Research - (2022) Volume 10, Issue 12
Tomographical Determination of Uncommon Mandibular Canal Variations
*Correspondence: Zainab AH Al-Tamemi, College of Dentistry, University of Wasit, Wasit, Iraq, Email:
Abstract
Objective: Through the use of Cone-Beam Computed Tomography, the purpose of this descriptive study is to demonstrate an extremely uncommon mandibular canal variation (MCV), which presents as a right trifurcation and a left bifurcation. Method: This was a descriptive study of 120 cases of patients with no systemic disorders who presented with painful symptoms and were referred for surgical removal of the lower third molars as a treatment option. The patients' ages ranged from 26 to 52. In order to evaluate the relationship between the third molars and the mandibular canal and to direct the surgical planning, con beam computed tomography was requested. Results: The resulting data were used to conduct an analysis of the tomographic volume. During the course of the investigation of the tomographic sections, it was discovered that there was a bilateral furcation. A comparison is made between the bifurcation of the right MCV and the trifurcation of the left MCV. The results of the Cone-Beam Computed Tomography role in both of sides was below 0.05 of p. value, which indicates that it was significant. Conclusion: Cone-beam computed tomography was emphasized as an essential tool for the diagnosis of anatomical changes, such as MC bifurcation and trifurcation, thanks to the findings of the current study.
Keywords
Cone-beam computed tomography, Mandibular canal, Bifurcation, Trifurcation
Introduction
The vasculonervous bundle is composed of three different components: a nerve, an artery, and a vein. Each of these components is a part of the vasculonervous bundle [1]. The vasculonervous bundle travels through the mandibular canal, which is an anatomical structure that is present in both the ramus and the body of the mandible [2]. The ramus is the portion of the mandible that extends anteriorly, while the body of the mandible extends posteriorly [3]. Within the body of the mandible, the bundle of nerves and blood vessels passes through this canal on its way to various locations [4]. The mandibular canal extends all the way from the mandibular foramen to the mental foramen and includes both of these openings along its path [5]. These structures are accountable for sensations, the blood innervation of the mandibular teeth, the interdental papilla, as well as the periodontal and alveolar bone tissue, respectively [6]. Additionally, the interdental papilla can be found in this region of the mouth. Interdental papilla Variations in anatomy are possible at any point along the course of the mandibular canal. These variations, in conjunction with the technique that the operator utilizes, are the primary causes of failure in the inferior alveolar nerve anesthetic blockade [7]. In addition to this, there is the possibility that the inferior alveolar nerve will sustain damage, either temporary or permanent, during routine dental procedures that are carried out in close proximity to the nerve [8]. A bifid mandibular canal is the type of mandibular canal that occurs when, rather than just one branch coming off of the mandibular canal, there are two branches coming off of the mandibular canal. Even though a bifid mandibular canal is a relatively uncommon anatomical variation, it is still something that needs to be thoroughly examined. Studies that made use of panoramic images, on the other hand, have shown that the prevalence ranges anywhere from 1 to 15% of the population [9]. In spite of the fact that the prevalence of the bifid mandibular canal is not known, the prevalence of the bifid mandibular canal ranges from 1 to 15 percent. When panoramic radiographs are used for the examination, there is a possibility that the incidence of bifid mandibular canal will be underestimated [10]. This is because panoramic radiographs cover a larger area [11]. This is because panoramic radiographs are a type of examination that do not permit adequate visualization of all canals. As a result, this situation has arisen. Some of the studies used examinations in three dimensions (3D), and those studies found a higher prevalence, ranging from 30 to 50 percent. Other studies did not use 3D examinations. Another variation that is extremely uncommon and almost never reported is the presence of a third branch in the mandibular canal, which is also referred to as mandibular canal trifurcation [12]. In some circles, it is also referred to as the mandibular canal trifurcation [13]. This condition has not been mentioned in any of the previous classifications, despite the fact that the identification of an accessory mandibular canal is essential for the prevention of complications during surgical interventions in the mandible [14]. The identification of an accessory mandibular canal is essential for the prevention of complications during surgical interventions in the mandible. Cone-beam computed tomography, which is more commonly referred to as CBCT and stands for "cone-beam computed tomography," is currently finding widespread application in a variety of dental subspecialties [15]. This is largely attributable to the device's capacity to produce images in all three dimensions simultaneously (3D), [16]. When compared to the evaluation using panoramic radiography, the evaluation of bifid MC using CBCT reveals a higher incidence of the condition [17]. This is the case even though panoramic radiography was used for the evaluation. In addition, tomography makes it possible to observe the location of the canal in addition to its size, its course, and any branches it may have [18]. Tomography can also determine whether or not the canal has any branches [19]. The purpose of this research is to describe a rare variation of the mandibular canal that shows itself as a trifurcation on the right and a bifurcation on the left. This will be accomplished through the utilization of CBCT.
