Research - (2022) Volume 10, Issue 5
Total Aplasia of the Paranasal Sinuses: A Rare Presentation
Fahrettin Kalabalık1* and Emre Aytugar2
*Correspondence: Fahrettin Kalabalık, Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Sakarya University, Sakarya, Turkey, Email:
Abstract
Paranasal sinuses are air-filled cavities located within the bones around the nasal cavity. Abnormalities and anatomical variations of the paranasal sinuses are commonly seen. Various degrees and combinations of paranasal sinus aplasia and hypoplasia cases have been reported. However, very few cases of total paranasal sinus aplasia have been reported to date. We herein describe a total paranasal sinus aplasia case detected incidentally in a 22-year-old male patient without any disease affecting the skeletal system.
Keywords
Paranasal sinus, aplasia, hypoplasia, cone-beam computed tomography
Introduction
Paranasal sinuses are air-filled cavities located within the bones of the face and skull around the nasal cavity. They consist of the maxillary, frontal, and sphenoid sinuses, and the ethmoid air cells [1,2]. Paranasal sinuses develop as invaginations from the nasal fossae during the third and fourth fetal months. They undergo their major expansion after birth according to the development of the facial cranium and the teeth [3]. Although a variety of paranasal sinus anomalies have been reported in the literature, only few cases of total paranasal sinus aplasia have ever been reported [4-6].
We present a case of total paranasal sinus aplasia without any craniofacial anomaly or disease affecting the skeletal system, and the first ever case reported using cone-beam computed tomography (CBCT).
Case Report
A 22-year-old healthy male patient was referred from orthodontics clinic for 3D cephalometric analysis and 3D evaluation of impacted teeth. He had no previous history of either facial trauma or systemic diseases affecting the skeletal system. The patient’s previous panoramic and cephalometric radiographs were examined, and multiple impacted teeth were detected in both jaws. Moreover, there was a total lack of pneumatization in maxillary and frontal sinuses (Figures 1 and Figure 2). A CBCT (NewTom 5G; QR, Verona, Italy) scan was performed to determine the exact location of the impacted teeth and to confirm the aplasia of maxillary and frontal sinuses. Detailed examination of the CBCT images revealed that there were multiple impacted permanent teeth localized in different positions in the jaws. Further, there was a total lack of development or pneumatization of all paranasal sinuses (Figures 3-5). The patient was referred to medical genetics, endocrinology, and hematology clinics to investigate if he had any associated diseases or syndromic anomalies. As a result of laboratory examinations, no skeletal, systemic, or hematological abnormalities were detected in the patient.
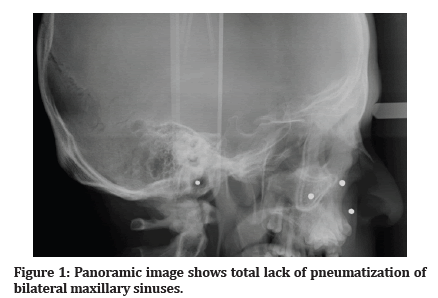
Figure 1: Panoramic image shows total lack of pneumatization of bilateral maxillary sinuses.
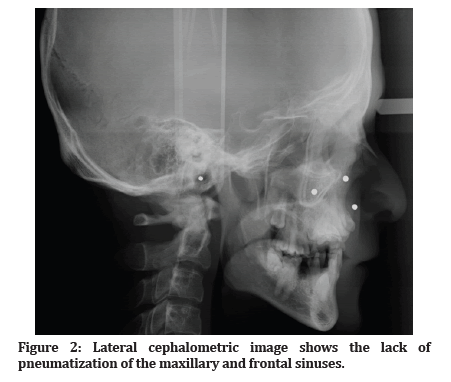
Figure 2: Lateral cephalometric image shows the lack of pneumatization of the maxillary and frontal sinuses.
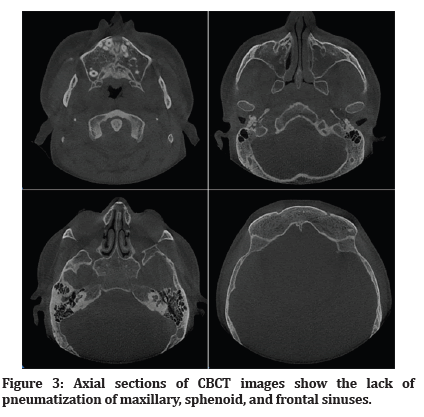
Figure 3: Axial sections of CBCT images show the lack of pneumatization of maxillary, sphenoid, and frontal sinuses.
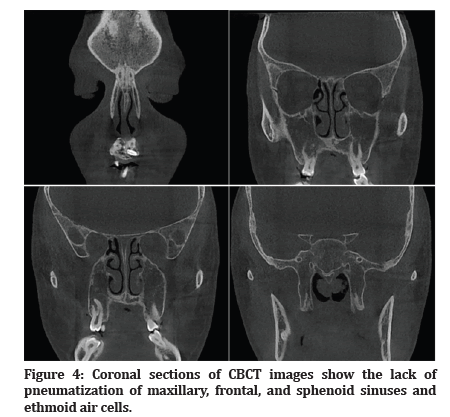
Figure 4:Coronal sections of CBCT images show the lack of pneumatization of maxillary, frontal, and sphenoid sinuses and ethmoid air cells.
