Research - (2021) Volume 9, Issue 2
Treatment of Pediatric Mandibular Fractures Utilizing the Open Cap Splint: A Clinical Study
Ali Ahmed Abbood1* and Thair A. Lateef Hassan2
*Correspondence: Ali Ahmed Abbood, Senior resident maxillofacial surgery, Iraqi Board for Medical Specializtion, Iraq, Email:
Abstract
Background: Mandibular fracture in pediatric patients always presents a challenge with respect to their diagnosis and treatment. As this pediatrics is of a growing age, care should be taken so that later the overall growth pattern of the mandibular skeleton is not disturbed. Although, the incidence and distribution of in pediatric patient’s mandibular fractures is common, there are few reports about this type of trauma in Iraqi people. The aim of this study: To assess the efficiency of open cap splint and circumferential wires in the closed reduction as a treatment modality in mandibular fractures affecting children and teenagers. Materials and Methods: This was a prospective clinical study included 10 pediatric patients presented with mandibular fractures. The age of the patients was divided into two age groups, the first decade aged group for patients younger than 10 years and the second decade aged group is patients with 10-19 years. Both of them were managed using closed reduction with aid of open cap splint and circumferential wire. The descriptive analysis included percentages or the mean ± standard deviation (SD). All investigated variables were analyzed statistically using the chi-square test. Results: The patient’s age was ranged from 2-15 years with a mean of 6.7 years and a standard deviation (SD) of ± 3.6 years. Eight of the patients 80% were in the first decade of life, while the remaining two patients (20%) were in the second decade. Males in this study were higher than females (70% vs 30%) respectively with a male to female ratio of 2.33:1. The most common cause of injury for first decade age group was fall from height in 90% of cases, and the mostly affected site of fracture was the prarsymphyseal region (70%). The results of this study explained that 40% of patients presented with discomfort and 90% of them suffered from pain in the first week after surgery. Conclusion: Mandibular fractures in Pediatric patients reported most frequently in the first decade of life with male predominance. Falls was the most common cause of mandibular fractures. The incidence of mandibular fractures is high in the parasymphyseal region since it was the most affected site. The surgical treatment was indicated in all cases and no major complications encountered, the open cap splint proved to be satisfactory for the surgeon and patients. Most cases were managed using 2 circumferential wires, which was quite enough for effective fixation.
Keywords
Mandibular fractures, Pediatrics, Teenagers, Orthodontics, Circummandibular
Introduction
Pediatric patient’s fractures are unusual when compared with fractures in adults. The reasons for this statement are based primarily on social and anatomical factors. Most often children are in protected environments, under the supervision of parents and thus less exposed to major trauma, occupational accidents or interpersonal violence, which are common causes of mandibular fractures in adults [1]. The incidence of maxillofacial trauma is 3.3% in children age 15 years or younger. In pediatric patients mandibular fracture accounts for the 36% among all the facial fractures. Condylar fracture followed by the symphysis/parasymphysis fractures are the most common type of fractures in the children [2]. The incidence of mandibular fracture in pediatric patients ranges from 0.6% to 1.2%. The most typical causes of fracture in children were fall (64%), traffic incidents (22%), and sports-related accidents 9% [3]. The incidence of mandibular fractures is higher in boys than in girls worldwide and in all age groups. This male preponderance, which has remained constant over time, ranges from 1.1:1 to 8.5:1and has been attributed to greater and more dangerous physical activities among boys [4].
There are various techniques which were utilized in management of pediatric patients fractures like Tape Muzzles, Circumferential wiring, acrylic splint, percutaneous skeletal fixation, open reduction, resorbable plates, orthodontic resin, modified orthodontic brackets, rubber elastics in combination with orthodontics brackets, nickel titanium staples depending upon the minimally/severely displaced fractures [5]. The management of mandibular fracture differs in children when compared to adults because of the presence of the permanent tooth buds in the mandible.
Open reduction with rigid fixation is not commonly used in pediatric cases. Fracture of the mandible may be associated with or without loss of both hard and soft tissues depending on the severity of the injury. The goal of the treatment of these fractures is restore the bone architecture in a stable position as less invasively as possible to restore the function and esthetic impairment [6].
