Research - (2021) Volume 9, Issue 4
A Clinical Study of Conduction Block in Acute Myocardial Infarction
D Arunprasath, C Ramakrishnan, E Dhandapani and NN Anand*
*Correspondence: NN Anand, Department of General Medicine, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
Objective: Acute myocardial infarction is a major health problem in both developing and developed countries, remaining as a leading cause of morbidity and mortatility. It can occurs at any level of the conduction system i.e. atrioventricular or interventricular. It may be transient or permanent.
Materials and Methods: 100 patients admitted in cardiac intensive care unit of sree balaji medical college and hospitals with the evidence of acute myocardial infarction are be studied. Results: 11% of the study populations developed heart failure whereas 89% were without evidence of heart failure. 19% of the study populations developed conduction blocks. In this 19% ,7 cases were first degree AV block, 4 cases of second degree AV block, 3 cases of complete heart block, 2 cases of left anterior hemi block, 2 cases of RBBB and one case of LBBB.
Conclusions: AV blocks were more common in inferior wall myocardial infarction. Bundle branch blocks were more common in anterior wall myocardial infarction. Association between mortality and conduction blocks were not done as our study did not had any mortality with conduction blocks.
Keywords
Ischaemia, Mycordium, Catecholamines, Hypoxia
Introduction
Acute myocardial infarction is a global epidemic and a major public problem due its leading cause of mortality and morbidity [1]. Myocardial infarction is usually resulting from an imbalance in oxygen supply and demand, which is often caused by plaque rupture with thrombus formation in an epicardial coronary artery which results in an acute reduction of supply to a portion of myocardium. Incidence of Acute MI is increasing nowadays with a male predominance when compared to females. In our country smoking is a common risk factor for the development of acute MI, now hypertension and diabetes, are also contributing as a major risk factor. The increased prevalence of stress and unhealthy lifestyle with earlier development of diabetes mellitus leads to the common cause of acute MI in the younger age groups [2,3]. Myocardial Infarction is considered as a part of a spectrum referred to as Acute Coronary Syndrome (ACS). The ACS continuum representing myocardial ischaemia or injury consists of Unstable Angina (USA), Non-ST Elevation MI (NSTEMI), ST Elevation MI (STEMI) [1]. Acute Myocardial Infarction is characterized by generalized autonomic dysfunction that results in enhanced automaticity of the myocardium and conduction system. Electrolyte imbalance and ongoing ischaemia which results in hypoxia of the conduction system further contribute to the development of conduction blocks and cardiac arrhythmias.
Various types of conduction blocks develop following an acute MI. Heart Blocks such as atrioventricular and interventricular blocks are among the most important electrical disturbances which occur following acute myocardial infarction. Delayed conduction may occur because of physiological phenomenon i.e increased vagal tone or pathological process with varying incidence rates in different populations.
The damaged myocardium results changes in tissue refractoriness. Enhanced efferent sympathetic activity, increased concentrations of circulating catecholamines and local release of catecholamines from nerve endings in the heart muscles results in development of various conduction block and development of arrhythmias [4,5].
The presence of conduction defects complicating acute MI is relatively frequent and it is associated with increased short term mortality rates. Bundle branch blocks in AMI caries poor prognosis. This is attributed both to the extent of myocardial damage and to the frequency of ventricular asystole. Development of conduction blocks worsens the outcome of AMI [6]. Thrombolytic therapy and early perfusion of the myocardium by PCI has been established to reduce the mortality in AMI. The incidence of high degree AV blocks has been reported to be as high as 20% in several studies with an association with increased shortterm mortality. The prognostic significance and management of these disturbances may vary with the location of the infarction, type of conduction blocks, associated clinical features and the hemodynamic compromise [7,8].
Materials and Methods
Study design
Prospective study.
Study population
100 patients admitted with acute myocardial infarction within 7 days of index event in Sree Balaji Medical College and Hospital CCU from February 2015 to September 2016.
Name
Age
Gender
Past illness-Diabetes Mellitus, Hypertension, Dyslipidemia, Old MI, Arrhythmia, ICD-intra cardiac device, CABG, Valvular Heart Disease, old evidence of conduction blocks, Drug history
Pregnancy
Troponin I/T
Inclusion criteria
Patients of acute myocardial infarction admitted in sree balaji medical college CCU.
Diagnosis of acute myocardial infarction based on ECG, Chest pain, Cardiac markers.
Diagnosis of conduction blocks based on ECG.
Exclusion criteria
Severe valvular heart disease.
Pregnancy.
Previously known case of conduction defects.
Patients on drugs, which may cause conduction defects like beta blockers, digoxin, calcium channel blockers.
Patients with renal failure (stage 3,4).
Hypokalemia and Hyperkalemia.
Unwilling patients.
History of cardiac valve replacement.
Coronary bypass graft patients.
Methodology
After ethical clearance, permissions were obtained from Head of the department of General medicine and Cardiology, respectively. After satisfying the exclusion criteria, inclusion criteria and informed consent, the structured proforma filled with respective data were collected.
