Research - (2022) Volume 10, Issue 4
Treatment of Pyogenic Granuloma with Diode Laser
*Correspondence: Aya A Majeed, Department of Biomedical Application, Laser Institute for Postgraduate Studies, University of Baghdad, Iraq, Email:
Abstract
Background: Pyogenic granuloma (PG) is a well-known oral benign growth. The most frequent intra-oral site is marginal gingiva. It is often arises in the second decade of life, mostly bleeds on simple probing and that has a strong tendency to recur after simple excision. The aim of study: to assess the therapeutic benefits of diode laser (810-980 nm) in treatment of oral pyogenic granuloma. Materials and Method: A total of 14 patients (7 males, 7 females) were enrolled in this study and had their pyogenic granuloma laser removed. All of the patients underwent the identical surgical procedure, which was performed under local anesthetic (cartridge containing 1 percent lidocaine with epinephrine 1:100.000). To achieve coagulation and prevent bleeding, the lesions were meticulously sliced by moving the laser fiber tip in a sweeping manner on the surgical site. The wounds were not sutured to allow them to heal. Thereafter, the specimens sent for histopathological purposes. Results & Conclusions: In most cases pain, bleeding and oedema were completely disappeared after second visit. The patient satisfaction and function improved after second visit.it seems that poor oral hygiene and poor fitting denture may lead to recurrence. The treatment of pyogenic granuloma with diode laser (810-980 nm) is safe, effective and reasonable alternative to conventional surgical therapy.
Keywords
Pyogenic granuloma, Diode laser, Benign tumor, Laser surgery, Oral lesion
Introduction
Pyogenic granuloma is a hemorrhagic nodule that develops on the gingiva (but can develop on any surface) as a result of long-term, mild local irritants. It arises as a result of connective tissue fibro vascular growth [1]. It manifests clinically as little red erythematous papules with a sessile or pedunculated base. The size varies in diameter from a few millimeters to few centimeters [2,3]. Depending on the extent of vascularity, the color of the lesion may change [3]. It comes in a variety of colors, from pink to red to purple. Young PGs have more vascularity and hyperplastic granulation tissue than older PGs, whereas older PGs have more collagen. To avoid recurrence, local irritants and other stressful elements must be reduced [2].
It was shown that PGs are found in 44.4%–83% of oral cavity gum. However, it also has been reported in the literature to occur in the lingual, buccal and palatal mucosa [4,5]. It may be encountered in different parts of the body outside of the oral cavity, such as the lips, nose, fingers and toes. PG can be seen in patients of any age; however, it is more common in those aged between 10 and 40 years. In young adult females, it is predominant in the second decade of life. Potential reasons for this may be the vascular effects of female sex hormones [6-8]. The study aimed to evaluate the therapeutic advantages of diode laser (810-980 nm) in treatment of Oral Pyogenic Granuloma.
Material and Methods
A total of 14 patients (7 male, 7 female) had been enrolled in this study subjected to laser excision of pyogenic granuloma ,presenting intraoral dull red, sessile, or pedunculated smooth surfaced nodule that may easily bleed on simple probing, and sizes ranging from a few millimeters to a few centimeters have been reported . Prior to surgery, a patient consent form was collected, and the operation was thoroughly explained to the patient. Patient demographics include age, gender, medical history, and a clinical assessment of the lesion. Oral prophylaxis was provided by preoperative intraoral antisepsis with Listerine mouthwash for around 30 seconds, and patients and surgical teams were required to wear safety goggles to protect their eyes. The lesions were excised in one piece using a Diode laser with a wavelength of 810-980 nm and a power of 0.8W in continuous wave mode with a fiber optic delivery system. All of the patients underwent the identical surgical procedure, which was performed under local anesthetic (cartridge containing 1 percent lidocaine with epinephrine 1:100.000). To achieve coagulation and prevent bleeding, the lesions were meticulously sliced by moving the laser fiber tip in a sweeping manner on the surgical site. The wounds were not sutured to allow them to heal. After that, the specimens were preserved in a 10% formaldehyde solution for histological examination. Ciprofloxacin (ciprodar) Tab 250mg, Metronidazol (Flagyl) Tab 500mg, Mefanamic acid (Ponistan) Cap. 250mg as analgesic, Listerine Mouth Wash were utilized as treatment regimen (Figure 1).