Closed reduction techniques with maxillomandibular fixation in very young children can pose several concerns, including cooperation, compliance and adequate nutritional intake [7].
Open cap splint is a simple, easy to fabricate and more reliable method. It has other advantages like ease of application and removal, less time consumption, cost-effectiveness, good stability during healing period and minimal trauma to surrounding tissues.
The height of contour in primary dentition is lower as compared to the permanent dentition which implies that the vertical height of the mandible is shorter [8]. In spite of warrants with using circummandibular wiring for acrylic support, increased elasticity of bone, thin and less dense mandibular cortex and the presence of tooth buds further sustain the use of circummandibular wiring [9].
Material and Methods
This was a prospective clinical study included (10) patients (7 boys and 3 girls) who had sustained isolated mandibular fracture and were treated at the Maxillofacial Surgery Unit of Al-Yarmouk Teaching Hospital during the period from January 2019 to June 2020.
Inclusion criteria
✓ Pediatric patients.
✓ The presence of fractures involving the body, parasymphysis, or symphysis, within period of one week of the original trauma.
✓ Patients who were available for follow up (with good compliance).
Exclusion criteria
✓ Mandibular fractures in adults & older mandibular fractures.
✓ Fracture of the angle and subcondylar regions.
✓ Comminuted, infected, and pathological fractures.
✓ Mandibular fracture in civilian or missile injury with considerable tissue loss.
✓ Patients with poor compliance.
Preoperative examination
Diagnosis of mandibular fractures was performed initially by taking history, clinical and radiographical examination. A detailed history was obtained from the patients or from parents, this included chief complaint, history of present injury and their surgical and medical history that may influence the healing process or may change the treatment plan.
General examination
Full examination of patients from out (top to toe examination) was carried. The purpose of general examination is to recognize the presence of other more serious injuries elsewhere in the body.
Local examination
Extraoral examination was initiated by careful inspection for any sign the of fracture such as swelling, deformity in the bony contour, inability to close the mouth or limitation of mouth opening, The mandible was carefully examined by palpation for the whole regions and the temporomandibular joint, with special attention to areas of point tenderness, as well as signs of neurosensory deficit such as anesthesia or paresthesia of the lower lip or mental region was recorded (Figure 1).

Figure 1. A patient with mandibular fracture presented with swelling on the right side of face.
Intraorally the occlusion was examined, for the presence of any disturbance and lacerations of gingival areas were examined. In addition any area of ecchymosis in the lingual and buccal sulci and floor of the mouth was carefully evaluated. The oral cavity was examined for any tooth mobility or fracture, and the condition of the teeth in the fracture line was carefully examined (Figure 2).
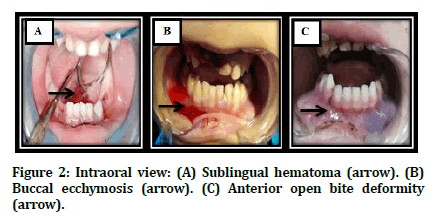
Figure 2. Intraoral view: (A) Sublingual hematoma (arrow). (B) Buccal ecchymosis (arrow). (C) Anterior open bite deformity (arrow).
For suspected fracture area a bimanual palpation was performed to test the mobility of the fracture, this was achieved by placing firm pressure over the mandible posterior and anterior to the fracture area in an attempt to elicit mobility in this area. After careful examination, an element of doubt still exists about the presence of mandibular fracture, a compression test may be applied.
Radiographical examination
In order to confirm the diagnosis, radiographical investigation was requested. For all the patients orthopantomogragh OPG and posterioanterior radiograph (PA) were obtained as illustrated in Figure 3.
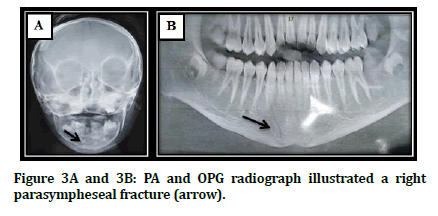
Figure 3A and 3B: PA and OPG radiograph illustrated a right parasympheseal fracture (arrow).
