As the needle is advanced, local twitch of the pectoralis muscle is elicited. Once they disappear as the needle advances deeper the patient was observed for the motor responses of the brachial plexus. The goal was to achieve a hand twitch [finger extension] using a current of 0.2 to 0.5 A. Insertion of the needle too medially should be avoided to prevent the occurrence of pneumothorax. With meticulous technique the incidence of pneumothorax is almost negligible. After achievement of the desired response to nerve stimulator, the appropriate volume of local anaesthetic with adjuvant was slowly administered to patients according to the group allocation. The loaded syringes were supplied in sealed envelopes just before the institution of nerve block in wrapped in aluminium foils to ensure blinding. The principal investigator who was aware of the group allocation loaded the syringes and supplied them to the senior anaesthesiologist who instituted the nerve stimulator guided infra clavicular blockade. The anaesthesiologist who performed to infraclavicular block and the senior post-graduate who performed intra operative and post-operative observations and recording of the data were unaware of the study drugs and also group allocation which ensures blinding.
After institution of infra clavicular block, the following parameters were monitored in every patient.
• Onset of sensory blockade
• Duration of sensory blockade
• Onset of motor blockade
• Duration of motor blockade
• Time to first request analgesia
• Post-operative pain by visual analogue scale scoring
• Occurrence of tourniquet pain
• Quality of intra-operative blockade
• Requirement of rescue analgesia in the postoperative period was also observed.
• Onset of sensory block is defined as the time in minutes from administration of block to absence or decrease of any onset of motor block sensation in the operative area.
• Duration of sensory block in the time of drug administration to complete resolution of motor block.
• Quality of intra-operative block is assessed on a grading system as excellent, fair and failed block
• Duration of post-operative analgesia is defined as the time in monitor from administration of the block to patient’s first request for analgesia.
Statistical analysis
Data was analysed statistically. Demographic data was analysed with Fischer exact test. Sensory and motor block comparisons between the two groups were analysed with student-ttest. Data was represented as mean/standard deviation, percentage and absolute numbers. p<0.05 was considered statistically significant.
Results
A total of 50 patients were enrolled for this study. One patient had failed block and was excluded from the study.
Demographic data like Age, weight, American Society of Anaesthesiologists physical status grading, male/female ratio and duration of surgery were comparable between two groups as shown in Table 1, p>0.05 statistically insignificant.
| Variable | Group D | Group K | p Value |
|---|---|---|---|
| Age in years (18-55 years) | 48 ± 5 | 42 ± 6 | 0.065 |
| Weight in kgs | 58.05 ± 8.12 | 62.12 ± 4.32 | 0.059 |
| Male:Female ratio | 14:11 | 15:10 | 0.064 |
| ASA Grading I/II | 16:09 | 18:07 | 0.061 |
| Duration of surgery in minutes | 105 ± 12 | 110 ± 8 | 0.07 |
| p value˃0.05, statistically not significant | |||
Table 1: Patient charecterstics.
Quality of intra-operative blockade is assessed by grading system shown in Table 2 as excellent, fair and failed Block. In group D, 24 patients had excellent blockade and 1 patient had fair blockade. In group K 22 patients had excellent blockade, 2 patients had fair blockade and 1 patient had failed block. The patient who had failed block was given general anesthesia and was excluded from the study, represented in Figure 1. Haemodynamic parameters of mean HR and mean SBP at different time intervals throughout the procedure were comparable between the two groups as represented in Figure 2. Sensory and motor Block characteristics were represented in Table 3, Table 4 and Figure 3. There was no significant difference in the mean onset of sensory Block which was 8.20 ± 0.05 minutes in group D and 7.50 ± 0.35 minutes in group K (p=0.067) respectively. The mean onset time of motor Block was also comparable between two groups, 15.04 ± 0.14 minutes in group D and 14.40 ± 0.40 minutes in group K, with p>0.05, statistically insignificant.
| Excellent | No pain, no discomfort |
| Fair | Mild discomfort, additional analgesic needed |
| Failed block | Needed conversion to GA |
Table 2: Quality of infraclavicular blockade.
| Time in minutes | Group D (n=25) | Group K (n=24) | p value |
|---|---|---|---|
| Onset of sensory block | 8.20 ± 0.15 | 7.50 ± 0.35 | <0.067 |
| Onset of motor block | 15.04 ± 0.14 | 14.40 ± 0.40 | <0.058 |
| p value>0.05, statistically not significant | |||
| Data expressed as mean and standard deviation | |||
Table 3: Mean onset time to sensory and motor blockade.
