Research - (2021) Volume 9, Issue 8
Validity the Role of T Scan Occlusion and PRP Combined with Hyaluronic Acid Injection as Complimentary Therapy in the Treatment of TMJ Diseases after Diagnosis by CBCT
Shefaa H Alnuamy1, Sameerah Jameel Tarfa2*, Azhar Ammash Hussein3 and Raad MuhiAldeen Helmi1
*Correspondence: Sameerah Jameel Tarfa, College of Dentistry, University of Thi-Qar, Iraq, Email:
Abstract
The causes factors of temporomandibular joint disorders (TMD) are multifactorial, whereas occlusal disharmony is one of the predisposing factors. Researchers still discuss the relation between occlusion and TMD, TMJDs complementary between muscle of mastication dysfunction and occlusal disharmony, CBCT is one of preferable device in diagnosis TMJ diseases patient not resolved by T scan system occlusion can be treated with injectable PRP and hyaluronic acid to improve function.
Keywords
Tempromandibularjoint disorder, CBCT diagnosis, T Scan, PRP combined with Hyaluronic acid, improving criteria
Introduction
Around 75% of adults have at least one TMD symptom, and 30% have two or more [1]. Patients often report discomfort while opening and chewing their mouths, as well as crepitation, clicking in the temporomandibular joint or ear, minimal mandibular opening, morning stagnation, and sleep disorders [2,3]. Since it is difficult to identify a single main reason for the etiology of the disorder is polyetiological. However, various researchers in the dental community disagree about the connection between dental occlusion and TMDs, and morphological disorders in the temporomandibular joint are not always a result of occlusal disorders. The posterior teeth should be in contact at the same time, distributing force evenly around the dental arch [4]. When the mandibular condyle is positioned in the mandibular fossa, slightly (0.5 mm) glided forward as well as backward from the apex of its front location, at the base of the temporal bone's articular tubercle, the most stable central occlusion occurs [5]. Internal joint space derangement, bone alterations, and degenerative pathologies are all symptoms of temporomandibular joint disorders (TMDs). TMDs are characterized by pain, joint noise, limited range of motion, weakened jaw control, deviations or displacements when opening and closing the mouth, and open locking [6,7].
For the first time in CBCT, we will now see both pathology and anatomy in high- resolution thin-slice grayscale images and 3-D color reconstructed views.
Internal temporomandibular joint (TMJ) derangements include disc displacements, with or without reduction, which are often responsible for TMJ joint sounds, pain, and irritation. Joint displacements are usually caused by the structure and occlusal force of the masticatory system [1], but they may also be caused by other factors [2]. Moreover, age, dentition, and masticatory muscle patterns can all play a role in the development or maintenance of temporomandibular joint dislocations [3]. When a disc moves out of its natural location in the joint spaces, it is called a disc displacement. The posterior band should be at 12 o'clock and the intermediate zone should be at 10 o'clock in the usual disc location. The disc is shaped like a bow tie, with a thin middle zone that has the shortest inter-bony width. Displacement of the disc may occur in either direction, but the most common is anterior disc displacement. The posterior band of the disc was anterior to the condylar head in dislocation with reduction, but with a natural disc– condyle relationship when the mouth was opened by 1 inch. The posterior band was located anteriorly to the condyle in non-reducing displacement both with the mouth closed and open 1 inch [8].
Disc displacement with or without TMJ reduction is an intracapsular dysfunction that contributes to disc and articular surface degeneration [9].
Osteoarthritis (OA) of the TMJ causes pain, stiffness, and loss of function due to degenerative changes in bone, cartilage, and supporting tissues [10]. It has a degenerative trend that leads to bone erosion, sclerosis, and bony alterations such as osteophytes and flattening of the condyle surface. It is more common in females than males [11]. Limitations in motion occur in the majority of cases, and patients are unable to chew efficiently or reach a natural mouth opening without discomfort. All these signs detected by CBCT [12].
Additional details about occlusion time, the origin of the occlusal force, and the distribution of pressures on both sides of the mandible can be obtained using digital analysis. Using the T-Scan analysis system, some authors claim that occlusion time is linked to premature contacts and occlusion instability [10,12].