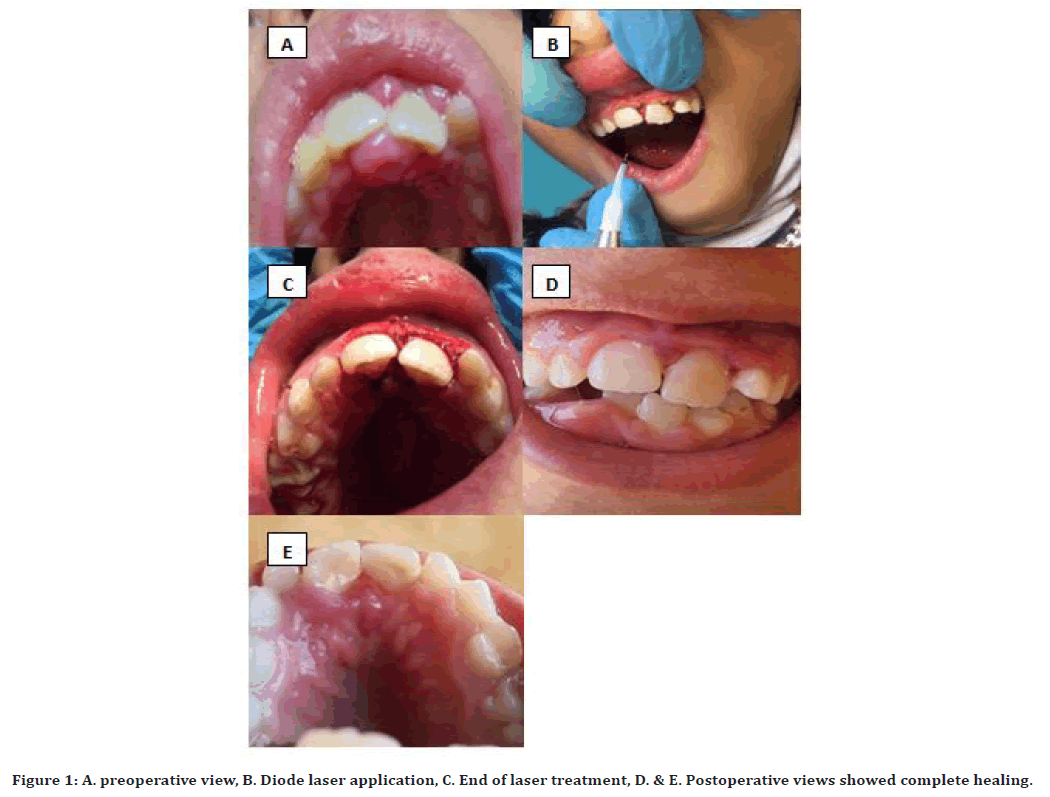
Figure 1. A. preoperative view, B. Diode laser application, C. End of laser treatment, D. & E. Postoperative views showed complete healing.
Statistical analysis
Data were introduced into SPSS V26 statistical program, tables and graphs were used to present descriptive statistics. While Friedman test was used to measure the improvement in the study dependent parameters, P value< 0.05 was considered as cuttof point of significance.
Results
A total of 14 patients (7 female & 7 male) had been enrolled in this study undergone surgical excision of pyogenic granuloma by diode laser (810-980nm) aged from 10-45years old. The results of this cross sectional study shows that 14 cases were involved , 35.7% of them were in adolescent age while 64.3% were in adult age group, 50% of studied patients were males. Regarding educational level 28.6%, 21.4% and 50% achieved primary, secondary and university level of education and 35.7% got the disease before less than 3 months (Table 1).
| Count | Column N % | ||
|---|---|---|---|
| Age | <18 year | 5 | 35.70% |
| =>18 years | 9 | 64.30% | |
| Gender | Male | 7 | 50.00% |
| Female | 7 | 50.00% | |
| Education | Primary | 4 | 28.60% |
| Seconary | 3 | 21.40% | |
| University | 7 | 50.00% | |
| Duration | <3 month | 5 | 35.70% |
| =>3month | 9 | 64.30% |
Table 1: Distribution of studied cases according to essential characteristics.