| Time in hours | Group D N = 25 | Group K N = 24 | P value |
|---|---|---|---|
| Duration of sensory block | 10.50 ± 0.50 | 9.30 ± 0.62 | 0.044 |
| Duration of motor block | 8.50 ± 0.17 | 6.40 ± 0.55 | 0.047 |
| Time to first rescue analgesia | 17.40 ± 1.50 | 12.40 ± 1.35 | 0.035 |
| p<0.05, statistically significant | |||
| Data expressed as mean and standard deviation | |||
Table 4: Mean duration of sensory and motor blockade.
| Supplemental analgesia | Supplemented analgesic intra-operatively |
Supplemented analgesic post-operatively |
|---|---|---|
| Group D (n = 25) | 2% | 24% |
| Group K (n = 24) | 4% | 32% |
| Data expressed as percentage | ||
Table 5: Requirement of supplemental analgesia.
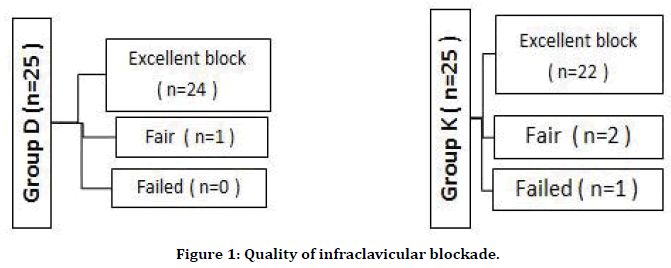
Figure 1. Quality of infraclavicular blockade.

Figure 2. Mean systolic blood pressure and mean heart rate.
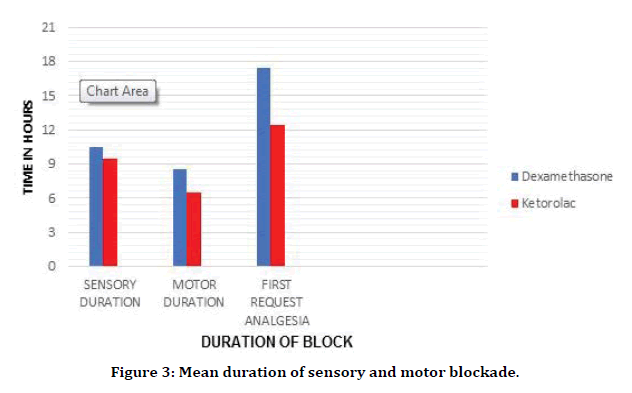
Figure 3. Mean duration of sensory and motor blockade.
The duration of sensory block was significantly prolonged in group D compared to group K, D vs. K 10.50 ± 0.5 vs. 9.30 ± 0.62 hours with a P value of 0.04, which is statistically significant. The mean duration of motor Block was also significantly prolonged in group D than group K, 8. 50 ± 0.17 vs. 6.40 ± 0.55 hours with a p value of 0.047 which was statistically significant. The time to first request analgesia was significantly prolonged in group D compared to group K, 17.40 ± 1.50 vs. 12.40 ± 1.35 hours with a p value 0.005, which is statistically significant.
The post-operative analgesic requirement was reduced in both the groups but significantly reduced in dexamethasone with Ropivacaine group compared to ketorolac with Ropivacaine, group D 24% versus group R 32% required supplemental analgesia post-operatively as represented in Table 5. None of the patients in both the groups complained of adverse effects.
Discussion
Dexamethasone, which is a synthetic glucocorticoid and potent anti-inflammatory agent, has gained interest recently for its role as an adjuvant analgesic along with perineural Blockade as well as other regional and general anaesthesia techniques [9]. Several potential mechanisms of action included suppression of C-fibre transmission of pain signals and reduction of neuronal discharge by the nerve cell [10].
Several RCTs have evaluated the effects of perineural as well as intravenous dexamethasone as adjuvant to peripheral nerve Blocks and demonstrated that both perineural and intravenous dexamethasone caused prolonged sensory Blockade and prolonged duration of post-operative analgesia when compared to placebo [11,12].
Ketorolac is a perineural NSAID which provides analgesia by inhibition of prostaglandin synthesis, studies proved that ketorolac alone produces adequate pain relief when administered parenterally or via wound infiltration [13]. There are few clinical studies that proved the efficacy of ketorolac to prolong the duration of analgesia when administered as adjuvant with LA in perineural Blockade and also IVRA [14]. Ketorolac may be preferred because of its opioid sparing effects. In standard doses ketorolac produces analgesia equivalent to 6-12 mg of morphine for duration between 6-8 hours. With the advent of neuro muscular stimulator and ultrasound guidance infraclavicular Block has become the choice of peripheral nerve Block for fore arm and hand surgeries. As coracoid approach requires multiple injections for success (according to reports by various clinical trials) medial approach was preferred in this study for infraclavicular block [15].