Material and Methods
Study design
The guidelines for academic responsibility served as the basis for this case study. Because she was experiencing painful symptoms, a patient in the age range of 28 to 45 years old who did not have any systemic disorders was referred for the surgical removal of her lower third molars. After noting the possibility of contact between the third molar and the mandibular canal variation, CBCT was requested to evaluate the relationship between third molars and mandibular canal variation and to direct the surgical planning.
Tomography
The examination was carried out with the assistance of a device known as an Orthophos XG 3D. The device had an average output of 85 kV and 8 mA, a field of view (FOV) that measured 8 cm x 4 cm, and a voxel that measured 0.5 mm. In order to conduct an analysis on the tomographic volume, the software known as Sidexis was utilized. When conducting the analysis of tomographic sections, it was possible to observe the presence of bilateral mandibular canal variation variations. This was possible to do so. An accessory branch was found in the right hemi mandible. It was located in a region that was posterior to the third molar. As seen in coronal and axial sections, this branch arrived at its destination, which was the retromolar position, at the end of its journey. As a direct consequence of this, the bifurcation of the mandibular canal variation took place at the retromolar position.
Additional observation
It was discovered that the left hemi mandible had an accessory canal that was situated in the retro molar position in the posterior region of the tooth. This discovery was made. Following the discovery of the primary mandibular canal, the researchers found this canal. It was found that there was a third branch that started posteriorly and moved downwards, moved posteriorly and below the retromolar canal, and terminated in the mesial root of the tooth. This branch was discovered after the tooth was extracted. This branch originated in a position superior to the main canal and inferior to the retromolar canal. This branch was located immediately above the main canal in its respective location. However, none of the earlier classifications make any mention of the fact that the mandibular canal divides into three distinct branches at various points along its length. These branches are located at various points along the canal's length. Before beginning the process of surgically removing the growth, the patient was given information regarding the proximity of the third molars to the mandibular canal variation as well as the risk of damage to the inferior alveolar nerve. This was done before the surgical removal of the growth could be planned. This was done in order to get the patient ready for the procedure that was going to take place later.
Results
View of tomography
When conducting the analysis of tomographic sections, it was possible to observe the presence of bilateral mandibular canal variation. This observation was made possible due to the presence of variations. The existence of variations allowed for the completion of this observation, which was previously thought to be impossible. This objective could have been achieved if one worked hard enough. It was found out that there is an accessory branch in the right hemimandible (Figure 1).
Figure 1: Bilateral mandibular canal variation in patient no. 3.
It occupied a spot on the right side of the mouth that was located behind the third molar of that side of the mouth. As can be seen in the coronal and axial sections that were taken at the conclusion of this branch's journey, it made it to its ultimate location, which was the retromolar position. This position was the endpoint of its journey. As a consequence of this, the variation of the mandibular canal took place at the position of the retromolar when it bifurcated. This was a direct result of the underlying cause in the first place (Figure 2).
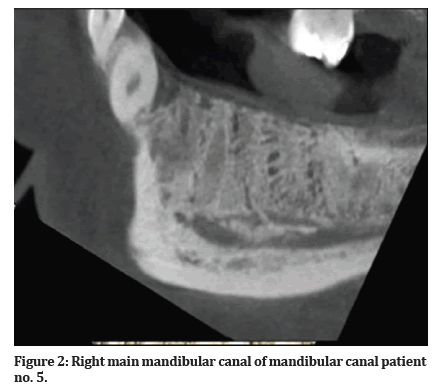
Figure 2: Right main mandibular canal of mandibular canal patient no. 5.