Table 2 shows that the level of pain, edema and bleeding were significantly decreased in median and mean ranks of pain, edema and bleeding, according to friedman test, p value ≤ 0.05 in all conditions. Satisfaction and function level were found to be steady and significantly incased across different stages of study. P value <0.01 in both conditions.
| Median | IQR | Mean rank | P Value | ||
|---|---|---|---|---|---|
| Pain | 1ST | 1 | 0.25 | 3 | 0.001 |
| 2ND | 0 | 0 | 1.57 | ||
| 3RD | 0 | 0 | 1.43 | ||
| Edema | 1ST | 1 | 0.25 | 3 | 0.001 |
| 2ND | 0 | 0 | 1.57 | ||
| 3RD | 0 | 0 | 1.43 | ||
| Bleeding | 1ST | 0 | 0.25 | 2.21 | 0.05 |
| 2ND | 0 | 0 | 1.89 | ||
| 3RD | 0 | 0 | 1.89 | ||
| Satisfaction | 1ST | 1 | 0.25 | 1.21 | 0.001 |
| 2ND | 2 | 1 | 1.96 | ||
| 3RD | 2 | 1 | 2.82 | ||
| Function | 1ST | 1 | 1.25 | 1.18 | 0.001 |
| 2ND | 2 | 1 | 2.04 | ||
| 3RD | 2 | 0.25 | 2.79 |
Table 2: Friedman Test shows differences in pain, edema, bleeding, patient’s satisfaction and function across different stages of study.
Table 3 shows that Recurrence was noticed in second case when pain, bleeding and edema were noticed at time of 4th visit, after it has been disappeared at 2nd and 3rd visit just like other 13 patients lesions, this case was 45 year female employed position who had primary level of education and she was putting poorly fitted denture with multiple manipulation and fitting trials.
| Pain | Edema | Bleeding | Satisfaction | Function | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R1 | R2 | R3 | R4 | R1 | R2 | R3 | R4 | R1 | R2 | R3 | R4 | R1 | R2 | R3 | R4 | R1 | R2 | R3 | R4 | |
| 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| 2 | 2 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 2 | 2 | 0 | 1 | 2 | 2 | 0 |
| 3 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 3 | 3 | 2 | 2 | 3 | 3 |
| 4 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| 5 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | 2 | 0 | 1 | 2 | 2 |
| 6 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | 2 | 0 | 1 | 2 | 2 |
| 7 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 2 | 3 | 1 | 2 | 2 | 3 |
| 8 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 3 | 3 | 1 | 2 | 2 | 3 |
| 9 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 2 | 3 | 2 | 1 | 2 | 3 |
| 10 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
| 11 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
| 12 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 2 | 3 | 1 | 2 | 2 | 3 |
| 13 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 2 | 3 | 1 | 2 | 2 | 3 |
| 14 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
Table 3: Distribution of studied patients according to scores of measured variables according to time of measurements of each patient.
Discussion
Oral pyogenic granuloma can appear at any time during a person's life. The majority of the cases collected manifested as a mass [9,10], with ulceration on the lesion's surface and a pedunculated base. In this study, pain, bleeding and oedema completely disappeared in most cases at second visit, regarding to patients satisfaction and function also improved at second visit. one case only undergo recurrence due to poor oral hygiene and poor fitting partial denture.
Short duration oral pyogenic granuloma much more easily bleed as a result of less collagen fibers as well as high vascularity; in contrast the older lesion have more collagen and less vasculature [11,12]. The socioeconomic status and oral hygiene practice play an important role in the growth of the lesion. The sizes of the oral pyogenic granuloma lesions in this investigation ranged from (0.5-2.5) cm. Simple surgical excision of the oral pyogenic granuloma by diode laser 810-980 nm bonded to the lesion base, encompassing around (2 mm) of the surrounding healthy tissue It is critical to monitor treated individuals to verify that there are no signs of recurrence in cases where surgery was performed. Recurrence was attributed to inadequate lesion removal as well as causative agents’ persistence [10,12,13] thus; (2 mm) of the surrounded normal health tissue was ablated to have good prognosis.
Histopathological examination of the excised pyogenic granulomas demonstrated infiltration of vascular granulation tissue with inflammatory cells and macrophages, i.e. distinguished vascular growth suggesting angiogenesis of a strong performance which may develop at any age but are mostly seen in adolescents and young adults. The current study showed no radiographical sign of bone resorption associated with lesion growth [14-20].