Mirkheshti et al. evaluated the effects of Dexmedetomidine versus ketorolac as local anaesthetic adjuvants on the onset and duration of infraclavicular brachial plexus Block and concluded that the time to first request analgesia was significantly longer in ketorolac group (p=0.016: p<0.001) than Dexmedetomidine had better effects on sensory and motor Block duration and motor Block onset in comparison with ketorolac [16].
Kumar et al. did comparative evaluation of Ropivacaine alone and Ropivacaine with Dexamethasone in Brachial plexus Block and concluded that duration of 8 mg of Dexamethasone to Ropivacaine in supraclavicular Brachial Plexus approach significantly and safely prolongs motor Blockade and Post-operative analgesia compared to Ropivacaine alone [17].
Elyazed et al. evaluated nitro-glycerine and ketorolac as adjuvants to lidocaine for IVRA in patients undergoing fore arm and hand surgeries and concluded that both agents improved the quality of pre-operative analgesia but ketorolac was superior in delaying onset of tourniquet pain and prolonging the duration of post-operative analgesia [18]. In the above studies ketorolac had significantly prolonged the time to first request analgesia when administered perineurally or IVRA along with local anaesthetics. In the present study also, ketorolac produced effective analgesia when administered perineurally with local anaesthetics.
Basenko et al. evaluated the use of Ketorolac as adjuvant in brachial plexus Block with Bupivacaine and concluded that addition of 30 mg of Ketorolac to 40 ml 0.25% Bupivacaine effectively prolonged the duration of postoperative analgesia without significant modification of haemodynamic parameters, the observations were similar to the results of our study with respect to ketorolac [19].
There are very few studies that compared ketorolac versus dexamethasone along with ropivacaine. Paramaswamy et al. compared dexamethasone and Ketorolac as an adjuvant to Bupivacaine in axillary Brachial Plexus Blocks and concluded that both dexamethasone and ketorolac significantly prolonged analgesia and duration of motor and sensory Block, but the effects are more enhanced with dexamethasone [20]. This study is comparable to the present study where dexamethasone with local anaesthetic combination significantly prolonged the duration of analgesia when administered perineurally compared to ketorolac. Also, the effects of analgesia were profound in the dexamethasone group in the present study which correlated well with Paramaswamy et al. study. Many of the studies clearly demonstrated the efficacy of perineural dexamethasone in combination with regional anesthesia; however the safety is still a matter of debate. Marty P et al conducted an animal study in 90 mice with the combination of perineural dexamethasone and Ropivacaine in sciatic nerve blockade, a placebo-controlled study and concluded that this combination allows longer duration of sensory blockade compared with Ropivacaine alone or Ropivacaine and systemic dexamethasone, without increased neural toxicity [21]. Though several studies proved the efficacy of dexamethasone as perineural adjuvant with local anaesthetics, the main concern for off label use of perineural dexamethasone is regarding neurotoxicity [22].
Haseen et al. in their systematic review and meta-analysis on the co-administration of dexamethasone with peripheral nerve block: perineural versus intravenous application, demonstrated the efficacy of perineural dexamethasone when compared to IV route, but mentioned that there is need for critical appraisal of the efficacy and adverse effects which recommends further research on the perineural use of dexamethasone [23].
There are two limitations in this present study. Firstly, the sample size is small and secondly, patients were not followed up for prolonged periods. Patients were followed until discharge only. None of the patients in the present study complained of any neurological adverse effects with the doses used. Hence this study also recommends future research regarding the perineural administration and optimal dosage of dexamethasone.
Conclusion
Perineural dexamethasone and ketorolac produced effective analgesia in combination with Ropivacaine. Ropivacaine with dexamethasone combination produced profound analgesia and prolonged postoperative analgesia when compared to Ropivacaine with ketorolac. No adverse effects were recorded in both the groups.
References
- Moore DC. Intercostal nerve block combined with celiac plexus (splanchnic) block. Regional Block. 4th edn. Springfield Ill: Charles C Thomas Publisher, 1981.
- Whiffler K. Coracoid Block: A safe and easy technique. Br J Anaesth 1981; 53:845-848.
- Cousins MJ, Bridenbaugh PO. Neural blockade in clinical anaesthesia and pain management. Philadelphia, Lippincott,1980.
- Desorches J. The infraclavicular brachial plexus block by the coracoid approach is clinically effective: An observational study of 150 patients. Can J Anesth 2003; 50:253-257.
- Wilson JL, Brown DL, Wongy GY. Infraclavicular brachial plexus block: Parasagittal anatomy important to the coracoid technique. Anesth Analg 1998; 87:870-873.