Hundred’s patients admitted in Sree Balaji Medical College and Hospital CCU with the diagnosis of Acute MI are to be studied. All of them need electrocardiographic evidence of infarction in case of STEMI. They also need clinical features with ECG evidence of infarction and positive cardiac troponin I or T at any time during the index admission in case of NSTEMI. The diagnosis was established by the presence of typical angina pain lasting at least 30 minutes, ST segment elevation or depression >1 mm in two or more consecutive leads, and an increase in CKMB of double the normal values (190 U/L).
Results
Distribution according to age and gender
Out of 100 patients, 27 belongs to the age group between 60-69 years. Major proportion of the study group was between 40 to 79 years (91%) (Table 1). 69% of the study population was males and 31 % were females (Figure 1).
| Age | Count | Percent |
|---|---|---|
| <40 | 4 | 4 |
| 40-49 | 15 | 15 |
| 50-59 | 39 | 39 |
| 60-69 | 27 | 27 |
| 70-79 | 10 | 10 |
| 80-89 | 3 | 3 |
| 90-99 | 2 | 2 |
Table 1: Distribution according to age.
Figure 1. Distribution according to gender.
Distribution according to comorbidities
52% of the study population were hypertensive and 69% were diabetic - type 2, 37%, 37% were dyslipidemias and 27% had a history of myocardial infarction. 15% of the study population underwent PCI and 2% underwent CABG in the past (Table 2). 27% of the study population were having both diabetes and hypertension, 26% of the study population were having both diabetes and dyslipidemia and 22 % of the study population were having all the three (Figure 2).
| Comorbidities | Count | Percent |
|---|---|---|
| HTN | 52 | 52 |
| DM | 69 | 69 |
| DLP | 37 | 37 |
| PCI | 15 | 15 |
| CABG | 1 | 1 |
| OLD MI | 27 | 27 |
Table 2: Distribution according to comorbidities.
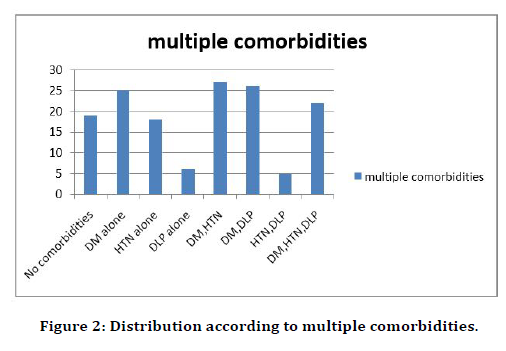
Figure 2. Distribution according to multiple comorbidities.
Distribution according to valvular heart disease
21% of the study population had valvular heart diseases whereas 79 % were free of valvular heart diseases (Table 3).
| VHD | Count | Percent |
|---|---|---|
| Yes | 21 | 21 |
| No | 79 | 79 |
Table 3: Distribution according to valvular heart disease.
Distribution According to cardiac markers
96% of the study population were positive for cardiac markers and 4% were cardiac markers negative (Figure 3).
Figure 3. Distribution According to cardiac markers.
Total summary
Out of 21 patients of valvular heart disease 10 patients developed AV block and 3 patients developed interventricular blocks. Out of 79 patients with no valvular heart disease, 4 patients developed AV block and 2 patients developed interventricular block (Figure 4).
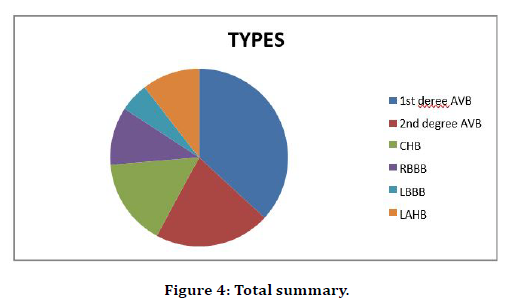
Figure 4. Total summary.
Discussion
Among 100 patients enrolled in this study with both male and female gender and age group from 40 years to 90 years. The most common age group for MI is ranging from 50 to 70 years (39 cases in the age group of 50 -59 years and 27 cases in the age group of 60-69 years) followed by 40 to 49 years (15 cases). similar findings were observed in Charvda et al. [9,10]. The male gender is more susceptible than the female gender. Incidence of MI in male were common in the age group of 45 to 55 years and incidence of MI in females were common in the age group of 55 to 65 years. Males are significantly younger than females in this study in developing MI and this due to more prevalence of risk factors such as hypertension, smoking and diabetes mellitus among males in this study. This finding is similar with Bangalore et al [9-11], Khan S et al study and several other local studies.