Accessory view indicated
It was found that the left hemimandible had an accessory canal that was located in the retromolar position in the posterior region of the tooth. This discovery was made after the tooth was prepared for root canal therapy. This finding was made available. After finding the primary mandibular canal, the researchers looked for any other possible canals and found this one. It was discovered that there was a third branch that began posteriorly and moved downwards, moved posteriorly and below the retromolar canal, and ended in the mesial root of the tooth (Figure 3).
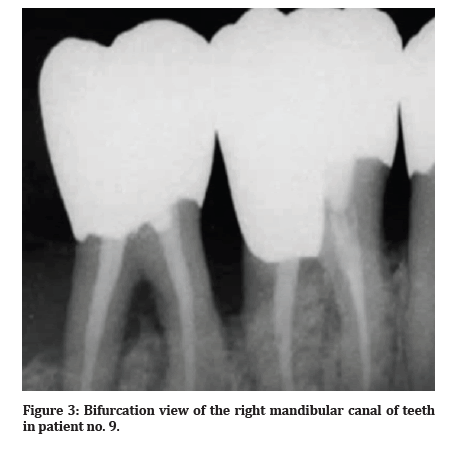
Figure 3:Bifurcation view of the right mandibular canal of teeth in patient no. 9.
This branch was located in the back of the tooth. Following the removal of the tooth, this branch was uncovered in the tree. This branch was formed in a location that was superior to the main canal and inferior to the retromolar canal when it first began. This branch was situated directly above the primary canal at its respective location in the landscape. Nevertheless, none of the earlier classifications make any reference to the fact that the mandibular canal splits into three separate branches at various points along its length. These splits take place at various points along the canal's length. These branches can be found at numerous points all the way along the length of the canal. Before beginning the process of surgically removing the growth, the patient was given information regarding the proximity of the third molars to the mandibular canal variation as well as the risk of damage to the inferior alveolar nerve (Figure 4).
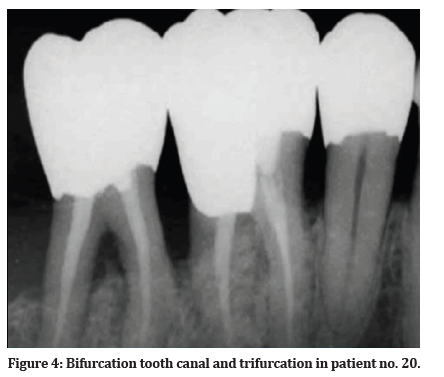
Figure 4:Bifurcation tooth canal and trifurcation in patient no. 20.
This was done before the process of surgically removing the growth could begin. This was carried out before the operative procedure to remove the growth could be organized. This was done so that the patient would be prepared for the procedure that was going to take place a little bit later.
Discussion
Panoramic imaging has been used in a number of research projects to evaluate the anatomical location and morphology of the bifid MC; however, 2D exams are not always able to correctly diagnose such variations [1]. CBCT is able to identify variations that are missed by orthopantomography [2]. The orthopantomographic examination did not uncover any irregularities in the mandibular canal [3]. The CBCT revealed that the patient had a variation in both the left mandibular canal trifurcation and the right mandibular canal bifurcation [4]. Surgeons have a significant amount of interest in the mandibular canals as a field of study [5]. The range of variation in the bifid mandibular canal found by tomographic research carried out in Brazil was found to be between 30.66 percent and 32 percent [6]. Studies done in the past have conclusively demonstrated that there is no link between the sexes and either bifid or multiple mandibular canals [7]. There was no discernible difference in the shape of the trifid mandibular canal between any of the one thousand radiographs [20]. The fact that a trifid mandibular canal was visible in only one of 550 CBCT images demonstrates how unusual of an occurrence it is. In order to identify variations in the mandibular canal [21–23], a systematic review and meta-analysis compared the diagnostic capabilities of panoramic x-rays and tomography [8]. Both of these imaging modalities provide three-dimensional images of the jaw [9]. Examinations in all three dimensions provide the most accurate diagnostic information [10]. You could be born with a single mandibular canal, a bifid mandibular canal, a unilateral mandibular canal, or even a bilateral mandibular canal [11]. There is no description of the variation of the mandibular canal that has three branches [12]. The majority of accessory canals have diameters that are approximately equivalent to 55% of that of the main mandibular canal [45 percent] [13]. This case report provided extensive details on