- Mageswaran R, Choy YC. Comparision of 0.5% ropivacaine and 0.5% levobupivacaine for infraclavicular brachial plexus block. Med J Malaysia 2010; 65:300-303.
- Chatrath V, Sharan R, Kheterpal R, et al. Comparative evaluation of 0.75% ropivacaine with clonidine and 0.5% bupivacaine with clonidine in infraclavicular brachial plexus block. Anesth Essays Res 2015; 9:189-194.
- Albrecht E, Vorobeichik L, Jacot-Gullarmod A, et al. Dexamethasone is superior to dexmedetomidine as a perineural adjunct for supraclavicular brachial plexus block: Systematic review and indirect metaanalysis. Anesth Analg 2019; 128:543-554.
- Albrecht E, Kern C, Kirkham KR. A systematic review and meta-analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia 2015; 70:71-83.
- Jaeger P, Grevstad U, Kosceilnaik-Neilsen ZJ, et al. Does dexamethasone have a perineural mechanism of action? A paired, blinded, randomized, controlled study in healthy volunteers. Br J Anaesth 2016; 117:635-641.
- Desmet M, Braems H, Reynvoet M, et al. IV and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: A prospective, randomized, placebo-controlled study. Br J Anaesth 2013; 111:445-452.
- Zorilla-Vaca A, Li J. Dexamethasone injected perineurally is more effective than administered intravenously for peripheral nerve blocks. Clin J Pain 2017; 65:1-7.
- Kim JH, Lee YS, Shin HW, et al. Effect of administration of ketorolac and local anaesthetic infiltration for pain relief after laparoscopic assisted vaginal hysterectomy. J Int Med Res 2005; 33:372-378.
- El-Hamid AM, Othman MSK. The effect of addition of local or intravenous ketorolac and morphine as an adjuvant to local anaesthetic in popliteal nerve block: A comparative study with epidural anaesthesia. Ain Shams J Anaesthesiol 2011; 4:40-56.
- Cepeda MS, Carr DB, Miranda N, et al. Comparision of morphine, ketorolac and their combination for postoperative pain: results from a large, randomized, double-blind trial. Anesthesiology 2005; 103:1225-32.
- Mirkheshti A, Saadatniaki A, Salimi A, et al. Effects of dexmedetomidine versus ketorolac as local anesthetic adjuvants on the onset and duration of infraclavicular brachial plexus block. Anesth Pain Med 2014; 4:17620.
- Kumar S, Palaria U, Sinha AK, et al. Comparative evaluation of ropivacaine and ropivacaine with dexamethasone in supraclavicular brachial plexus block for postoperative analgesia. Anesth Essays Res 2014; 8:202-208
- Elyazed MMA, Ghaffar MSA. Nitro-glycerine and ketorolac as an adjuvant to lidocaine for intravenous regional anaesthesia in patients undergoing forearm and hand surgery. AAMJ 2014; 12:159-176.
- Basenko IL, Tchuev PN, Budnyuk AA, et al. Use of ketorolac as adjuvant in brachial plexus block with bupivacaine. Europ J Anaesth 2006; 23:123.
- Paramaswamy R, Mahipathy SRV, Raj ARD, et al. Comparison of dexamethasone and ketorolac as an adjuvant to bupivacaine in axillary brachial plexus blocks for isolated hand and fore arm surgeries: A randomised double-blind Prospective study. J Clin Diag Res 2018; 12:5-9.
- Marty P, Bennis M, Legiallard B, et al. A new step toward evidence of in vivo perineural dexamethasone safety: An animal study. Reg Anesth Pain Med 2018; 43:180-185.
- Choi S, Rodseth R, McCartney CJL. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: A systematic review and meta-analysis of randomized trials. Br J Anesth 2014; 112:427-39.
- Heesen M, Klimek M, Imberger G et al. Co-administration of dexamethasone with peripheral nerve block: intravenous versus perineural application: systematic review, meta-analysis, meta-regression and trial sequential analysis. Br J Anesth 2018:120:212-227.
Author Info
Gudala Prasanna Kumar1 and Middepogu Yerra Sun Kanna2*
1Department of Anaesthesiology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India2Department of Anaesthesiology, Nimra Institute of Medical Sciences, Vijayawada, Andhra Pradesh, India
Citation: Gudala Prasanna Kumar, Middepogu Yerra Sun Kanna, To Compare the Efficacy of Dexamethasone Versus Ketorolac with Ropivacaine for Nerve Stimulator Guided Infraclavicular Brachial Plexus Block: A Prospective Randomised Comparative Study, J Res Med Dent Sci, 2019, 7(5):10-15.
Received: 29-Jul-2019 Accepted: 30-Aug-2019