Recommendation
Study of larger sample size and multi-centric involvement to ensure more dependable results.
References
- Jensen JL, Barr RJ. Lesions of the facial skin. Differential diagnosis of Oral and Maxillofacial Lesions. 5th Edn. St Louis, MO: Mosby 1997: 549–550.
- Al-Mohaya MA, Al-Malik AM. Excision of oral pyogenic granuloma in a diabetic patient with 940nm diode laser. Saudi Med J 2016; 37:1395-400.
- Rai S, Kaur M, Bhatnagar P. Laser: A powerful tool for treatment of pyogenic granuloma. J Cutan Aesthet Surg 2011; 4:144-147.
- Neville BW, Damm DD, Allen CM, et al. Oral and maxillofacial pathology. Elsevier Health Sciences 2015.
- Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. PMPH-USA; 2001.
- Asnaashari M, Bigom-Taheri J, Mehdipoor M, et al. Posthaste outgrow of lip pyogenic granuloma after diode laser removal. J Lasers Med Sci 2014; 5:92.
- Aldelaimi A, Aldelaimi TN, Al-Gburi SM. Using of diode laser (940 nm) in orofacial region. J Res Med Dent Sci 2017; 5:34-39.
- Adusumilli S, Yalamanchili PS, Manthena S. Pyogenic granuloma near the midline of the oral cavity: A series of case reports. J Indian Society Periodontol 2014; 18:236.
- Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci 2006; 48:167-175.
- Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: A retrospective analysis of 108 cases. J Oral Maxillofac Surg 2003; 61:1285-1288.
- Gordon- Nunez MA, de Vasconcelos Carvalho M, Benevenuto TG, et al. Oral pyogenic granuloma; a retrospective analysis of 293 cases in a Brazillian population. J Oral Maxillofac Surg 2010; 68.
- Aldelaimi AA, Aldelaimi TN. Management of pyogenic granuloma (Clinicopathological Study). Indian J Forensic Med Toxicol 2021; 15:223.
- LaftaAbdulla W, Kadim NM, Abd ST. Assessment of pyogenic granuloma of the gingiva in Iraqi patient. Indian J Public Health 2020; 11:299.
- Newadkar UR, Khairnar S, Dodamani A. Pyogenic granuloma: A clinicopathological analysis of fifty cases. J Oral Res Rev 2018; 10:7.
- Ali K, Chatha MR, Rashid N, Raja M. Pyogenic granuloma–review. Pak Oral Dent J. 2006; 26:59-61.
- Marla V, Shrestha A, Goel K, et al. The histopathological spectrum of pyogenic granuloma: A Case Series. Case Rep Dent 2016; 2016:ID1323798.
- Papageorge MB, Doku HC. An exaggerated response of intraoral pyogenic granuloma during puberty. J Clin Pediatr Dent 1992; 16:213-216.
- Rosa C, Cartagena A, Torre A. Oral pyogenic granuloma diagnosis and treatment: A series of cases. Rev Odontol Mex 2017; 21:244-52.
- Aldelaimi TN, Khalil AA. Clinical application of diode laser (980 nm) in maxillofacial surgical procedures. J Craniofac Surg 2015; 26:1220–1223.
- Aldelaimi AA, Enezei HH, Aldelaimi TN, et al. Tumors of craniofacial region in Iraq (Clinicopathological Study). J Res Med Dent Sci 2021; 9:66-71.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Biomedical Application, Laser Institute for Postgraduate Studies, University of Baghdad, Iraq1Department of Maxillofacial Surgery, College of Dentistry, University of Anbar, Iraq
Citation: Aya A Majeed, Tahrir N Aldelaimi, Treatment of Pyogenic Granuloma with Diode Laser, J Res Med Dent Sci, 2022, 10 (4):52-56.
Received: 07-Mar-2022, Manuscript No. JRMDS-22-48333; , Pre QC No. JRMDS-22-48333 (PQ); Editor assigned: 09-Mar-2022, Pre QC No. JRMDS-22-48333 (PQ); Reviewed: 23-Mar-2022, QC No. JRMDS-22-48333; Revised: 28-Mar-2022, Manuscript No. JRMDS-22-48333 (R); Published: 04-Apr-2022