Even though literature suggests that arthrocentesis alone can achieve these results [10,13], further research is needed to better understand the effectiveness of different techniques for performing arthrocentesis using growing factors, autologous solutions, or alternative materials; the most used materials are platelet-rich plasma (PRP) and hyaluronic acid (HA) Platelets are separated from other blood components after centrifuging heparinized whole autologous blood for 15 minutes. To achieve the desired concentration, the platelets are dissolved with a tube containing hyloronic acid solution. This is a new type of regenerative therapy for injuries in the orthopaedical region, with promising anti-inflammatory, analgesic, and antibacterial properties [4,5,14].
PRP is also being proposed for use as a biological adjuvant medication in the treatment of Orth. It also enhances chondrocyte glycosaminoglycan synthesis, balances joint angiogenesis, and serves as a scaffold for stem cell migration by restoring intra-articular hyaluronic acid. According to basic science research, PRP stimulates cell proliferation and cartilage matrix growth in chondrocytes and bone marrow-derived mesenchymal stromal cells and enhances hyaluronic acid synthesis in synoviocytes [15].
PRP include: connective tissue growth factor, epidermal growth factor vascular endothelial growth factor, insulinlike growth factor 2, Interleukin 8, keratinocyte factor, platelet-derive growth factor .
Serotonin is a chemical found in the pineal gland, the digestive tract, the central nervous system, and blood platelets. It is also known as 5-hydroxytryptamine. A hormone is a natural material produced by our bodies that influences and controls the function of specific cells and organs [16,17]. HA is a high-molecular-weight glycosaminoglycan present in synovial fluid that helps in joint lubrication. HA injections have long been used to treat TMDs, either as a single dose or in conjunction with other treatments such as arthrocentesis or arthroscopy, and several published trials have shown positive and supportive outcomes in terms of increased mouth opening and pain relief [6,18,19].
Materials and Methods
All 50 volunteer patients in 2019- 2020 suffering pain in TMJ during clinical examination, they are all diagnosed, and treated in AL-Israa dental college using digital T scan (Teck-scan Novus) analysis. They have been examined by using centric occlusal force with T Scan and CBCT (planmeca Romexes version 42).
Patients with TMJ pain are diagnosed using CBCT imaging, some of them have osteoarthritic changes, which can be easily identified using CBCT imaging. An alternative method used in case of a failed T scan analysis are treated with PRP combined with hyaluronic acid with special tube injected in TMJ space.
Results
Our study examine 50 volunteer patients with different age ranged from 10-59 groups as in Table 1 and Figure 1, all patient complain pain in temporomandibular joints as in Table 2 and Figure 2 42/complain pain only ,16/ complain pain and sound ,12/complain pain +limitation in mouth opning,30/complain pain + limitation in mouth opening and sound, all 50 patients examine in planmeca Romexes CBCT as in Table 3 and Figure 3 and radiological examine find 41.67 they are normal patients 16.67/with disc displacement according to 12 o’clock angle 12.5/ are with osteolytic lesion, 12.5/with flattening in head of coronoid and 16.67/ with dislocation in TMJ and this diagnosis appear significant in p value 0.022than all patients examine by T scan in centric occlusion this relationship in which the condyles articulate with thinnest avascular portion of their respected disc and the force of their bite appear 16/ are with force in anterior segment more ,48/ in left side force and in premolar area 26/in right side, 10/force in both side equally , and P value appear in this study highly significant as in Table 4 and Figure 4, Table 5 and Figures 5 and Figure 6 show the patients that not recovery with T scan adjusting occlusion which are 24 patient and 26 patient are improved by T scan occlusal adjusting , the patients not improved by T scan they treated by PRP with HA combination with special needle taken 2cc of PRP mixed with HU and injected in space of glenoid fossa at point 2mm inferior to the triangle canthal line with 27gauge needle ,1ml of PRP with HA was injected, 17 patient which are 62.5/ are improved after one injection in TMJ space they , improved according to the following criteria :the level of pain that is little or diminished ,the range of mouth opening 30mm with good motion, sound disappear with improved mastication and occlusion patient with unsuccessful in 1st injection after give other injection after one month interval give three injection, one every month 29.17/ they improved ,two patients only give them three injection every two months after six months they improved according to clinical criteria and sound disappear.as in Table 5 and Figure 5 and this Type of treatment give 0.048 in P-value which is highly significant.
| Age | No. | % | P-value |
|---|---|---|---|
| 10-19 | 12 | 24 | 0.001 (P<0.05 Sig) |
| 20-29 | 12 | 24 | |
| 30-39 | 6 | 12 | |
| 40-49 | 9 | 18 | |
| 50-59 | 11 | 22 | |
| Total | 50 | 100 |
Table 1: No. of patient according age group.