both the plaintiff's and defendant's positions regarding the issue [14]. The findings of studies indicate that alterations to the right side of the mandibular canal occur more frequently [15]. It was reported that there was a difference on the left side of both of the sides. Examining the mandibular canal in addition to its lateral branches as part of the examination [16]. Variations in the mandibular canal can lead to the failure of an anesthetic blockade, a hemorrhage, a sensorineural disorder, a traumatic neuroma, or the loss of an implant [17]. Additionally, these variations can cause a sensorineural disorder and Oral surgery and implant dentistry both become more challenging as a result of the presence of mandibular canals [18]. In some of the studies, the positioning of the tooth 40 implant was determined by using a panoramic image. After the operation, the patient complained of painful symptoms caused by the implant [19,24,25]. CBCT was able to provide further evidence of the significance of anatomical mandibular canal variations and 3D examinations by demonstrating the presence of three accessory channels [26–28]. It is uncommon for patients to have a mandibular canal variation trifurcation because the condition has a low prevalence and most patients only get 2D exams [29–31]. CBCT was successful in locating a variation in the mandibular canal, which allowed for the surgical procedure to be planned [32].
Conclusion
This piece of research described a very uncommon occurrence of mandibular trifurcation, which was a significant and important contribution to the wider scientific community. This objective was successfully accomplished by the organization as a result of the contribution that it made to the scientific community as a whole. Cone beam computed tomography (CBCT) was shown to be an important tool for the accurate diagnosis of mandibular anatomical changes, as indicated by the results of this research project, which provided convincing evidence of this fact.
References
- Karthika B, Nisa S, Pavani M. Dental devices. In: Medical Devices. CRC Press 184–234.
- Ahmed J, Nath M, Sujir N, et al. Correlation of pericoronal radiolucency around impacted mandibular third molars using CBCT with histopathological diagnosis: A prospective study. Open Dent J 2022; 16.
- Niemczyk SP, Barnett F, Johnson JD, et al. Press and piezo microsurgery (Bony Lid): A 7-year evolution in a residency program part 1: Surgeon-defined site location. J Endod 2022.
- León-López M, Cabanillas-Balsera D, Martín-González J, et al. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int Endod J 2022; 55:1105-1127.
- Wu P. Improved image quality in cone-beam computed tomography for image-guided interventions. Doctoral dissertation, Johns Hopkins University 2022.
- Mishra R, Verma A, Rai S, et al. Advances in endodontics a complete guide. Book Rivers 2022.
- Tabakov S, Bregant P. Introduction to diagnostic radiology (X-Ray and computed tomography imaging). In: Introduction to Medical Physics. CRC Press 2022; 95–142.
- https://www.bib.irb.hr/1205165/download/1205165.J_Clinic_Periodontology_-_2022_-_-_Poster_Discussion.pdf
- Cheslerean-Boghiu T, Pfeiffer F, Lasser T. Task-specific performance prediction and acquisition optimization for anisotropic X-ray dark-field tomography. arXiv 2022.
- Özdemir O, Kopac T. Recent progress on the applications of nanomaterials and nano-characterization techniques in endodontics: A review. Materials 2022; 15:5109.
- https://scholarworks.rit.edu/cgi/viewcontent.cgi?article=12367&context=theses
- Scholey J, Vinas L, Kearney V, et al. Improved accuracy of relative electron density and proton stopping power ratio through CycleGAN machine learning. Phys Med Biol 2022; 67:105001.
- Kurukkal NS. Study of medical image data transformation techniques and compatibility analysis for 3D printing. Masters Thesis UIS 2022.
- Rusanov B, Hassan GM, Reynolds M, et al. Deep learning methods for enhancing cone-beam CT image quality toward adaptive radiation therapy: A systematic review. Med Phys 2022; 49:6019-6054.