Fabrication of the splint
Impressions were taken, and casts poured and sectioned to the desired mandibular position using the upper cast as a guide. The two pieces were then stuck together with sticky wax. An open acrylic splint was fabricated using clear hot cured acrylic resin. The color of the splint was clear to show any pressure areas on the soft tissue Figure 4.
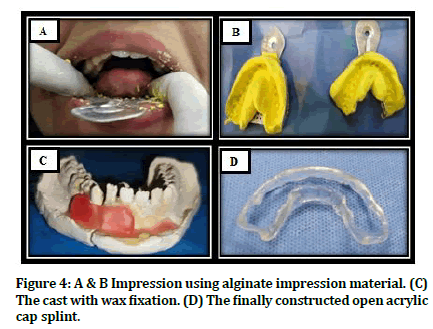
Figure 4: A & B Impression using alginate impression material. (C) The cast with wax fixation. (D) The finally constructed open acrylic cap splint.
Surgical procedure
Prior to surgery. The patients were given prophylactic regime (500) mg ceftriaxone vial. for the patients under 10 years and (1000) mg for the patients more than 10 years. Surgery was performed under general anesthesia for all patients.
After preparation of the patient, the patient irrigation with normal saline solution was done to clean surgical field. The displaced segments were reduced by bidigital pressure with the guidance of the surgical splint. Awl was introduced guided along the body of the mandible and taken out lingually. The wire was tied in and the awl end gently guided along the lower border of the mandible and passed into the buccal sulcus. The wire was held together and sawing was done to adapt the wire in close approximation to the bone. This also prevents soft tissue injury and avoid undesirable scar. The open acrylic cap splint was then stabilized on the right side by winding the wire in a clockwise direction. The same procedure was followed on the other side. Care was taken to avoid pulling the wire through the mandible since this stage the mandibular cortex is thin and relatively less dense, after that cut the access of bending wire Figure 5.
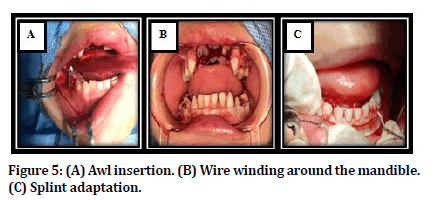
Figure 5. (A) Awl insertion. (B) Wire winding around the mandible. (C) Splint adaptation.
Postoperative care and follow up
An OPG radiograph was taken one week after surgery to check if the wires were properly secured to bone. Postoperative antibiotic coverage was started for one week. The patient instructed for soft diet, avoidance of physical activities, and antibacterial mouth rinse was prescribed. Postoperative monitoring was performed on a weekly for (24 weeks) basis and was favorable in both healing and function the interdental wiring and acrylic splint were removed after 3 weeks under local anesthesia.
Results
The total number of pediatric patients included in this study was 10 suffered from mandibular fracture in three different sites (symphseal, parasymphseal and body). All of them were treated by closed reduction utilizing open acrylic cap splint and circumferential wires.
The patient’s age in this study ranged from 2-15 years with a mean of 6.7 years and a standard deviation (SD) of ± 3.6 years. Eight of the patients (80%) were in the first decade (0-9 year), while the remaining two patients (20%) were in the second decade (10-19 year). The proportion of boys was higher than girls (70% vs 30%) respectively with a male to female ratio of 2.33:1.
Ninety percent of fractures resulted from fall from height and the results reported 7 (70%) of patient’s fractures were in the parasymphyseal region.
The descriptive statistics corresponding to the number of circumferential wires required for each patient demonstrated that 9 (90%) of patients were treated by closed reduction utilizing open cap splint and two circumferential wires. The results of this study reported that 40% of patients presented with discomfort. Concerning the oral hygiene data, the prominent figure (70%) was fair. On the other hand, 80% of them developed gingivitis, and only 90% had pain 1st week postoperatively.
There was no statistical significant association (P > 0.05) between age and discomfort of the patients. The highest prevalence of discomfort (80%) was observed in patients aged 1st decade.