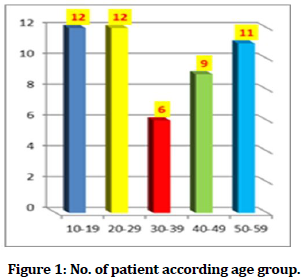
Figure 1. No. of patient according age group.
| Clinical Finding | No. | % | P-value |
|---|---|---|---|
| Pain only | 21 | 42 | 0.036 (P<0.05 Sig) |
| Pain +sound | 8 | 16 | |
| Pain + Limitation in mouth opinion | 6 | 12 | |
| pain +limitation +sound | 15 | 30 | |
| Total | 50 | 100 |
Table 2: No. of patient at all 50.TMJ problem with clinical finding.
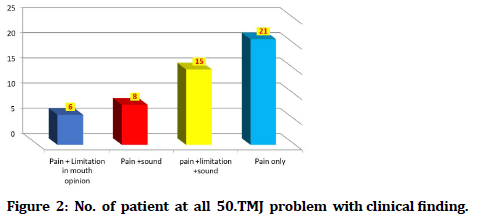
Figure 2. No. of patient at all 50.TMJ problem with clinical finding.
| No. | % | P-value | |
| Normal radiology | 10 | 41.67 | 0.022 (P<0.05 Sig) |
| Disc displacement according to 12 o’clock angle | 4 | 16.67 | |
| Osteophyte and osteolytic in TMJ | 3 | 12.5 | |
| Flattening in head of coronoid | 3 | 12.5 | |
| Dislocation | 4 | 16.67 | |
| Total | 24 | 100 |
Table 3: Radio graphical finding of TMJ in CBCT (24) patient (open and closed).
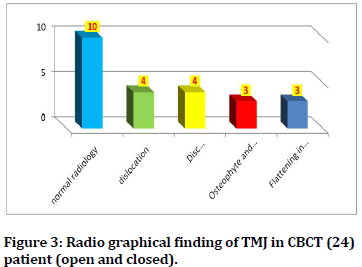
Figure 3. Radio graphical finding of TMJ in CBCT (24) patient (open and closed).
| More percentage force | No. | % | Adjusting the occlusion | P-value |
|---|---|---|---|---|
| Force in anterior teeth | 8 | 16 | 7 | 0.017 (P<0.05 Sig) |
| Force in left side more in premolar area | 24 | 48 | 9 | |
| Force in Right side in molar area | 13 | 26 | 6 | |
| Force in both side area | 5 | 10 | 4 | |
| Total | 50 | 100 | 26 |
Table 4: No. of patient diagnosis by T-Scan at centric occlusion and later adjusting the occlusion for improvement.
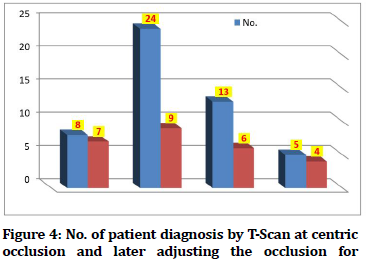
Figure 4. No. of patient diagnosis by T-Scan at centric occlusion and later adjusting the occlusion for improvement.
| Time intervals at months | No. injection | Improvement | % | P-value |
|---|---|---|---|---|
| 3-6 Months | 3 | 2 | 8.333 | 0.048 (P<0.05 S) |
| 3rd Month | 3 | 7 | 29.17 | |
| 1 month | 1 | 15 | 62.5 | |
| Total | 7 | 24 | 100 |
Table 5: PRP+HA according to No. of injection in TM.
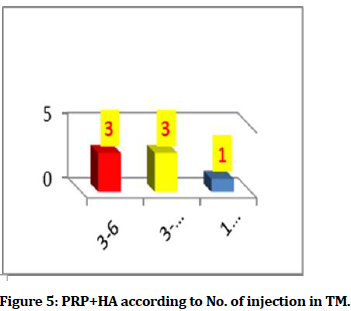
Figure 5. PRP+HA according to No. of injection in TM.
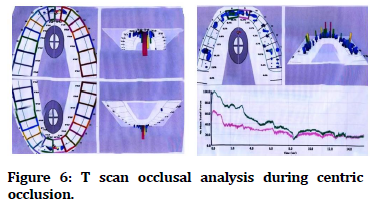
Figure 6. T scan occlusal analysis during centric occlusion.