- https://ir.library.oregonstate.edu/concern/graduate_thesis_or_dissertations/sj1399366
- Blaivas L, Tsung J, Corl K. Scientific research: Oral presentations. 2022 AIUM Award Winners. 2022; 41:1.
- Primidis T. Design and optimisation of ultra-compact, high-resolution, 3D X-ray imaging systems. Doctoral dissertation, University of Liverpool 2022.
- Alzahrani HMS. Characterisation of a novel radiation detector and demonstration of a novel error detection algorithm for application in radiotherapy. Doctoral dissertation, University College London 2022.
- https://e-archivo.uc3m.es/bitstream/handle/10016/34941/tesis_monica_garcia_sevilla_2022.pdf?sequence=1
- Ahmed AM, Jalil AT. Investigating the protective role of rhodanese enzyme against cyanide, the cytotoxic by-product of amygdalin. HDF and L929 cell lines. Lett Drug Des Discov 2022; 19.
- Alwan AM, Afzaljavan F, Tavakol Afshari J, et al. The impact of CYP19A1 variants and haplotypes on breast cancer risk, clinicopathological features and prognosis. Mol Genet genomic Med 2021; 9:e1705.
- Alwan AM, Afshari JT. In vivo growth inhibition of human caucasian prostate adenocarcinoma in nude mice induced by amygdalin with metabolic enzyme combinations. Biomed Res Int 2022; 2022.
- Alwan AM, Afshari JT, Afzaljavan F. Significance of the estrogen hormone and single nucleotide polymorphisms in the progression of breast cancer among female. Arch Razi Inst 2022; 77:943–958.
- Wang D, Qi Y, Wang Z, et al. Recent advances in animal models, diagnosis, and treatment of temporomandibular joint osteoarthritis. Tissue Eng Part B Rev 2022.
- Uzun Saylan BI, Akcali A, Tunali M. Treatment of gingival recessions using titanium platelet rich fibrin in combination with current approaches: Case series. J Clin Periodontol 2022; 9:4-54.
- Hartshorne J, Wertheimer M. Clear Aligner Therapy (CAT)–Ethical and dento-legal risk considerations. In Dent 2022; 12.
- Andresen AKH, Jonsson MV, Sulo G, et al. Radiographic features in 2D imaging as predictors for justified CBCT examinations of canine-induced root resorption. Dentomaxillofa Radiol 2022; 51:20210165.
- Miloševic D, Vodanovic M, Galic I, et al. Automated estimation of chronological age from panoramic dental X-ray images using deep learning. Expert Syst Appl 2022; 189:116038.
- Ganz SD. Utilization of three-dimensional imaging technology to enhance maxillofacial surgical applications. In: Peterson’s principles of oral and maxillofacial surgery. Springer 2022; 211–237.
- Palczewska-Komsa MP, Gapinski B, Nowicka A. The Influence of new bioactive materials on pulp–dentin complex regeneration in the assessment of Cone Bone Computed Tomography (CBCT) and Computed Micro-Tomography (Micro-CT) from a present and future perspective—A systematic review. J Clin Med 2022; 11:3091.
- Hamdan MH, Tuzova L, Mol A, et al. The effect of a deep-learning tool on dentists’ performances in detecting apical radiolucencies on periapical radiographs. Dentomaxillofac Radiol 2022; 51:20220122.
- Apostolakis D, Michelinakis G, Kamposiora P, et al. The current state of computer assisted orthognathic surgery: A narrative review. Computer assisted orthognathic surgery. J Dent 2022; 104052.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
College of Dentistry, University of Wasit, Wasit, IraqCitation: Zainab AH Al-Tamemi, Tomographical Determination of Uncommon Mandibular Canal Variations, J Res Med Dent Sci, 2022, 10 (12): 98-102.
Received: 07-Nov-2022, Manuscript No. jrmds-22-76495; , Pre QC No. jrmds-22-76495(PQ); Editor assigned: 07-Nov-2022, Pre QC No. jrmds-22-76495(PQ); Reviewed: 22-Nov-2022, QC No. jrmds-22-76495(Q); Revised: 25-Nov-2022, Manuscript No. jrmds-22-76495(R); Published: 02-Dec-2022