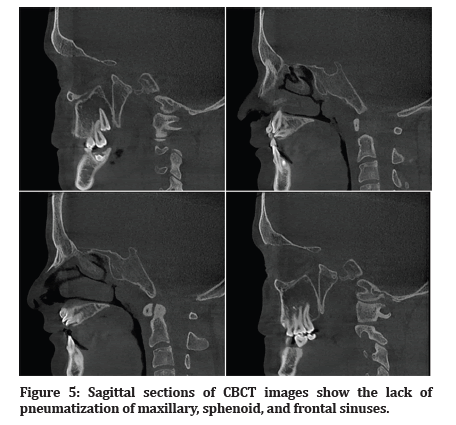
Figure 5:Sagittal sections of CBCT images show the lack of pneumatization of maxillary, sphenoid, and frontal sinuses.
Discussion
Development of the paranasal sinuses begins as an evagination of the nasal mucosa in 3rd to 4th month of intrauterine life and their expansion continues after birth throughout early adulthood [3,7]. At birth maxillary sinus and ethmoid air cells are present, while the frontal and sphenoid sinuses develop later in childhood. The maxillary sinus is the first paranasal sinus to develop during human fetal life [8]. By the age of 4 the maxillary sinus extends laterally past the infraorbital canal and by the age of 9 it reaches the maxillary bone. At birth, ethmoid cells are more developed anteriorly and pneumatization progresses in a posterior direction. Their growth lasts until late puberty. From as early as 2 years old pneumatization of the sphenoidal sinuses can be detected and by the age of 14 they reach their final size. After the age of 2, the frontal sinus which is the last paranasal sinus that undergoes major expansion, starts growing and reaches its final size after puberty [9].
Paranasal sinus pathologies and anatomic variations can be evaluated using different imaging modalities. CBCT is an exciting technology in the field of oral and maxillofacial radiology but is generally accepted as one of the pioneering imaging techniques for paranasal sinus evaluation by dentists, maxillofacial radiologists, and otolaryngologists [10,11]. CBCT image evaluation for the nasal cavity and paranasal sinuses provides many advantages, such as low radiation doses compared with computed tomography and low cost compared with magnetic resonance imaging [11].
Having the largest volume within the paranasal sinuses, the maxillary sinuses have a critical importance in dentistry because of their close proximity to the maxillary premolar and molar teeth [12]. Especially during the maxillofacial surgical procedures, osteotomies are performed on the lateral wall of the maxillary sinus in surgical interventions such as the Caldwell-Luc, Le Fort I osteotomy, and more often, in sinus floor elevation with the lateral window approach [13]. The maxillary sinuses are also prone to odontogenic infection, cyst and tumors of odontogenic origin [14].
Anatomical variations are commonly seen in the paranasal sinuses. Sphenoid sinus aplasia is a rare entity. The frequency of unilateral aplasia of frontal sinus was reported to be 15% and bilateral aplasia in 5% of adults [9]. While maxillary sinus hypoplasia is a well-known clinical entity, maxillary sinus aplasia is quite rare. In the literature, the prevalence of maxillary sinus hypoplasia was reported from 2.1% to 10.4% [15]. Total aplasia of paranasal sinuses is an extremely rare condition [6].
Although the causes of paranasal sinus anomalies are not fully understood, several other clinical syndromes are found to be associated with paranasal sinus hypoplasia and aplasia like Down’s syndrome, Crouzon syndrome, Treacher-Collins syndrome, Apert syndrome, osteodysplasia (Melnick-Needles), craniosynostosis, Paget’s disease, thalassemia, cystic fibrosis, and ciliary dyskinesia [4,16]. Pifferi et al. [17] reported a high prevalence of frontal and sphenoidal sinus aplasia or hypoplasia in patients with cystic fibrosis or primary ciliary dyskinesia. Therefore, in patients with paranasal sinus hypoplasia and aplasia, primary ciliary dyskinesia and cystic fibrosis should be considered and excluded [5]. The developmental pathologic abnormalities of the paranasal sinuses may be misdiagnosed as sinusitis or neoplasm. So, CT should be performed in suspicious cases [5,18].
There are few cases reported of total paranasal sinus aplasia in the literature. In a case presented by Celebi et al. [4] in 2012, total paranasal sinus aplasia was reported in a 35-year-old man whose complaints were fullness on the face and nasal obstruction. Korkmaz, et al. [5] reported a case of total paranasal sinus aplasia in a 57-year-old woman with complaints of nasal fullness and chronic headaches. Joshi et al. [6] reported a case of total paranasal sinus aplasia in a 15-¬year-¬old male with complaints of chronic frequent bilateral headache associated with facial fullness and frequent throat clearing habit. A case of total aplasia of the paranasal sinuses and nasal cavity in a 26-year-old male with complaints of nasal obstruction and mouth breathing since birth was presented by Hasan et al. [19]. Takaichi et al. [20] reported a case of total paranasal sinus aplasia with impacted teeth and no sinonasal symptoms. In our case, the patient was asymptomatic and total paranasal sinus aplasia was diagnosed incidentally as in the case presented by Takaichi et al. [20].