Discussion
Our study was considering 26 / of patient improved after T scan, and 24 / are remain complain from TMJ problem after analysis and adjust in the occlusion according to T scan analysis as in Table 2 this agrees with Clin Diagn [2] The size, shape, and location of the teeth, the timing and sequence of eruption, the size of the dental arch, and the pattern of craniofacial development all influence dental occlusion [18].
Using injectable PRP with hyaluronic acid dysfunction is comparable to not treating patients with T scan. Various therapies for TMJ problems and disc displacement have been published in the literature and are used in clinical practice include, resting the jaw, disc repositioning done by HA with PRP TMJ in this study found its complementary and effective method, so it agrees with Mustafa [16].
The occlusal equilibrium is determined by the distance between the center of occlusal force, but this distance can also be affected by the function of the masticatory muscles [2]. In this analysis, the average value of the center of occlusal force was 1.5 ± 0.1mm. The average of patients with TMDs (4.39 ± 0.15 mm) was higher than our group subjects in Wang and Yin's study, but the differences were statistically important [2]. Based on previous research, patients with TMJs have a larger center of occlusion force than those who do not have TMJs (teeth cause); hence, occlusal imbalance is seen.
However, in our study, this disparity was not statistically important.
The disparity in occlusal force between the right and left sides is reflected in Iraqi citizens of our volunteer by the left side asymmetry index of maximum occlusal force being higher than the right side in molar area but higher in premolar area. In this analysis, there were statistically significant variations between the Iraqi patients. Patients complain of TMDs, which cause masticatory muscle action on one or both sides and can lead to temporomandibular joint disorders [19].
Even though the average values of these complex occlusion parameters were different, there was no statistically significant difference between the classes of the study sample. We can speculate that this was due to the limited sample size, the variety of patients' problems and clinical effects, and the seriousness of the disorders.
In 16% of the patients, clicking was noted as a symptom. It should also be noted that temporomandibular joint pain is associated with a functional imbalance of the stomatognathic system, changes in the movements of the lower mandible, and the emergence of muscular hypoactivity, resulting in a reduction in chewing force and pressure [8]. As a result, occlusal forces are distributed unevenly on both dental arches during occlusion, resulting in an imbalance in force concentrations on one side of the mandible compared to the other. The relationship movements of the lower mandible and decide the role of the mandibular condyle in the articulatory structures during exercise and at rest were studied by overseas authors, and it has been found that more people use the left side than the right side. As a result, occlusion is only just one of the options for patients with TMDs, and occlusion [1,2,8] does not consider the patients' complaints. There have not been any studies like this.
To review the findings of this research, we can claim that changes in occlusal parameters in the centric occlusion are typical of temporomandibular joint disorders patients. In the human articulatory system, not only occlusal and articulatory surfaces, but also masticatory muscles that control predisposing factors in the etiology of TMDs, play an important role. The distance between the centre of occlusal force, the asymmetry index of maximum occlusal force, and patients' discomfort in the temporomandibular joint region were all statistically important. Other statistically relevant variations between complainants and other topics have not been found, however crepitation in the joint region and reversible articulatory disk dislocation have been recorded the most frequently. These findings imply that there is a connection between patients' complaints and static occlusion parameters. This research discovered. While everyone's reaction to medication is different, most patients would need three sets of injections. Each series of treatments were spread out by about four weeks. There is a limit on the number of therapies in this study; only seven participants will need PRP for HA injections. Our study found 37 / they improved by more than one injection and 62/ done one time and patients improved in this study agree with Ayman [1].
Improvements in mouth opening and pain relief during mandibular motion with subsequent enhancement during T scan adjustment and HA with PRP injection are the treatment outcomes of TMJ arthrocentesis. The asymmetry index of maximal occlusal force and occlusion time was higher in patients with temporomandibular joint disorders than in healthy subjects, but the variations were not statistically significant. Patients' pain in the temporomandibular joint zone, the distance between the center of occlusal force, and the asymmetry index of maximal occlusal force were all statistically significant. Premolar and anterior occlusion have also been shown to have statistically significant differences between complainants and non-complainants, but crepitation in the joint area and reversible articulatory disk dislocation have been reported as the most common. These findings point to a connection between static occlusion parameters and patients' complaints. Additional research with larger samples is required to validate the results of this analysis [10,12].