In term of gender distribution, there was no statistical significant effect (P ≥ 0.05) between patients discomfort and gender, as shown in Table 1. Table 2 register no statistical significant difference (P ≥ 0.05) between patient discomfort and different fracture sites.
| Variable | Discomfort | Total (%) (10) | P - Value | |
|---|---|---|---|---|
| Yes (%) (4) | No (%) (6) | |||
| Age (Years) | ||||
| 1st decade (0-9) | 4 (40) | 4 (40) | 8 (80.0) | 0.19 |
| 2nd decade (10-19) | 0 | 2 (20.0) | 2 (20.0) | |
| Gender | ||||
| Male | 4 (40) | 3 (30) | 7 (70.0) | 0.091 |
| Female | 0 (0) | 3 (30) | 3 (30.0) | |
Table 1: Association between discomfort and demographic data.
| Variable | Discomfort | Total (%) (10) | P - Value | |
|---|---|---|---|---|
| Yes (%) (4) | No (%) (6) | |||
| Fracture Site | ||||
| Parasymphysis | 2 (20) | 5 (50) | 7 (70) | 0.375 |
| Symphysis | 1 (10) | 0 (0) | 1 (10) | |
| Body | 1 (10) | 1 (10) | 2 (20) | |
Table 2: Comparison of patient discomfort with different fracture sites.
The chi-square test used for testing the significance of postoperative pain with demographic data. The results illustrated that there was significant association between 1st week postoperative pain and age decades (P < 0.05). On the other hand, no significant correlation between pain and gender data in this study, as demonstrated in Table 3.
| Variable | Pain (1st week postoperatively) | Total (%) (10) | P - Value | |
|---|---|---|---|---|
| Yes (%) (9) | No (%) (1) | |||
| Age (Years) | ||||
| 1st decade (0-9) | 8 (80.0) | 0 (0) | 8 (80.0) | 0.03 |
| 2nd decade (10-19) | 1 (10.0) | 1 (10.0) | 2 (20.0) | |
| Gender | ||||
| Male | 7 (70) | 0 (0) | 7 (70) | 0.107 |
| Female | 2 (20) | 1 (10) | 3 (30) | |
Table 3: Comparison of patient discomfort with different fracture sites.
All the 10 patients had a follow-up period of 6 months, and none of them had any major complications (malunion, malocclusion, TMJFigure problems. Postoperatively, there was satisfactory healing and union of fracture fragments in all patients. With regard to wire placement and removal, none of the patients had any obvious swellings postoperatively. The 6-month followup good occlusion, without interference with teeth eruption.
Discussion
In this research, the age of patients ranged from 2-15 years with a mean of 6.7, this may be contributed to the facts that the children in this age started in the first year to walk and increased susceptibility to fall, attending schools, unsupervised physical activity, road traffic accidents and sport activities which may increase the incidence of fractures. The study reported that 80% of the patients were in the first decade of life, this is in the same line with Kale et al., 2011 [10] and Shehzadi et al., 2018 [11] who registered that the age of patients ranged from (1.5-11) years with a mean of 6 years and most fracture happened in first decade of life (90%). On the other hand, this study was in disagreement with Felts & Christian, 2019 [12] who reported in their study that the largest proportion of fractures (55%) seen in patients with age group ranged from 13-17 (the second decade) due to assault followed by 31% and 14% in patients age group ranged (5-12 and 0-4) respectively due to motor vehicle accident and fall from height. While, in this research the most common etiological factor of fracture was fall from height 90%.
Regarding gender, the present study confirmed that males children were affected more than twice than females (ratio of 2.33:1). The probabilistic interpretation for this ratio may be borrowed from Munante-Cardenas et al., 2010 [13] and Zimmermann et al., 2006 [14] who registered a male/female ratio of fractures (ranging 2.1:1 to 3.1:1) and stated that the predominance of males returned to their violent social and hyperkinetic activity. Also, because of cultural condition which made the males being found in outdoors more than females and this powered by Ashrafullah et al., 2018 [15]. In contrast, Felts & Christian, 2019 [12] found that motor vehicle accidents was most common overall in females.
In the current study, the parasymphyseal fracture was the dominant one (70%) probably due to the presence of permanent teeth buds in the pediatric mandible presenting a high tooth to bone ratio. And this is supported by Vyas et al., 2014 [16] who found that 32.4% of fractures in the parasymphyseal region. This went with Kale et al., 2011 [10] and Ashrafullah et al., 2018 [15] who stated that the parasymphysis was the most commonly affected site in the mandible (90%).