Risk factors such as hypertension were present in 18% of cases, diabetes in 25% of the cases, smoking in 29% of the cases. A similar finding was observed in Charvda et al. where smoking is the most common risk factors followed by diabetes mellitus. The prevalence of DM and HTN in the study by Hrey et al. was 22.3% and 20.2% respectively. While comparing the risk factors between males and females, smoking, hypertension, diabetes, dyslipidemaia are where common in males and diabetes and dyslipidemia were common in females [12]. In our study, Inferior Wall MI is the most common site of MI followed by AWMI. This finding was supported by Hrey be and Saba and shah et al. In our study, out of 100 patients with MI,19% had conduction block. Out of this 19% 14% were developed AV block and 5% developed Interventricular block. Out of this 14% with AV block,7% developed first degree AV block and 4% developed 2nd degree AV block and 3% cases developed complete heart block. Out of this 5% with Interventricular block 2 cases of RBBB and 2 cases of LAHB and 1 case of LBBB were seen. Similar findings were seen in Bhalli et al. Archbold et al. and Shirafkan et al. [6,10,13,14]. Male’s patients with AMI developed more conduction blocks than the females with AMI in this study and this was supported by Escosteguy et al study. In our Atrioventricular blocks are more common in Acute IWMI and Interventricular blocks are more common in Acute AWMI and this association was statistically significant (p<0.001) and consistent with an earlier study.
Our study data and results in this respect very closely like the findings of Escosteguy et al. who studied 929 cases of AMI in Brazil and found significant association of AV Blocks and BBB with inferior and anterior wall MI respectively.[15] In patients with AWMI our findings in relation interventricular blocks are also compatible with other studies. Interventricular blocks are common in AWMI then IWMI and in patients with IWMI AV Blocks are more common than in AWMI. First degree AVB is more common in isolated IWMI and with RVMI whereas 3 rd degree AVB is more common in IWMI combined with RVMI.
Conclusion
In our study there is no mortality seen in patients with conduction blocks with AMI since interventions were done earlier soon after developing conduction blocks, if left untreated AMI with conduction blocks will results in significant mortality when compared to AMI without conduction blocks which was supported by several studies. so earlier diagnosis and prompt intervention will reduce the mortality rates in AMI with conduction blocks.
Funding
No funding sources.
Ethical Approval
The study was approved by the institutional ethics committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Antman EM, Braun Wald E Braunwald. Heart disease. A textbook of cardiovascular medicine. 6th Edn. Philadelphia; WB Saunders 2001.
- Rissam HS, Kishore S, Trehan N. Coronary artery disease in young Indian-The missing link. JIACM 2001; 2:128-132.
- Fabijanic D, Culic V, Bozic I, et al. Gender difference in in-hospital mortality and mechanisms of death after the first acute myocardial infarction. Ann Saudi Med 2006; 26:455-460.
- Davies MJ, Redwood D, Harris A. Heart block and coronary artery disease. Br Med J 1967; 3:342-343.
- Janse MJ, Wit AL. Electrophysiological mechanisms arrthymias and conduction blocks resulting from myocardial ischaemia and infarction. Physiol Rev 1989; 69:1049-1049.
- Kramullah I, Iqbal MA , Hadi A, et al. Conduction disturbances in patients with acute anterior wall infarctions and outcomes. Pak Heart J 2014; 47:156-161.
- Bauer GE, Julian DG, Valentine PA. Bundle –branch block in acute myocardial infarction. Br Heart J 1965; 27:724-730.
- Uhley HN. Some controversy regarding peripheral distribution of the conduction system. Am J Cardiol 1972; 30:919-920.
- Hecht HH, Kossmann CE, Childers RW, et al. Atrioventricular and intraventricular conduction. Revised nomenclature and concepts. Am J Cardiol 1973; 31:232.
- Go AS, Barron HV, Rundle AC, et al. Bundle-branch block and in-hospital mortality in acute myocardial infarction. National registry of myocardial infarction 2 investigators. Ann Intern Med 1998; 129:690.
- Stenestrand U, Tabrizi F, Lindbäck J, et al. Comorbidity and myocardial dysfunction are the main explanations for the higher 1 -year mortality in acute myocardial infarction with left bundle-branch block. Circulation 2004; 110:1896.
- Lamas GA, Muller JE, Turi ZG, et al. A simplified method to predict occurrence of complete heart block during acute myocardial infarction. Am J Cardiol 1986; 57:1213.
- Meine TJ, Al-Khatib SM, Alexander JH, et al. Incidence, predictors, and outcomes of high-degree atrioventricular block complicating acute myocardial infarction treated with thrombolytic therapy. Am Heart J 2005; 149:670.
- Harpaz D, Behar S, Gottlieb S. Complete atrioventricular block complicating acute myocardial infarction in the thrombolytic era. J Am Coll Cardiol 1999; 34:1721-1728.
- Gomez JF, Zareba W, Moss AJ, et al. Prognostic value of location and type of myocardial infarction in the setting of advanced left ventricular dysfunction. Am J Cardiol 2007; 99:642 -646.
Author Info
D Arunprasath, C Ramakrishnan, E Dhandapani and NN Anand*
Department of General Medicine, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: D Arunprasath, C Ramakrishnan, E Dhandapani, NN Anand, A Clinical Study of Conduction Block in Acute Myocardial Infarction, J Res Med Dent Sci, 2021, 9 (4): 406-410.
Received: 20-Mar-2021 Accepted: 22-Apr-2021