Conclusion
This study shows that T scan digital occlusion first and PRP combined with hyaluronic acid are more effective method in dissolving most problems in temporomandibular joint after diagnosis by CBCT.
References
- Hegab AF, Ali HE, Elmasry M, et al. Platelet-rich plasma injection as an effective treatment for temporomandibular joint osteoarthritis. J Oral Maxillofac Surg 2015; 73:1706-13.
- Wang C, Yin X. Occlusal risk factors associated with temporomandibular disorders in young adults with normal occlusions. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114:419-23.
- Koos B, Godt A, Schille C, et al. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch. J Orofac Orthop 2010; 71:403-10.
- Baldini A, Nota A, Cozza P. The association between occlusion time and temporomandibular disorders. J Electromyography Kinesiol 2015; 25:15-154.
- Carlsson GE. Critical review of some dogmas in prosthodontics. J Prosthodontic Res 2009; 53:3-10.
- Dzingutė A, Pileičikienė G, Baltrušaitytė A, et al. Evaluation of the relationship between the occlusion parameters and symptoms of the temporomandibular joint disorder. Acta Med Lituanica 2017; 24:167.
- Haralur SB. Digital evaluation of functional occlusion parameters and their association with temporomandibular disorders. J Clin Diagnostic Res 2013; 7:1772.
- Sierpinska T, Kuc J, Golebiewska M. Assessment of masticatory muscle activity and occlusion time in patients with advanced tooth wear. Archives of oral biology. 2015 Sep 1;60(9):1346-55.
- Patyk A, Lotzmann U, Scherer C, et al. Comparative analytic occlusal study of clinical use of T-scan systems. ZWR 1989 ;98:752-5 .
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations if the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 2014; 28:6-27 .
- Hansdottir R, Bakke M. Joint tenderness jaw opening chewing velocity and bite force in patients with temporomandibular joint pain and matches control subjects. J Oral Facial Pain 2004; 18:108-13.
- Krishnamoorthy B, Mamatha NS, Kumar VA. TMJ imaging by CBCT: Current scenario. Annals Maxillofac Surg 2013; 3:80.
- Schnabl D, Rottler AK, Schupp W, et al. CBCT and MRT imaging in patients clinically diagnosed with temporomandibular joint arthralgia. Heliyon 2018; 4:e00641.
- Luther F. TMD and occlusion part II. Damned if we don't Functional occlusal problems: TMD epidemiology in a wider context. Br Dent J 2007; 202:38-9.
- Huang YF, Jung CL, Yang HW, et al. Clinical effectiveness of laser acupuncture in the treatment of temporomandibular joint disorder. J Form's Med Assoc 2014; 113:535-39.
- Hancı M, Karamese M, Tosun Z, et al. Intra-articular platelet-rich plasma injection for the treatment of temporomandibular disorders and a comparison with arthrocentesis. J Cranio-Maxillofac Surg 2015; 43:162-166.
- Alstergren P, Ernberg M, Kopp S, et al. TMJ Pain in relation to circulating neuropeptide Y, serotonin, and Interleukin-1 in rheumatoid arthritis. J Orofacial Pain 1999; 13:49-55.
- Haralur SB. Digital evaluation of functional occlusion parameters and their association with temporomandibular disorders. J Clin Diagn Res 2013; 7:1772-75.
- Agbaje JO, Van de Casteele E, Salem AS, et al. Assessment of occlusion with the T-Scan system in patients undergoing orthognathic surgery. Scientific Reports 2017; 7:1-8.
Author Info
Shefaa H Alnuamy1, Sameerah Jameel Tarfa2*, Azhar Ammash Hussein3 and Raad MuhiAldeen Helmi1
1College Of Dentistry, AL-Israa university college, Iraq2College of Dentistry, University of Thi-Qar, Iraq
3College of Dentistry, University of Tikrit, Iraq
Citation: Shefaa H Alnuamy, Sameerah Jameel Tarfa, Azhar Ammash Hussein, Raad MuhiAldeen Helmi,Validity the Role of T Scan Occlusion and PRP Combined with Hyaluronic Acid Injection as Complimentary Therapy in the Treatment of TMJ Diseases after Diagnosis by CBCT, J Res Med Dent Sci, 2021, 9(8): 280-285
Received: 14-Jun-2021 Accepted: 23-Aug-2021