This interpretation does not correspond with Ferreira et al., 2004 [17] and Glazer et al., 2011 [18] who observed that the condylar fractures (31%) was more common than the parasymphysis one (13.1%) in pediatric age group due to thin cortices, along with high amount of medullary bone which poorly resistant to impact force during falls.
In this research, 90% were fixed by two circumferential wires. In most cases, 2 wires was sufficient for adequate reduction and fixation and to increase the stability and strength of open cap splint. This is powered by Nezam et al.,2018 [19] and Agnihotri et al.,2015 [9] who used in their studies also two circumferential wires. On the other hand, 10% of splints were stabilized by three circumferential wires. This result was supported by Sezer et al.,2010 [7] who involved three circumferential wires in their study.
The results of the present study demonstrated that 40% of the patients presented with discomfort and 70% with fair oral hygiene from the time of operation until the removal of the splint 3 weeks after surgery.
The proposed explanation behind this may be related to the advantage of open cap splints over the traditional one which include tooth to tooth contact so as to facilitate occlusion guided reduction, preservation of periodontal tissue integrity and oral hygiene and this supported by Bhola et al., 2013 [20] who advocated that the use of open cap splint maintain reasonable oral hygiene.
Also, Jain et al., 2015 [21] and Khatri & Kalra, 2011 [22] claimed that the open cap splint was less traumatic to the adjacent anatomic structures, easy to apply and remove, safe to use in all age group, less discomfort to children, and low cost to the patient.
Concerning the results that 80% of patients developed gingivitis from the time of operation until the removal of the splint 3 weeks following surgery, this may be attributed to that the young age group included in this study that cannot preserve good oral hygiene without the assistance of their parents, also the fear of patients from teeth brushing during the healing period and the awareness and educational level of the patients or parents.
No intraoperative complications were recognized in this study such as hemorrhage, or damage to the adjacent teeth. Nine (90%) of patients presented with pain during the first week of follow-up this may be contributed to the nature of fracture (simple or compound) with no or minimal displacement.
In addition to that the use of closed reduction made complications being absent compared with ORIF that may cause many problems such as trauma to tooth buds, need for nonresorbable plate removal, risk of migration of plates, infection, and nerve injury.
This study is agreement with the finding of another study done by Bhola et al., 2013 [20] on 10 patients from (5-9 years) who found only one patient suffered from infection. Kale et al., 2011 [10] reported that the complications with open cap splint were very rare when checked good occlusion after placement of the appliance, maintenance of good oral hygiene, the TMJ not restricted and keep stable dentition. Yuvaraj et al., 2011 [23] encountered tear in floor of mouth resulting in hematoma in 3 out of 22 (13.6%) pediatric patients, but in this study none of the patients developed postoperative hematoma.
All patients participated in this study were satisfied depending on the patients or parent’s own words in the follow up period and approved the final outcome after the completion of management and study period. This was in agreement with another study done by Shrutha et al. [24] in which they found the pure joy and satisfaction derived after treating of the children is unparalleled.
Conclusion
Despite the limitations, the present study led to the following conclusions: No major complications encountered in this study, The open cap splint proved to be satisfactory for the surgeon and the patients, In most cases 2 circumferential wire were quite enough for adequate fixation.
References
- Maranoa R, Netoa PO, Sakugawab KO, et al. Mandibular fractures in children under 3 years: A rare case report. Rev Port Estomatol Med Dent Cir Maxilofac 2013; 54:166–170.
- Boffano P, Roccia F, Zavattero E, et al. European maxillofacial trauma (EURMAT) in children: A multicenter and prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 119:499–504.
- Agrawal RM, Yeluri R, Singh C, et al. Management of pediatric mandibular fracture: A case series. Compend Contin Educ Dent 2014; 35:578-82.
- Khairwa A, Bhat M, Sharma A, et al. Management of symphysis and parasymphysis mandibular fractures in children treated with maclennan splint: Stability and early results. Int J Clin Pediatr Dent 2015; 8:127-132.
- Madan N, Bajaj N. Conservative treatment of pediatric mandibular fracture with removable acrylic splint. Indian Dent Sci 2010; 2:22–24.