In conclusion, we present an extremely rare case with total paranasal sinus aplasia using CBCT. Awareness of the paranasal sinus anomalies is essential for an accurate surgical planning and to avoid complications during the procedure. Although CT is accepted as the gold standard in the evaluation of paranasal sinus pathologies and anatomical variations, CBCT can be preferred to CT for these purposes due to higher spatial resolution, lower patient dose, and lower cost.
References
- Aydinlioglu A, Kavakli A, Erdem S. Absence of frontal sinus in Turkish individuals. Yonsei Med J 2003; 44:215-8.
- de Oliveira AG, dos Santos Silveira O, et al. Anatomic variations of paranasal sinuses-clinical case report. Surg Radiol Anat 2013; 35:535-8.
- Hengerer AS. Embryologic development of the sinuses. Ear Nose Throat J 1984; 63:134-6.
- Celebi S, Taskin U, Altin F, et al. Bilateral aplasia of paranasal sinuses. Eur Arch Otorhinolaryngol 2012; 269:1055-7.
- Korkmaz H, Korkmaz M. Total aplasia of the paranasal sinuses. Allergy Rhinol 2013; 4:e105-9.
- Joshi A, Sundarray C, Sahoo KA. Bilateral total aplasia of paranasal sinuses: A rare case report. Clin Rhinol An Int J 2015; 8:124-126.
- Koertvelyessy T. Relationships between the frontal sinus and climatic conditions: A skeletal approach to cold adaptation. Am J Phys Anthropol 1972; 37:161-72.
- Wagenmann M, Naclerio RM. Anatomic and physiologic considerations in sinusitis. J Allergy Clin Immunol 1992; 90:419-23.
- Scuderi AJ, Harnsberger HR, Boyer RS. Pneumatization of the paranasal sinuses: normal features of importance to the accurate interpretation of CT scans and MR images. AJR Am J Roentgenol 1993; 160:1101-4.
- Langner S. Optimized imaging of the midface and orbits. GMS Curr Top Otorhinolaryngol Head Neck Surg 2015; 14:1-24.
- Ferreira LM, Nejaim Y, Freitas DQ, et al. The fundaments of CBCT and its use for evaluation of paranasal sinuses: Review of literature. Braz J Oral Sci 2017; e18038-e.
- Amorim Kde S, da Silva VT, da Cunha RS, Souto ML, et al. Removal of an upper third molar from the maxillary sinus. Case Rep Dent 2015; 2015:1-5.
- Pandharbale AA, Gadgil RM, Bhoosreddy AR, et al. Evaluation of the posterior superior alveolar artery using cone beam computed tomography. Pol J Radiol 2016; 81:606-10.
- Mehra P, Jeong D. Maxillary sinusitis of odontogenic origin. Curr Allergy Asthma Rep 2009; 9:238-43.
- Kaya M, Cankal F, Gumusok M, et al. Role of anatomic variations of paranasal sinuses on the prevalence of sinusitis: Computed tomography findings of 350 patients. Niger J Clin Pract 2017; 20:1481-8.
- Erdem T, Aktas D, Erdem G, et al. Maxillary sinus hypoplasia. Rhinology 2002; 40:150-153.
- Pifferi M, Bush A, Caramella D, et al. Agenesis of paranasal sinuses and nasal nitric oxide in primary ciliary dyskinesia. Eur Respir J 2011; 37:566-71.
- Tasar M, Cankal F, Bozlar U, et al. Bilateral maxillary sinus hypoplasia and aplasia: Radiological and clinical findings. Dentomaxillofac Radiol 2007; 36:412-5.
- Hasan TS. Total aplasia of the paranasal sinuses and nasal cavity: the first case report. Egypt J Otolaryngol 2022; 38:1-5.
- Takaichi M, Tomihara K, Terashima R, et al. Total paranasal sinus aplasia with multiple impacted teeth: A case report. J Oral Maxillofac Surg Med Pathol 2021; 33:158-60.
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Author Info
Fahrettin Kalabalık1* and Emre Aytugar2
1Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Sakarya University, Sakarya, Turkey2Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Izmir Katip Celebi University, İzmir, Turkey
Citation: Fahrettin Kalabalık, Emre Aytugar, Total Aplasia of the Paranasal Sinuses: A Rare Presentation, J Res Med Dent Sci, 2022, 10 (5):01-04.
Received: 22-Apr-2022, Manuscript No. JRMDS-22-61604; , Pre QC No. JRMDS-22-61604 (PQ); Editor assigned: 25-Apr-2022, Pre QC No. JRMDS-22-61604 (PQ); Reviewed: 10-May-2022, QC No. JRMDS-22-61604; Revised: 16-May-2022, Manuscript No. JRMDS-22-61604(R); Published: 23-May-2022