- John B, John R, Stalin A, et al. Management of mandibular body fracture in pediatric patients: a case report with review of literature. Contemporary Clin Dent 2013; 1:291–296.
- Sezer B, Koyuncu B, Akay C, et al. Splint fixation with circummandibular wires for pediatric mandibular fracture: Two case reports. J Ege University School Dent 2010; 3:113-117.
- Adlakha V, Bansal V, Chandna P, et al. Mandibular fracture in an 18 month old child. Indian J Dent Res 2011; 22:723-725.
- Agnihotri A, Agnihotri D, Dwivedi D, et al. Management of pediatric mandibular fracture using acrylic cap splint & cap splint & circummandibular wiring-A report of 12 cases. Int J Orthop Traumatol Surg Sci 2015; 1:16-19.
- Kale TP, Urologin SB, Kapoor A, et al. Open cap splint with circummandibular wiring for management of pediatric mandibular parasymphysis/symphysis fracture as a definitive treatment modality: A case series. Dent Traumatol 2013; 29:410-415.
- Shehzadi C, Riaz N, Zulfiqar R. Retrospective study of 2,536 mandibular fractures in different ages over a period of 9-year. Dent Sci 2018; 17:2155-2160.
- Felts C, Christian JM. Pediatric mandible fractures at a level 1 trauma center: A 10-year retrospective study. J Dent Forecast Sci Forecast Publications 2019; 2:1- 4.
- Munante-Cardenas, Moraes L, De M, et al. Mandibular fractures in a group of Brazilian subjects under 18 years of age: A epidemiological analysis. Int J Pediatr Otorhinolaryngol 2010; 74:1276-80.
- Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int. J Oral Maxillofac Surg 2006; 35:2-13.
- Ashrafullah Pandey RK, Mishra A. The incidence of facial injuries in children in Indian population: A retrospective study. J Oral Bio Craniofac Res 2018; 8:82-85.
- Vyas A, Mazumdar U, Purohit C. A study of mandibular fractures over a 5-year period of time: A retrospective study. Contemporary Clin Dent 2014; 5:452-455.
- Ferreira PC, Amarante JM, Silva AC, et al. Etiology and patterns of pediatric mandibular fractures in Portugal: A retrospective study of 10 years. J Craniofac Surg 2004; 15:384–91.
- Glazer M, Joshua BZ, Woldenberg Y, et al. Mandibular fractures in children: Analysis of 61 cases and review of the literature. Int J Pediatr Otorhinolaryngol 2011; 75:62–64.
- Nezam S, Kumar A, Shukla J, et al. Management of mandibular fracture in pediatric patient. Natl J Maxillofac Surg 2018; 9:106–109.
- Bhola N, Jadhav A, Borle R, et al. Lateral compression open cap splint with circummandibular wiring for management of pediatric mandibular fractures: A retrospective audit of 10 cases. Oral Maxillofac Surg 2013; 18:65-8.
- Jain P, Yeluri R, Gupta S, et al. Management of pediatric mandibular parasymphyeal fracture with acrylic closed cap splint: A case report. Annals Dent Specialty 2015; 3:45-47.
- Khatri A, Kalra N. A conservative approach to pediatric mandibular fracture management: Outcome and advantages. Indian J Dent Res 2011; 22:873.
- Yuvaraj V, Thomas S, Singh D, et al. Awl versus intravenous cannula stillete in circummandibular wiring–A prospective comparative study. Oral Maxillofac Surg 2011; 15:21-25.
- Shrutha SP, Vinit GB. Circummandibular wiring in pediatric maxillofacial trauma: A case report. Annals Essences Dent 2011; 3:32-34.
Author Info
Ali Ahmed Abbood1* and Thair A. Lateef Hassan2
1Senior resident maxillofacial surgery, Iraqi Board for Medical Specializtion, Iraq2President of the Iraqi Scientific Council of Maxillofacial Surgery in Iraqi Board for Medical Specializtion, Iraq
Citation: Ali Ahmed Abbood, Thair A. Lateef Hassan, Treatment of Pediatric Mandibular Fractures Utilizing the Open Cap Splint: A Clinical Study, J Res Med Dent Sci, 2021, 9 (2): 36-42.
Received: 02-Jan-2021 Accepted: 20-Jan-2021
